Chapter 14 Access (Precut) Papillotomy
The cardinal step of therapeutic endoscopic retrograde cholangiopancreatography (ERCP) is deep cannulation of the desired duct, usually the common bile duct (CBD). This also can be the most challenging and humbling aspect of the procedure. For successful biliary intervention, deep access to the biliary tree is a prerequisite. Given the availability and accuracy of magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EUS), there are only limited indications for diagnostic ERCP. The role of diagnostic ERCP is now limited to tissue sampling from biliary or pancreatic lesions, sphincter of Oddi dysfunction (SOD) manometry, and diagnostic cholangioscopy/pancreatoscopy, and all of these also require deep access to the desired duct. Since the initial description of precut sphincterotomy by Siegel in 1980,1 successful biliary cannulation has improved significantly. However, despite technical innovations, improved endoscopic imaging, and specialized accessories, deep biliary cannulation may still fail in 5% to 15% of cases, even in experienced centers. In these situations the use of alternative techniques may be necessary. Even though access papillotomy is probably the most accurate term to describe the method, in this chapter we will use the term precut, which is most popularized. As opposed to traditional biliary sphincterotomy, precut is usually not a planned intervention, but endoscopists must be prepared for this event in case of unsuccessful cannulation. This chapter focuses on precut techniques, equipment used by most experts, outcomes, and adverse events. We will discuss indications, contraindications, and evidence that supports our recommendations. We will not discuss the use of needle-knife sphincterotomy over a stent in special situations such as Billroth II anatomy or pancreas divisum, as this is covered in Chapters 20 and 29.
Indication for Precut Papillotomy
Precut papillotomy has been considered the weak point of many endoscopists but also the ultimate tool for succeeding in therapeutic biliary procedures. When there has been repeated instrumentation of the pancreatic duct without selective biliary cannulation or multiple attempts without cannulation of either duct, alternative methods of cannulation should be considered. It is very important to change one’s approach rather than to persist with the same unsuccessful technique. The decision to change the approach should be made early, particularly in patients who are at high risk for post-ERCP pancreatitis. It should be done before the ampulla is traumatized and the pancreatic duct is overly manipulated or opacified. Prior to considering a precut, two alternative techniques may be considered.2,3 It is our practice that if the pancreatic duct is selectively cannulated with a guidewire, we attempt the dual wire technique, leaving the guidewire in the pancreatic duct and using a cannula or sphincterotome beside the wire to cannulate the bile duct. The pancreatic wire may straighten the intraampullary portion of the distal bile duct, allowing for successful biliary cannulation. If this fails after a couple of attempts, a small caliber (3 to 5 Fr) pancreatic stent is placed and another couple of attempts to cannulate the bile duct above the stent are carried out. If deep cannulation of the CBD is still not achieved, a precut papillotomy is performed.
The decision to proceed to a precut when standard cannulation techniques fail depends on several factors, including the indication for the ERCP, the expertise of the endoscopist performing the ERCP, and the other expertise available. Marked variation exists in the use of precut sphincterotomy, which may be as infrequent as 1% or as frequent as 38% of cases.2,4 Successful cannulations are reported in 70% to 90% of first attempts with ultimate success of subsequent ERCP in 92% to 99% of cases.2,4
Other options following a failed standard cannulation include stopping the procedure and reattempting the ERCP at another session or referring the patient to another endoscopist or center with more experience. Techniques such as percutaneous and EUS rendezvous techniques have been described to achieve deep biliary cannulation. However, in most situations a precut papillotomy will be the first technique attempted when standard biliary cannulation fails. It is important that the endoscopist attempting a precut be experienced and comfortable with the technique. If not, it is best to abort the procedure and explore other options for gaining access (Box 14.1).
Video for this chapter can be found online at www.expertconsult.com.
Precut Accessories
Accessories used for precut papillotomy should be available for all ERCPs, since the need for precut is unpredictable prior to the procedure. The most widely used type of papillotome in this category is the needle-knife catheter. These catheters have a retractable electrosurgical cutting wire. The control handle has a mechanism for projecting the wire forward from the distal aspect of the catheter. The length of the exposed needle is adjustable. With the needle in contact with the mucosa, activation of current and manual movement of the catheter and endoscope permits cutting of the targeted tissue. These catheters are available in variable tip length (4 to 7 mm) and have either single-, double-, or triple-lumen configuration. A new insulated-tip needle knife to protect the papillary orifice is not yet available in North America. The second type of precut papillotome is referred to as an Erlangen-type papillotome and is similar to the standard traction-type sphincterotome. It has an ultrashort 5-mm-long monofilament cutting wire and a less-than-1-mm catheter tip distal to the wire.5 Soft-tipped hydrophilic guidewires must be available. We recommend the use of electrosurgical units with pulsed modes, which have a microprocessor control generator in which cutting and coagulating currents alternate and are automatically adjusted according to the tissue resistance. The advantage of these modes is that a stepwise cutting action results, which allows for precise control of direction depth and length of the precut.
Techniques
Precut sphincterotomy implies unroofing the papilla to expose the biliary orifice and allow for deep cannulation. Unlike the traditional biliary sphincterotomy that enlarges the biliary opening for extraction of stones and placement of stents, the precut is used purely for biliary (occasionally pancreatic) access (Box 14.2).
