Chapter 21 Plastic Pancreaticobiliary Stents and Nasopancreaticobiliary Tubes
Concepts and Insertion Techniques
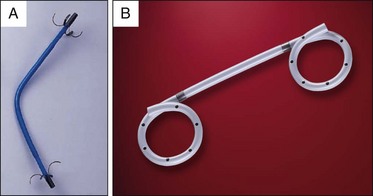
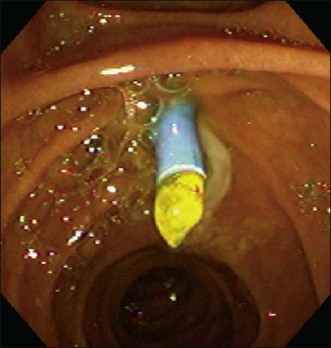
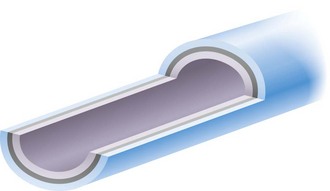
The use of plastic biliary stents for drainage of the bile duct was described over 3 decades ago1 and plastic pancreaticobiliary stents are used for a variety of indications.2 These stents are used for malignant and benign conditions and have proven reliable and safe for decompression of the biliary tree. Palliative insertion of biliary stents relieves distal biliary obstruction as effectively as surgical bypass.3 Plastic stents are available in a variety of configurations and lengths and are composed of Teflon, polyethylene, or polyurethane (Tables 21.1 and 21.2).2,4 Common configurations are straight, single pigtail, or double pigtail (Fig. 21.1). All plastic stents have limited patency due to occlusion with debris and biofilm (Fig. 21.2)5 and require periodic replacement when long-term drainage is required. Nearly all stents of the same diameter have similar patency rates. A 10 Fr stent with a unique double-layer design (Fig. 21.3) has been shown in more than one prospective study to have prolonged patency when compared to standard stent design,6 although in another study it was shown to be equivalent to other plastic stents.7
Table 21.1 Plastic Biliary Stents
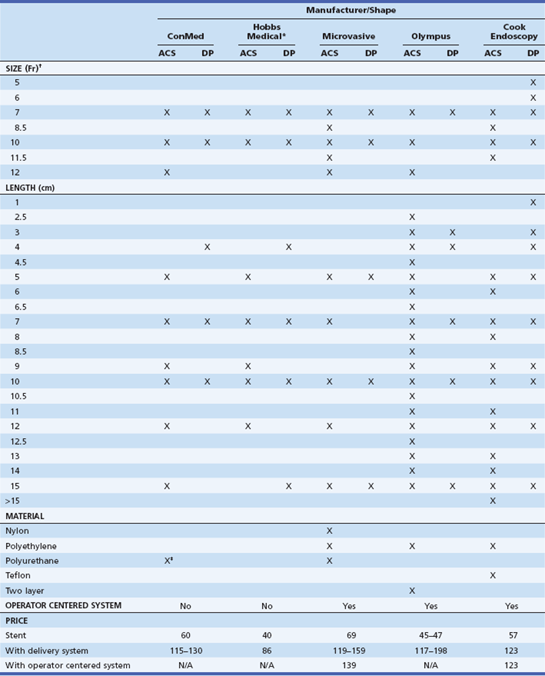
ACS, Angled, curved, or straight; DP, double pigtail; N/A, not available..
*Hobbs Medical did not disclose its stent material for this review.
†Stents >10 Fr require a 4.2-mm channel duodenoscope.
‡Covered with hydromer coating.
From Somogyi L, Chuttani R, Croffie J, et al. Biliary and pancreatic stents. Gastrointest Endosc. 2006;63(7):910-919.
