Chapter 53 FUNCTIONAL ANATOMY AND PATHOPHYSIOLOGY OF PELVIC ORGAN PROLAPSE
Pelvic floor disorders, including pelvic organ prolapse and urinary incontinence, are debilitating conditions that result in surgery in one of nine women.1 In the United States, the National Center for Health Statistics estimates that 400,000 operations are performed for pelvic floor dysfunction each year, with 300,000 of these occurring in the inpatient setting.2,3 This is six to eight times more operations than radical prostatectomies performed each year. Although there is wide recognition of urinary incontinence, pelvic organ prolapse is responsible for twice as many operations, yet its causes are largely unknown. Prolapse arises because of injuries and deterioration of the muscles, nerves, and connective tissues that support and control normal pelvic function. This chapter addresses the functional anatomy of the pelvic floor in women and specifically focuses on how the pelvic organs are supported by the surrounding muscle and fasciae. It also con-siders the pathophysiology of pelvic organ prolapse as it relates to changes in these structures.
SUPPORT OF THE PELVIC ORGANS: CONCEPTUAL OVERVIEW
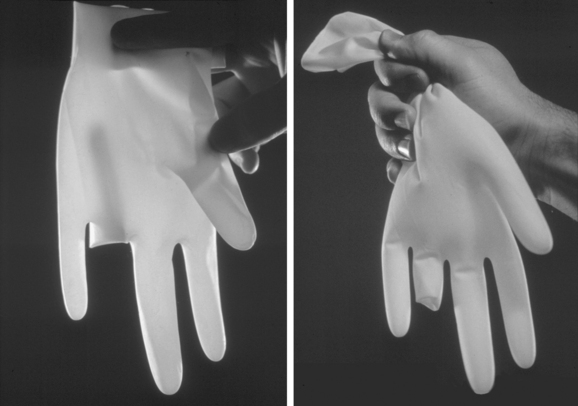
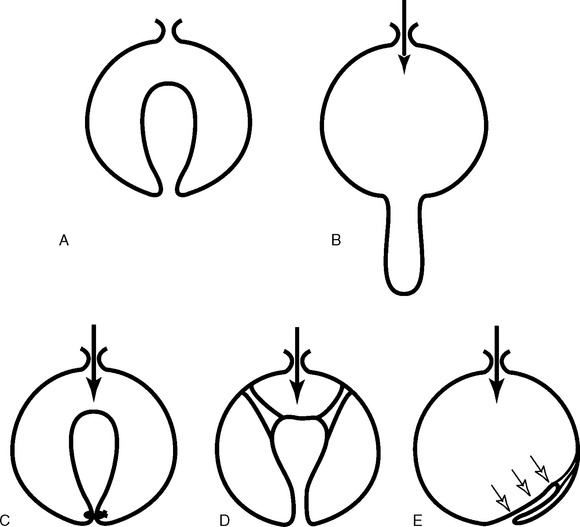
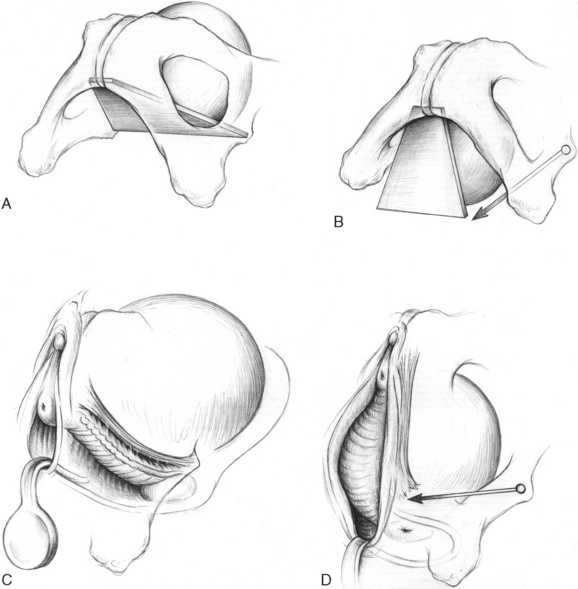
In 1934, Bonney pointed out that the vagina is in the same relationship to the abdominal cavity as the in-turned finger of a surgical glove is to the rest of the glove (Fig. 53-1).4 If the pressure in the glove is increased, it forces the finger to protrude downwards in the same way that increases in abdominal pressure force the vagina to prolapse. Figure 53-2 provides a schematic illustration of this prolapse phenomenon. In Figure 53-2C, the lower end of the vagina is held closed by the pelvic floor muscles, which prevents prolapse by constricting the base of the invaginated finger. Figure 53-2D shows suspension of the vagina to the pelvic walls. Figure 53-2E demonstrates that spatial relationships are important in the flap-valve closure, in which the suspending fibers hold the vagina in a position against the supporting walls of the pelvis; increases in pressure force the vagina against the wall, thereby pinning it in place. Vaginal support is a combination of constriction, suspension, and structural geometry.