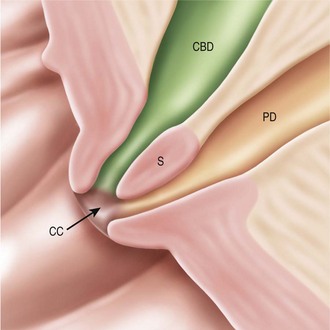
To understand the concept of precut technique, it is essential to understand the anatomy of the ampulla of Vater in a three-dimensional way. The terminal parts of the bile duct and pancreatic duct taper down to the opening on the medial duodenal wall. The ampullary segment is enveloped by biliary, pancreatic, and ampullary sphincters. These sphincters are covered by duodenal mucosa and submucosa and the bile duct and pancreatic duct join just before termination of the duodenum, forming a common channel approximately 5 mm long. In most patients the pancreatic duct enters the ampulla in a straight fashion at the 1 o’clock position and cannulation is easy (Fig. 14.1). The bile duct is located more superficially and runs parallel to the duodenal wall terminating at the 11 to 12 o’clock position. Since precut is often a freehand technique, the understanding of this three-dimensional anatomy is imperative (Box 14.3).
Needle-Knife from the Orifice
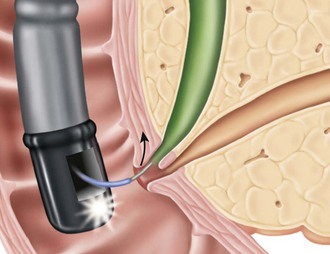
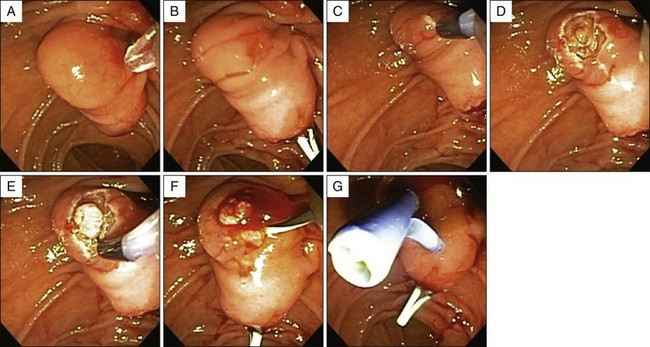
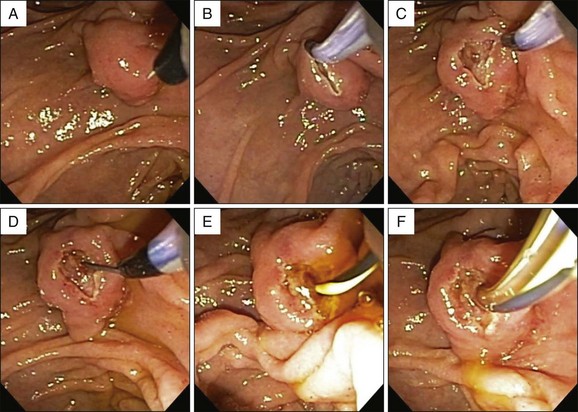
The most widely practiced method is the freehand needle-knife technique in which the incision is made starting at the orifice and extending upward to the roof of the papilla (Fig. 14.2; Cases 14.1 and 14.2). The first step should be a sham precut with the needle retracted. A few practice movements are performed to ensure that the incision will be performed in the intended direction. The direction of the cut is the most critical aspect of the procedure and determines its success or failure.6 Originally this technique was described by using an upward motion with the elevator.7 It has been suggested by Howell that improved control and safety can be achieved by “loading” the needle knife by upward traction of the endoscope. The length of the fully exposed needle is 4 to 7 mm, but we usually only expose 2 to 3 mm of the cutting wire. The tip of the needle is positioned at the upper margin of the papillary orifice, current is applied, and a 2- to 5-mm incision is made on the papillary bulge. The length and depth of the incision depends on the size and configuration of the papilla and the length of the intraduodenal segment. We recommend that the incision is made in short increments with repeated gentle strokes opening the papilla gradually in layers.6,7 When current is applied, the needle should be in continuous motion to avoid deeper thermal damage. Once the mucosa is separated, the mucosal edges should be pushed aside with the catheter, and the underlying sphincter is visualized. Gentle suction often amplifies the sphincter and may promote bile drainage. The site is carefully examined looking for nodularity of biliary epithelium that usually appears as a pink or brownish nodule. The area is gently explored with the precut catheter with retracted needle or guidewire. It is very important that the incision is probed gently without injecting any contrast unless deep cannulation has been achieved. Injection of contrast prior to deep access may result in submucosal injection compromising further attempts. Our preferred modality to explore the precut site is with the use of the tip of a hydrophilic guidewire. Once deep access has been achieved, the sphincterotomy can be completed with a standard sphincterotome. If cannulation is still not successful and the patient is stable, a repeat attempt can be made in 48 to 72 hours, and frequently, once the edema has subsided, the biliary orifice is easily identified. Success rate for repeat attempts ranges from 80% to 100%. However, depending on the clinical situation, and especially if the patient is septic and the biliary cannulation is not successful, placement of a percutaneous drain may be required urgently following the initial failed attempt.