Fig. 17.1
Operative port placement for robotic right hemicolectomy
The robotic cart is positioned on the same side as the pathology. For right colectomy this means maneuvering the robotic cart and approaching the operating table over the patient’s right shoulder. The vision stack is also located on the patient’s right side, by his right foot (Fig. 17.2). The bedside assistant and the scrub nurse are situated to the patient’s left side. Once the robot is docked, there can be no change to the patient’s or robot’s position, without first undocking the robotic arms. The camera arm is attached to the left iliac fossa port and adjusted to point towards the ileocolic pedicle. The remaining robotic arms are secured to their respective ports. The robotic camera is inserted along with a robotic bowel grasper for arm #3 and a second robotic bowel grasper for arm #2. The monopolar scissors is inserted into arm #1 in the left upper quadrant. The scene is now set for the robotic operation to begin.
Fig. 17.2
Operating room set-up. The robotic cart is located on the patient’s right with the vision stack located inferiorly. The scrub nurse is located near the patient’s left foot. The assistant is located on the patient’s left. The console is also located on the left
Robotic Procedure
Robotic right colectomy does not differ in any way from its laparoscopic counterpart. We routinely perform medial-to-lateral dissection with early division of the ileocolic pedicle close to its origin from the superior mesenteric vessels. Arm #3 provides traction to the cecum/terminal ileum to give tension and to lift the ileocolic vessels. The retroperitoneal space immediately below the vessels is entered and a retroperitoneal “cave” is developed, making maximum use of the pneumoperitoneum (Fig. 17.3). The duodenum is identified and displaced posteriorly and the ileocolic vessels are skeletonized and ligated/divided with clips, endovascular linear stapler, or energy source (Fig. 17.4). Arm #3 then grasps the divided ileocolic pedicle and retracts it toward the anterior abdominal wall. The retroperitoneal “cave” is further developed with identification of the right ureter. Gerota’s fascia is displaced posteriorly and the retroperitoneal dissection is completed out to the lateral parietal attachments and to the underside of the hepatic flexure.
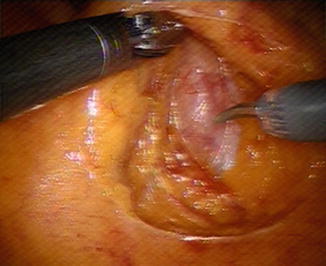
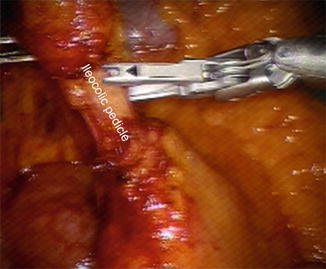
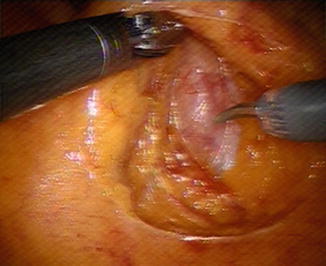
Fig. 17.3
Dissection of the retrocolic “cave” with posterior displacement of the duodenum
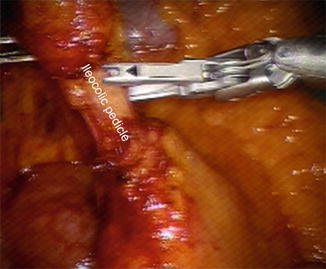
Fig. 17.4
Ligation of the ileocolic vessels with clips
The mesentery of the terminal ileum is divided up to the point of division of the small bowel. The assistant then divides the terminal ileum using a laparoscopic linear stapler. Division of the remaining peritoneal adhesions holding the inferior pole of the cecum and appendix is performed and extended up the right paracolic gutter, thus freeing the entire inferior and lateral part of the right colon. The dissection is completed with division of the hepatic flexure. This is best performed by retracting the right colon with the arm #3 grasper, retracting the transverse colon caudally by the assistant, and opening up the greater sac along the proximal transverse colon.
Once the hepatic flexure has been fully mobilized extending past the origin of the middle colic vessels, consideration is given to whether the middle colic vessels should be divided. This is a decision based upon the location of the tumor in the right colon. For proximal cancers it is usual to take the right branch of the middle colic artery. For hepatic flexure tumours the entire middle colic blood supply may be sacrificed. Division of the middle colic vessels may take either an infracolic or supracolic approach, depending on the ease of access. Vessel division and ligation is performed by the assistant using either clips or the laparoscopic linear stapler with a vascular cartridge. The right colon is now fully mobilized and resection is completed by division of remaining mesocolon up to the point of resection of the transverse colon.
The next decision is whether to perform an extracorporeal or intracorporeal anastomosis. For an extracorporeal anastomosis, the robot is undocked and a 5-cm umbilical incision is made to accommodate an Alexis wound retractor (Applied Medical). The right colon is delivered through the wound retractor and the resection and anastomosis completed in the usual fashion. For an intracorporeal anastomosis, the proximal transverse colon is divided by the assistant with a laparoscopic stapler and the mobilized right colon placed out of the way in the pelvis. Two sutures are used to approximate and orientate the divided ends of the terminal ileum and transverse colon. An enterotomy and colotomy are made at the distal proposed anastomotic site using diathermy scissors. A laparoscopic stapler is placed into the lumen of the bowel ends by the assistant with tension provided by a robotic grasper on the orientating sutures. The stapler is fired and carefully removed to prevent spillage of enteric contents (Fig. 17.5). The resulting entero-colotomy is closed by robotic suturing to complete the anastomosis (Fig. 17.6). The resected right colon is retrieved and extracted through a convenient site, but usually in the suprapubic region for best cosmesis. A final laparoscopic inspection is performed to ensure good hemostasis and the wounds closed taking care to prevent port-site herniation.

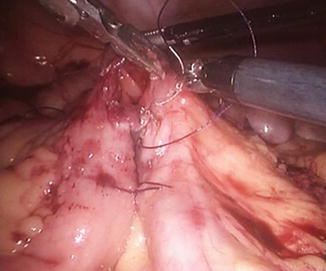

Fig. 17.5
A linear stapler is passed through one of the upper ports and is used to create the ileocolostomy anastomosis
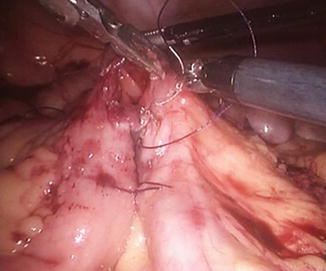
Fig. 17.6
The entero-colotomy is closed with two layers of absorbable suture to complete the anastomosis
Postoperative Management
Postoperatively, patients are managed according to an enhanced recovery protocol [20]. Fluids are given as tolerated including dietary supplements and soft diet is commenced as tolerated from postoperative day #1. Patient controlled analgesia (PCA) is used until fluids and oral analgesia are tolerated. Early mobilization is encouraged with physiotherapy support. Thromboprohylaxis with fractionated subcutaneous heparin and antiembolism stockings is continued in the early postoperative period and continued for 1 month. Further antibiotics are avoided, unless there is a clinical indication. Patients are discharged when they are tolerating normal diet, mobile, and comfortable on oral analgesia.
Complications
The potential complications following robotic right colectomy include those related to any major abdominal operation with general anesthesia and those specific to a laparoscopic or robotic approach.
Conclusions
The technical advantages of the robot over conventional laparoscopy have been well-documented. In our opinion, the main advantages in right colon surgery include the stable camera platform, the additional dexterity of the Endowrist (Intuitive) instruments allowing precise dissection at the root of the ileocolic and middle colic vessels, and the ease of formation of an intracorporeal anastomosis.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








