Chapter 71 VAGINAL HYSTERECTOMY IN THE TREATMENT OF VAGINAL PROLAPSE
Hysterectomy continues to be one of the most commonly performed surgical procedures in the United States, second only to cesarean section. Approximately 800,000 hysterectomies are performed annually in the United States.1 According to the National Center for Health Statistics, 3,525,237 hysterectomies were performed in the United States between 1994 and 1999, at a rate of 5.5 per 1000 women. The most common indication for hysterectomy continues to be uterine leiomyoma, accounting for approximately 38% of all hysterectomies. Endometriosis accounts for 18% of all hysterectomies, followed by uterine prolapse (16%) and endometrial hyperplasia (4%).1 As the population of women older than 65 years continues to rise, the practitioner can anticipate an increase in the number of women presenting with these indications.2 Most hysterectomies are performed by the abdominal route, with the rate of vaginal hysterectomy remaining stable over the past several decades.1 Vaginal hysterectomy in the appropriately selected patient has been reported to result in a shorter hospital stay, less operative blood loss, and less postoperative pain compared with the abdominal route of hysterectomy. Patients presenting for evaluation and surgical correction of pelvic organ prolapse are particularly appropriate candidates for vaginal hysterectomy.
ANATOMY OF PELVIC SUPPORT
Normal pelvic support is a complex interaction between the muscular and fascial structures that line the pelvic cavity, collectively known as the pelvic floor. The levator ani complex (i.e., coccygeus, iliococcygeus, and pubococcygeus) stretches from the coccyx to the symphysis pubis anteriorly in the erect woman. Laterally, the levator complex attaches to the arcus tendineus fasciae pelvis (“white line”). The arcus tendineus fasciae pelvis extends from the symphysis pubis to the ischial spines bilaterally. The levator ani complex is typically described in two parts: the diaphragmatic portion (i.e., coccygeus and iliococcygeus) and the pubovisceral portion (i.e., pubococcygeus). The coccygeus muscles run bilaterally from the sacrum and coccyx to the ischial spines and are associated with the sacrospinous ligaments. The iliococcygeus muscles pass laterally from the symphysis pubis to the arcus tendineus fasciae pelvis, where they attach and turn medially to join the coccygeus at the coccyx, forming the levator plate. The pubovisceral portion, or pubococcygeus, is associated with the puborectalis, arising from the posterior surface of the symphysis pubis and extending back to the ventral surface of the coccyx.3
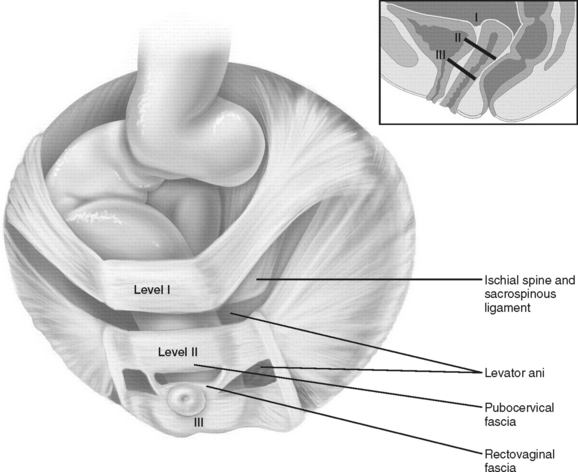
Normal pelvic support is provided by the pelvic floor and by the connective tissue attachments. The pelvic organs rest on the pelvic floor and are stabilized by the connective tissues. In 1992, DeLancey described the stabilization of the vagina in levels. Level 1 support is derived from the cardinal-uterosacral complex and is responsible for holding the upper vagina and cervix in a superior position in relation to the genital hiatus. Level II support is responsible for lateral support of the midvagina to the arcus tendineus fasciae pelvis. Level III support is responsible for distal support of the lower vagina by means of connections to the perineal body and perineal membrane4 (Fig. 71-1).
PELVIC ORGAN PROLAPSE
The cause of pelvic organ prolapse is multifactorial. Uterovaginal prolapse results from damage to the cardinal-uterosacral complex, or level I support.5 The uterus and upper vagina normally lie over the pelvic floor and are directed to the hollow of the sacrum. Increased intra-abdominal pressure is directed toward the levator ani complex. Attenuation of the levator ani complex may result in inadequate support to the overlying pelvic organs. Such attenuation may be the result of childbirth and some connective tissue disorders. Conditions or maneuvers that result in repeated increases in intra-abdominal pressure may lead to attenuation of the pelvic floor and aggravate pelvic organ prolapse. These conditions may include occupations that require heavy lifting or medical conditions such as chronic constipation resulting in excessive straining or chronic obstructive pulmonary disease with chronic coughing.
PELVIC ORGAN PROLAPSE
Diagnosis
Patients with uterovaginal prolapse may present with a multitude of symptoms. A carefully tailored history and physical examination are important in gaining insight into the complaint and any affect on the patient’s quality of life. Patients may present with a vaginal mass, sometimes described by them as a bulge. They may complain of pelvic pain, pressure, or dyspareunia. Patients may describe urinary urgency or frequency or incontinence. In cases of severe prolapse, patients may complain of urinary retention, because of the effect of the prolapse on the anatomy of the lower urinary tract. The typical patient describes symptoms that are worse with standing or activity and that improve on assuming a supine position. If the diagnosis of pelvic organ prolapse is obscure, it is important to consider performing the examination of the patient at the end of the day, when the prolapse is likely to be at its worst.
Physical Examination
The result of physical examination remains one of the most important pieces of information in the evaluation of pelvic organ prolapse. The diagnosis of uterovaginal prolapse is confirmed by significant descensus of the uterus on pelvic examination. A bimanual examination is important to ascertain the size and mobility of the uterus and any underlying pathology such as uterine leiomyoma or adnexal masses. The caliber of the genital hiatus is measured to predict the success of a vaginal hysterectomy. The coexistence of anterior or posterior vaginal wall prolapse should be determined. In our experience, it is advisable to evaluate the patient with uterovaginal prolapse in the supine and standing positions. The patient should be examined with an empty bladder because the prolapse may not be fully appreciated in the presence of a subjectively full bladder.6 It is important to evaluate for the sign of stress incontinence with the bladder full and the prolapse reduced to its normal anatomic location to exclude potential or occult stress incontinence.
Classification
The severity of pelvic organ prolapse is described to standardize findings among examiners. For decades, the Baden-Walker system was used to describe the presence of pelvic organ prolapse.7 The Baden-Walker system, still in use today, is also known as the halfway system. It involves description of the most dependent position of the pelvic organs during a maximum Valsalva maneuver or during standing in relation to the hymenal ring (Table 71-1).
Table 71-1 Baden-Walker Classification of Pelvic Organ Prolapse
| Cystocele | First degree: Anterior vaginal wall and bladder descend halfway to the hymen. |
| Second degree: Anterior vaginal wall and bladder descend to the hymenal ring. | |
| Third degree: Anterior vaginal wall and bladder are outside the hymen. | |
| Uterine or vaginal vault prolapse | First degree: Cervix or vaginal apex descends halfway to the hymen. |
| Second degree: Cervix or vaginal apex extends to the hymen or over the perineal body. | |
| Third degree: Cervix and uterine corpus extend beyond the hymen, or the vaginal vault is everted and protrudes beyond the hymen. | |
| Rectocele | First degree: Posterior vaginal wall descends halfway to the hymen. |
| Second degree: Posterior vaginal wall descends to the hymen. | |
| Third degree: Posterior vaginal wall extends beyond the hymen. | |
| Enterocele | Presence of the enterocele sac, relative to the hymen, should be described anatomically, with the patient in the supine and standing positions during a Valsalva maneuver. |
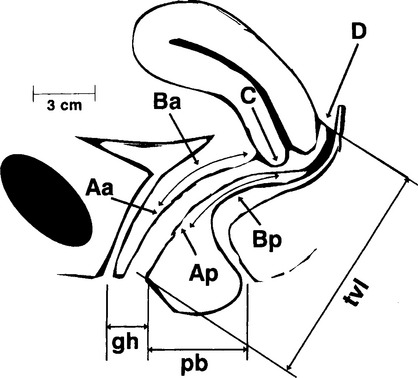
In 1996, Bump and colleagues8 standardized the terminology of female pelvic organ prolapse for the International Continence Society (ICS). The Pelvic Organ Prolapse Quantification (POP-Q) system involves measurement of six anatomic points (in centimeters) in relation to the hymenal ring, as well as the genital hiatus, perineal body, and total vaginal length. The hymenal ring, defined as zero, is chosen as the reference point because it is a fixed anatomic point from which interobserver variability can be standardized. Prolapse distal to the hymenal ring is described in positive centimeters from the hymenal ring. Prolapse proximal to the hymenal ring is defined in negative centimeters from the hymenal ring. The six anatomic points can be divided into two points on the anterior vaginal wall (Aa and Ba), two points on the posterior vaginal wall (Ap and Bp), and two points in the superior vagina (C and D) (Fig. 71-2).
The genital hiatus (gh) is measured from the posterior fourchette to the middle of the urethral meatus. The perineal body (pb) is measured from the posterior fourchette to the middle of the anus. Total vaginal length (tvl) is measured with point C and point D reduced to their normal anatomic positions.
Table 71-2 represents the stages of pelvic organ prolapse as defined by the POP-Q system. Because of the use of measurements revolving around fixed anatomic landmarks, the POP-Q system is a much more precise method of defining pelvic organ prolapse compared with previous systems. Interexaminer variability is markedly reduced, which is important for clinical standardization and for the purposes of research.
Table 71-2 Stages of Pelvic Organ Prolapse
| Stage 0 | No evidence of pelvic organ prolapse. Points Aa, Ba, Ap, and Bp are all defined at − 3 cm. Points C and D are located within 2 cm of the tvl (i.e., ≤ tvl − 2 cm). |
| Stage 1 | Most distal portion of the prolapse is > 1 cm above the level of the hymen (i.e., ≤ 1 cm). |
| Stage 2 | Most distal portion of the prolapse within 1 cm of the hymenal ring, proximal or distal (i.e., ≥ − 1 cm but ≤ +1 cm) |
| Stage 3 | Most distal portion of the prolapse is more than 1 cm distal to the hymenal ring but not more than 2 cm less than the tvl (i.e., > +1 cm but not more than tvl − 2 cm). |
| Stage 4 | Complete eversion of the tvl |
tvl, total vaginal length.
VAGINAL HYSTERECTOMY AND RELATED PROCEDURES
Indications
The most frequent indication for hysterectomy is the leiomyomatous uterus. Patients with uterine fibroids may complain of pelvic pain or pressure. Other patients may complain of low back pain or urinary symptoms. Dysfunctional uterine bleeding is a common complaint of the woman with uterine fibroids. The patient with symptomatic uterine fibroids is a safe candidate for vaginal hysterectomy assuming the uterus is mobile and the total uterine size is less than 12 weeks’ gestational size.9
Contraindications
With an appropriate understanding of pelvic anatomy, the experienced surgeon encounters few contraindications to the vaginal route of hysterectomy. Even the large fibroid uterus can be removed vaginally in the hands of a skilled surgeon. Uterine immobility can make a vaginal hysterectomy difficult if abdominopelvic adhesions or scarring are present. A narrow, or stenotic, vaginal introitus can complicate removal of the uterus vaginally, and consideration should be given to an abdominal approach in this case. Selected cases of endometriosis are a contraindication to the vaginal route of hysterectomy. In 1995, Kovac10 assigned 617 women to abdominal, vaginal, or laparoscopically assisted vaginal hysterectomy based on uterine size and risk factors suggesting pelvic disease. In his series, 548 women were able to undergo successful vaginal hysterectomy. In the case of laparoscopically assisted vaginal hysterectomy, all but 2 of the 63 cases could have undergone successful vaginal hysterectomy based on laparoscopic findings. In his series, Kovac reported a 99.5% success rate for the vaginal route of hysterectomy using the techniques of morcellation, bivalving, and uterine coring (discussed later).10 The suspicious adnexal mass and high-grade endometrial carcinoma present absolute contraindications to the urogynecologic surgeon. In some cases, low-grade endometrial carcinoma may be managed with a vaginal hysterectomy.