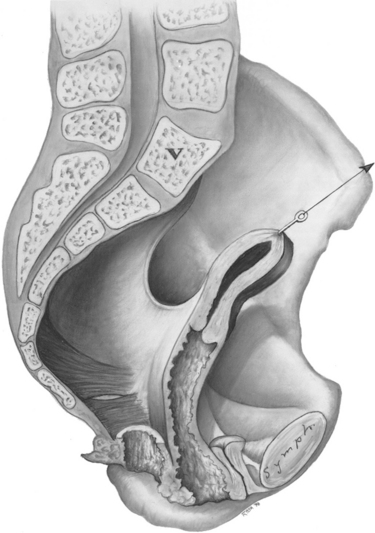
The female pelvis can naturally be divided into anterior and posterior compartments (Fig. 53-3). The genital tract (vagina and uterus) divides these two compartments through lateral connections to the pelvic sidewall and suspension at its apex. The levator ani muscles form the bottom of the pelvis. The organs are attached to the levator ani muscles when they pass through the urogenital hiatus and are supported by these connections.
Functional Anatomy and Prolapse
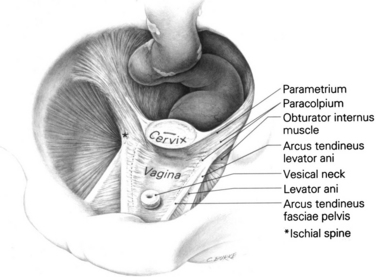
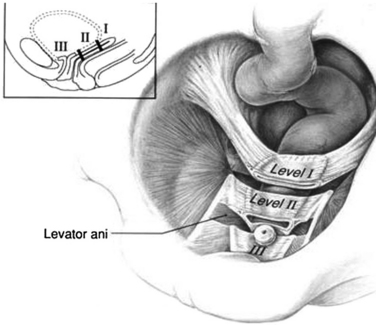
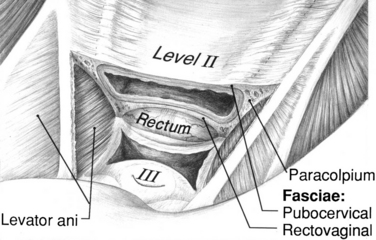
The pelvic organ support system is multifaceted and includes the endopelvic fascia, the perineal membrane, and the levator ani muscles, which are controlled by the central and peripheral nervous system. The supports of the uterus and vagina are different in different regions (Fig. 53-4).5 The cervix (when present) and the upper third of the vagina (level I) have relatively long suspensory fibers that are vertically oriented in the standing position, whereas the midportion of the vagina (level II) has a more direct attachment laterally to the pelvic wall (Fig. 53-5). In the most caudal region (level III), the vagina is attached directly to the structures that surround it. At this level, the levator ani muscles and the perineal membrane have important supportive functions.
In the upper part of the genital tract, a connective tissue complex attaches all the pelvic viscera to the pelvic sidewall. This endopelvic fascia forms a continuous, sheet-like mesentery, extending from the uterine artery at its cephalic margin to the point at which the vagina fuses with the levator ani muscles below. The fascial region that attaches to the uterus is called the parametrium, and that which attaches to the vagina is the paracolpium. Level I is composed of both parametrium and paracolpium. The uterosacral and cardinal ligaments together form the parametrium and support the uterus and upper third of the vagina. The paracolpium portion of level I consists of a relatively long sheet of tissue that suspends the superior aspect of the vagina by attaching it to the pelvic wall. This is true whether or not the cervix is present. The uterosacral ligaments are important components of this support. At level II, the paracolpium changes configuration and forms more direct lateral attachments of the midportion of the vagina to the pelvic walls (Fig. 53-6). These lateral attachments have functional significance: they stretch the vagina transversely between the bladder and the rectum. In the distal vagina (level III), the vaginal wall is directly attached to surrounding structures without any intervening paracolpium. The vagina fuses anteriorly with the urethra, posteriorly with the perineal body, and laterally with the levator ani muscles.
Damage to level I support can result in uterine or vaginal prolapse of the apical segment. Damage to the level II and III portions of vaginal support results in anterior and posterior vaginal wall prolapse. The varying combinations of these defects are responsible for the diversity of clinically encountered problems and are discussed in the following sections.