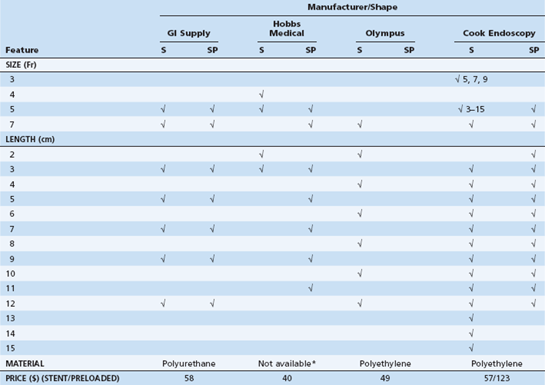
S, Straight; SP, single pigtail.
*Hobbs Medical did not disclose its stent material for this review.
From Somogyi L, Chuttani R, Croffie J, et al. Biliary and pancreatic stents. Gastrointest Endosc. 2006;63(7):910-919.
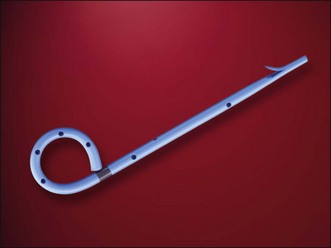
Plastic stents are easy to insert, effective for decompression, and inexpensive to use. Almost all plastic stents are hollow tubes. Side holes are present to a variable degree, but uniformly present in pancreatic duct stents to allow drainage of side branches (Fig. 21.4). A star-shaped stent with a limited central lumen (Fig. 21.5) is available for both biliary and pancreatic insertion (Viaduct, GI Supply, Camp Hill, Pa.).8 The central lumen allows only a guidewire and is inserted without an inner guiding catheter even for 10 Fr diameter stents (see Stent Systems below). A biliary stent with an antireflux valve (windsock) to prevent stent occlusion due to food and vegetable material (Cook Endoscopy, Winston-Salem, N.C.) is also available and may have improved patency over conventional large-bore 10 Fr stents.9
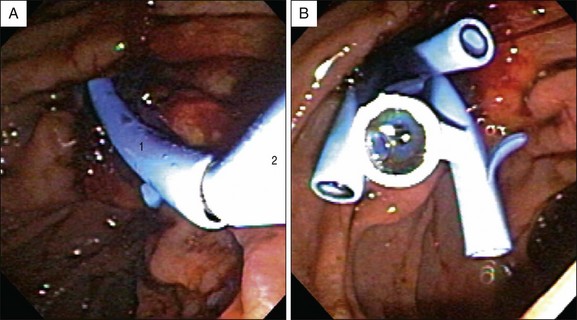
Stent Systems
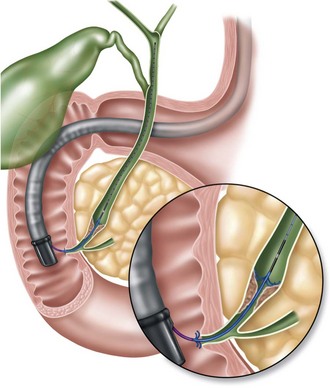
A variety of stent systems are available as discussed in Chapter 4. Stents smaller than 8.5 Fr diameter are usually placed directly over a guidewire using a pusher tube. Stents greater than 8.5 Fr diameter typically include an inner guiding catheter that passes over the guidewire (Fig. 21.6); the stent and pusher tube are then passed over the inner guiding catheter (Fig. 21.7). The inner guiding catheter promotes stability and rigidity, which are necessary to allow stent passage across tight strictures.
Distal Biliary Obstruction
The approach to distal biliary strictures is more straightforward than for hilar tumors and will be discussed separately. After successful deep cannulation of the biliary tree contrast is introduced to clearly elucidate the margins of the stricture to allow for selection of the appropriate stent length. The stricture is traversed with a guidewire. It is important to pass the wire well proximal to the stricture to prevent wire loss and to provide mechanical advantage, although care must be taken to preclude perforation through the liver capsule. In general, a biliary sphincterotomy is not required for insertion of stents up to 10 Fr diameter10 and is not protective of post-ERCP pancreatitis after stent placement for malignant biliary obstruction.11 However, one study showed that in patients with bile leaks, placement of 10 Fr stents without a sphincterotomy was associated with a higher rate of post-ERCP pancreatitis.12 A biliary sphincterotomy is required when multiple stents are placed, such as in the treatment of benign strictures (see Chapter 40).10
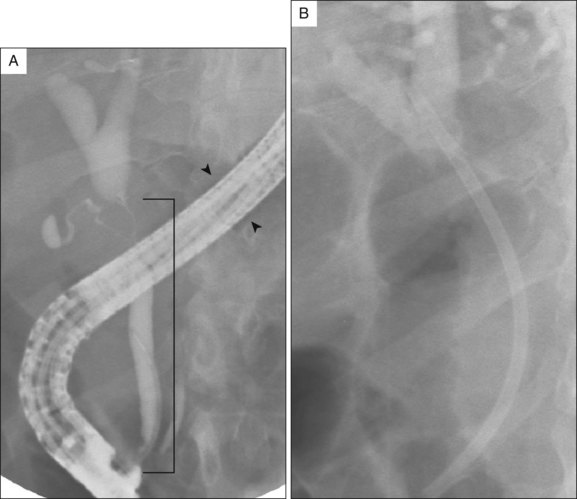
When multiple stents are placed, using a slightly longer initial stent is helpful as the friction created by passage of additional stents during insertion may result in upward movement. If the first stent is too short, it may migrate into the duct. This is usually of no consequence assuming that the stent is still across the stricture. The length of the stent chosen is based on the distance from the papilla to the proximal edge of the stricture plus an additional 2 cm. Excessively long stents should be avoided, as distal migration tends to occur into the duodenum until the proximal flange or pigtail impacts at the top of the stricture; meanwhile, the distal end of the stent may impact and perforate the opposite duodenal wall (Fig. 21.8). In general, 5- or 7-cm–long stents are of sufficient length for nearly all biliary strictures resulting from pancreatic cancer. Defining the stricture length can be achieved in several ways. One way is during withdrawal of the initial cannulating catheter. When the catheter tip is at the proximal end of the stricture, the endoscopist holds the catheter just outside the biopsy port; the catheter is withdrawn until it is endoscopically visible in the duodenum just distal to the papilla. The distance from the endoscopist’s fingers to the biopsy port is measured and represents the stricture length. Anecdotally, this method seems to overestimate the length of the stricture. Another way is to use the radiograph to measure the length of the stricture. When the tip of the endoscope is in contact with the papilla, a radiographic image is captured. The distance from the tip of the endoscope to the proximal edge of the stricture is measured. The diameter of the endoscope is used as a comparison measuring point to determine the true stricture length and account for a magnification factor. The following equation is used to solve for the unknown variable X, which is true stricture length (Fig. 21.9):
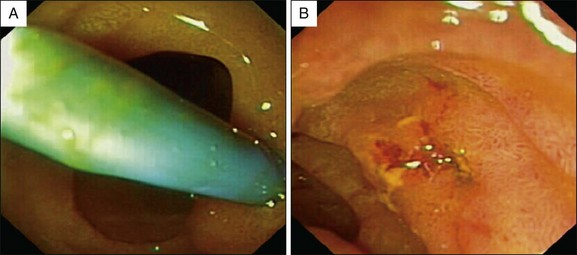
In patients with short, distal bile strictures (e.g., chronic pancreatitis, postsphincterotomy ampullary stricture), three to four 10 Fr 5-cm–long stents can be mounted on the inner guiding catheter at one time. Once the first stent is placed (Fig. 21.10) the inner guiding catheter and guidewire are withdrawn just enough to release this first stent; the duct is then recannulated alongside the first stent with the second stent, guidewire, and inner guiding catheter. The process is continued until all stents are deployed. Alternatively, the stents can be placed one by one alongside each stent (Fig. 21.11).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree