Chapter 69 USE OF A POSTERIOR SLING FOR VAGINAL VAULT PROLAPSE
HISTORY
The first posterior sling operation was performed in 1992. Initially, the operation was used only for repair of significant vaginal vault and uterine prolapse (i.e., restoration of structure). Over the past 12 years, it was found that coexisting symptoms of abnormal emptying, nocturia, pelvic pain, urge, and frequency—a group of symptoms now described as the posterior fornix syndrome1—also were being improved in approximately 80% of patients (i.e., restoration of function). Although the generic name for this procedure is infracoccygeal sacropexy,2 the operation is universally known as the posterior IVS or posterior sling operation.
RESTORATION OF STRUCTURE
Dynamic Structural Mechanism of the Uterus and Vaginal Vault
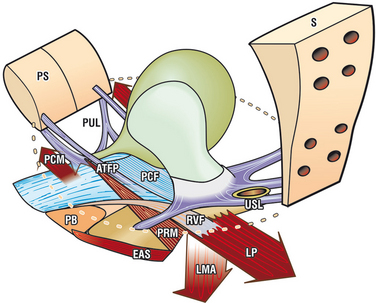
The uterus and vaginal vault are anchored passively by the suspensory ligaments, the uterosacral ligaments (USLs) and arcus tendineus fasciae pelvis (Fig. 69-1), and they are anchored actively by the three directional muscle forces that stretch the vagina against these ligaments.3,4 The USLs, the apical segment of the vagina, rectovaginal fascia, and perineal body (see Fig. 69-1) work synergistically as a subsystem,3 and repair of all three is often required.
Fibromuscular Supports of the Uterus and Vagina
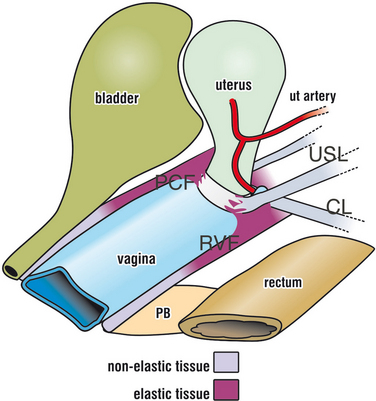
The inherent strength of the rectovaginal fascia and its backward stretching by the levator plate are major factors in preventing prolapse, which is really a form of intussusception (Fig. 69-2). The cervix is a key anchoring point for the pubocervical fascia anteriorly and the rectovaginal fascia posteriorly, and the anterior and posterior fascial supports may need repairing in a patient with uterine or vault prolapse.
Hysterectomy may weaken the fascial side wall support and weaken the USLs, perhaps by removing a major part of the blood supply. Conservation of the uterus may be important in preventing vaginal prolapse and incontinence.5
Vaginal Fascia as a Tensor of the Vagina
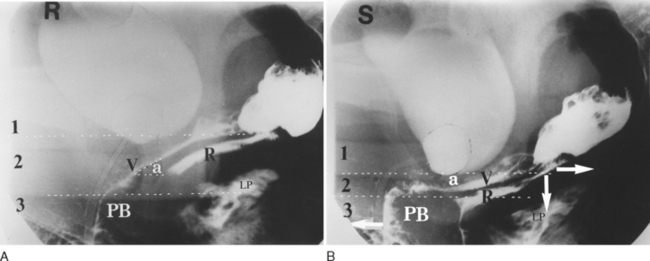
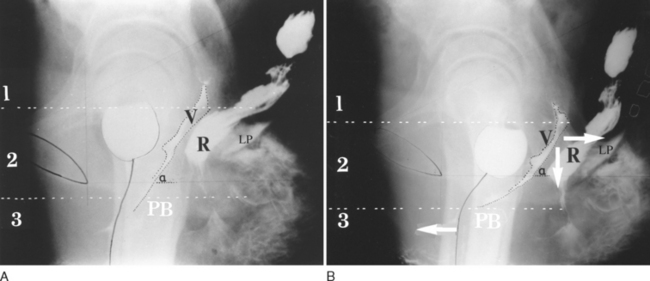
This concept, that vaginal fascia functions as a tensor of the vagina, was originally proposed by Sturmdorf in 1916,6 and it was confirmed by an observational radiologic study.7 During effort, the rectovaginal fascia was stretched backward against the perineal body and downward against the USLs to compress level 2 (Fig. 69-3). In contrast, there is no compression of level 2 in the multipara with damaged tissues (Fig. 69-4), even though the muscles appear to be contracting normally, as evidenced by downward angulation of the anterior part of levator plate and forward movement of the distal urethra.
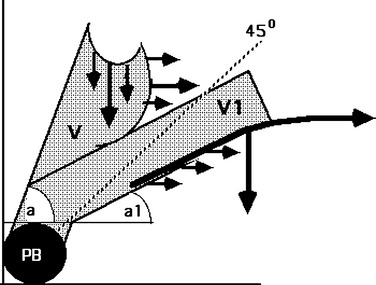
Compression of the vaginal canal appeared to be related to the angle “a” formed between the upper vagina and the horizontal at rest.7 When the angle was more than 45 degrees to the horizontal (Fig. 69-5), only 2 of 23 patients demonstrated angulation and compression of the vagina on straining, compared with 100% when the angle was less than 45 degrees to the horizontal (n = 27). If the vaginal fascia is lax, the stretching forces (see Fig. 69-5) may not be able to grip, and there is no angulation or compression (see Fig. 69-4B). The damaged vaginal tissues become vulnerable to the forces generated by the abdomen and pelvis (see Fig. 69-5) to create cystocele, rectocele, and enterocele.