Apical Segment
In level I, the cardinal and uterosacral ligaments attach the cervix and the upper third of the vagina to the pelvic walls.6,7 Neither is a true ligament in the sense of a skeletal ligament that is composed of dense regular connective tissue similar to knee ligaments. Rather, they are “visceral ligaments” that are similar to bowel mesentery. They are made of blood vessels, nerves, smooth muscle, and adipose tissue intermingled with irregular connective tissue. They have a supportive function in limiting the excursion of the pelvic organs, much as the mesentery of the small bowel limits the movement of the intestine. When these structures are placed on tension, they form condensations that surgeons refer to as ligaments.
The uterosacral ligaments are bands of tissue that run under the rectovaginal peritoneum; they are composed of smooth muscle, loose and dense connective tissue, blood vessels, nerves, and lymphatics.6 They originate from the posterolateral aspect of the cervix at the level of the internal cervical os and from the lateral vaginal fornix.6 Although macroscopic investigation showed insertion of the ligament to the levator ani, the coccygeus, and the presacral fascia,8 examination by magnetic resonance imaging (MRI) showed that the uterosacral ligaments overlie the sacrospinous ligament and coccygeus in 82% of the cases and overlie the sacrum in only 7% of the cases.9 The difference between the appearance of these structures on MRI and on dissection may have to do with the tension placed on the structures during dissection and require further research to clarify.
The cardinal ligament is a mass of retroperitoneal areolar connective tissue in which blood vessels predominate; it also contains nerves and lymphatic channels.7 It has a configuration similar to that of “chicken wire” or fishing net in its natural state, but when placed under tension it assumes the appearance of a strong cable as the fibers align along the lines of tension.7 It originates from the pelvic sidewall and inserts on the uterus, cervix, and upper third of the vagina. Both the uterosacral and cardinal tissues are critical components of level I support and provide support for the vaginal apex after hysterectomy (see Figs. 53-5 and 53-6). The cardinal ligaments are oriented in a relatively vertical axis (in the standing posture), whereas the uterosacral ligaments are more dorsal in their orientation.
The nature of uterine support (Fig. 53-7) can be understood when the cervix is pulled downward with a tenaculum during dilation and curettage. After a certain amount of descent, the level I supports become tight and arrests further cervical descent. Similarly, downward descent of the vaginal apex after hysterectomy is resisted by the paracolpium. Damage to the upper suspensory fibers of the paracolpium (cardinal and uterosacral ligaments) allows uterine or apical segment prolapse (Fig. 53-8).
Anterior Compartment
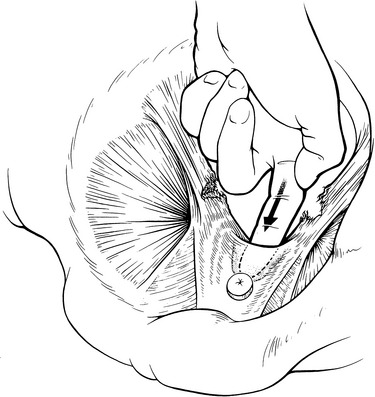
Anterior compartment support depends on the connections of the vagina and periurethral tissues to the muscles and fascia of the pelvic wall via the arcus tendineus fascia pelvis (Fig. 53-9). On both sides of the pelvis, the arcus tendineus fascia pelvis is a band of connective tissue attached at one end to the lower sixth of the pubic bone, 1 cm lateral to the midline, and at the other end to the ischium, just above the spine.
The anterior wall fascial attachments to the arcus tendineus fascia pelvis have been called the paravaginal fascial attachments by Richardson.10 Lateral detachment of the paravaginal fascial connections from the pelvic wall is associated with stress incontinence and anterior prolapse (Fig. 53-10). Further details of the structural mechanics of anterior wall support are provided later. In addition, the upper portions of the anterior vaginal wall are affected by the suspensory actions of level I. If the cardinal and uterosacral ligaments fail, the upper vaginal wall prolapses downward while the lower vagina (levels II and III) remains supported.
Anterior vaginal wall prolapse can occur either because of lateral detachment of the anterior vaginal wall at the pelvic side wall, referred to as a displacement “cystocele,” or as a central failure of the vaginal wall itself that results in distention “cystocele” (Fig. 53-11). Although various grading schemes have been described for anterior vaginal prolapse, they are often focused on the degree of prolapse rather than the anatomic perturbation that results in descent; therefore, it is important to describe anterior prolapse with regard to the location of the fascial failure (lateral detachment versus central failure). At present, although a number of investigators have described techniques to distinguish central from lateral detachment, validation of these techniques remains elusive.
Cystocele caused by defects of the midline fascia is easy to understand, but understanding how lateral detachment results in cystocele is not as obvious. The fact that lateral detachment is associated with cystourethrocele was first established by Richardson and colleagues10 (see Fig. 53-10). A study of 71 women with anterior compartment prolapse showed that paravaginal defect usually results from a detachment of the arcus tendineus fascia pelvis from the ischial spine, and rarely from the pubic bone.11 A visual analogy is that of a swinging trapezoid (Fig. 53-12). The mechanical effect of this detachment allows the trapezoid to rotate downward. When this happens, the anterior vaginal wall protrudes through the introitus. Upward support of the trapezoid is also provided by the cardinal and uterosacral ligaments in level I. For this reason, resuspension of the vaginal apex at the time of surgery, in addition to paravaginal or anterior colporrhaphy, helps to return the anterior wall to a more normal position.
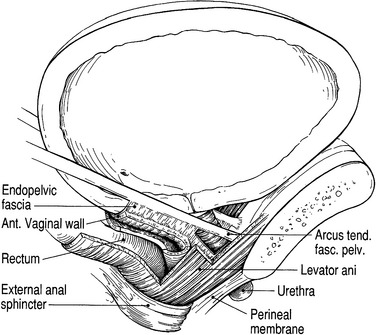
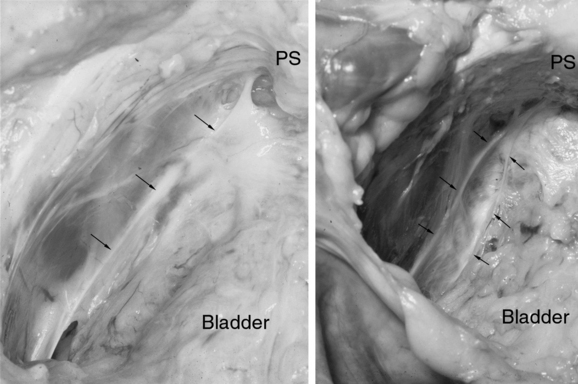
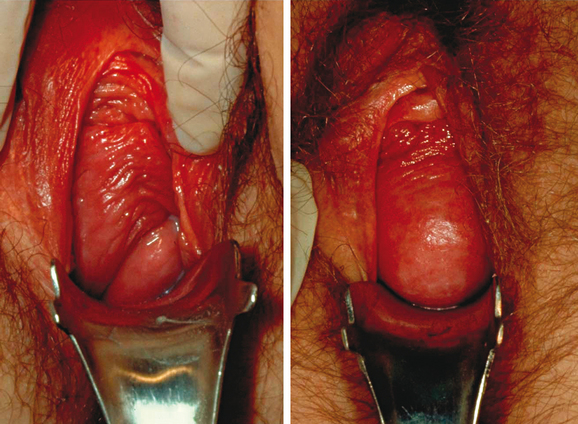
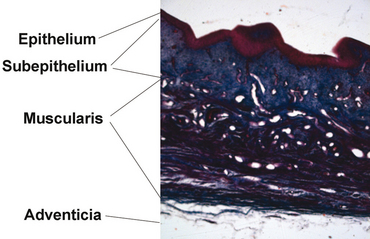
Anatomically, the term endopelvic fascia refers to the areolar connective tissue surrounding the vagina. It continues down the length of the vagina as loose areolar tissue surrounding the pelvic viscera (Fig. 53-13). The term “fascia” is often used by surgeons to refer to the strong tissue that they sew together during anterior repairs. This has led to confusion and misunderstanding of the anatomy. Histologic examination has shown that the vagina is made up of three layers: epithelium, muscularis, and adventitia (Fig. 53-14).12–14 The adventitial layer is loose areolar connective tissue made up of collagen and elastin. These layers form the vaginal tube. The tissue that surgeons plicate during repairs is not what an anatomist would refer to as endopelvic fascia; rather, it is the vaginal muscularis and the adventitial layer of the vaginal tube. Also, many basic science studies that are addressed later in this chapter have used biopsies from the vaginal tube and not from the endopelvic fascia that connects the vaginal wall to the pelvic sidewalls.
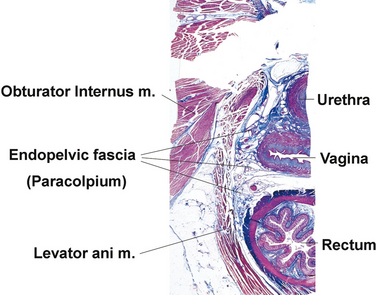
Figure 53-13 Histiologic cross-section of pelvis at the level of the mid-urethra.
(From the collection of Dr. Thomas E Oelrich. © 2005 DeLancey; with permission.)