A short vagina may prevent angulation and compression (see Fig. 69-5). The vagina is a cylinder. Excising vaginal tissue during surgery may shorten or narrow the vagina. It is possible to conclude the following from these findings:
CORRECTIVE SURGERY
The late David Nichols stated that vaginal vault prolapse is a significant longer-term complication in patients undergoing hy-sterectomy.8 Nichols emphasized the need for axial repair, conservation of vaginal form and function, and the requirement to repair coexisting cystoceles, rectoceles, and enteroceles. The biomechanical rationale for this is presented in Figure 69-5.
Posterior Sling Operation
With the posterior sling operation, the aim was to create an axial procedure for cure of uterine and vaginal vault prolapse using plastic tapes to create artificial collagenous neoligaments. It was reasoned that this approach would avoid the morbidity and complications associated with alternative techniques: nerve injury and dyspareunia with sacrospinous colpopexy, bleeding from sacral veins and peritoneal adhesions with abdominal sacropexy, and ureteric injury with the McCall culdoplasty.9
Posterior IVS Operation for Vaginal Vault Prolapse
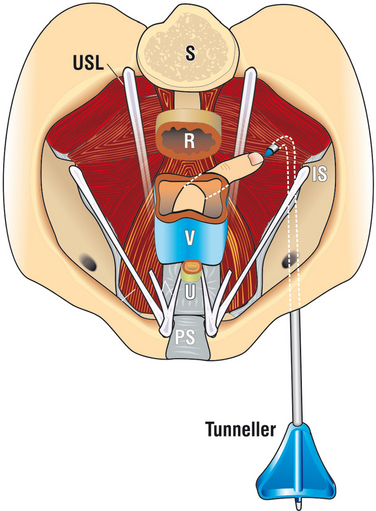
A more evolved technique than that originally described2 for the posterior IVS operation is presented. Posterior IVS (i.e., infracoccygeal sacropexy) reinforces the distal part of USLs and anchors the vaginal apex to the posterior muscles of the pelvic floor with a polypropylene tape. A full-thickness incision approximately 2.5 to 3 cm long is made in the posterior vaginal wall just below the hysterectomy scar line (Fig. 69-6). Using dissecting scissors with the tip pressed against the vaginal skin, a channel is made in the direction of the ischial spine sufficient to insert the index finger. The ischial spine is located, and the point of entry through the pelvic muscles for the IVS tunneler (Tyco) is determined. If an enterocoele is opened, it is ligated with a high purse-string suture.
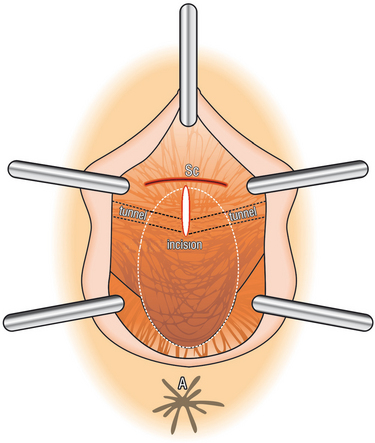
Figure 69-6 Vaginal incision, as viewed looking into the posterior vaginal wall. Sc, hysterectomy scar.
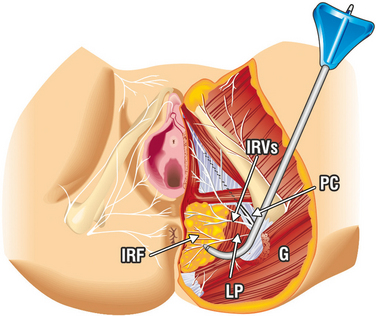
Bilateral skin incisions 0.5 cm long are made in the perianal skin at the 4- and 8-o’clock positions halfway between the coccyx and external anal sphincter in a line 2 cm lateral to the external border of the external anal sphincter (Fig. 69-7). The tunneler is pushed 3 to 4 cm into the ischiorectal fossa, keeping the plastic tip parallel to the floor (Fig. 69-8). The index finger is placed into the tunnel created in the vagina to locate the tip of the tunneler, which penetrates the levator muscles 1 cm medial and dorsal to the ischial spine (Fig. 69-9). At this point, the tunneler is safely sited well away from rectum and peritoneum.
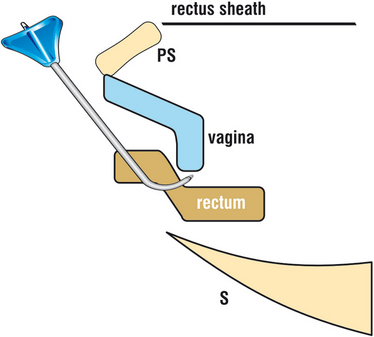
Figure 69-8 As the tunneler is inserted in a supine patient, it passes across the anterior wall of the rectum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree