Chapter 2 The ERCP Room
The endoscopic retrograde cholangiopancreatography (ERCP) room can range from very basic to state-of-the-art. While smaller centers with low ERCP volumes can adequately manage their caseload by performing ERCP in radiology or operating suites, most centers performing high-volume ERCP have designed dedicated ERCP rooms within the endoscopy unit. A basic ERCP room requires a quality fluoroscopy unit with still image capability in addition to the endoscopic equipment. Major innovations in the field of interventional endoscopy have led to the development of multipurpose interventional rooms with the ability to combine endoscopic ultrasound (EUS), cholangioscopy, pancreatoscopy, confocal endomicroscopy, and other interventions with ERCP. A well-designed ERCP room is needed to accommodate this expansion in ERCP complexity. In addition, changes in patient populations have led to the necessity to be able to perform ERCP on morbidly obese patients and those with altered anatomy using deep enteroscopy instruments (see Chapter 29). Many centers have transitioned to anesthesia support for all ERCPs. The cumulative effect of these changes in ERCP practice has led to substantial changes in the design of the ERCP room, with the incorporation of new technology to benefit the patient, endoscopists, and allied health staff.
Evolution of the ERCP Room
The basic intent of ERCP has not changed. Endoscopic visualization of the ampulla and cannulation of the desired ductal system with high-quality radiographic images that guide the appropriate therapy remain the goal. In the great majority of cases, basic equipment to remove a biliary stone or place a biliary stent is all that is needed. What has changed is the complexity of ERCP, especially at tertiary centers. The need for high-quality radiographic imaging to define focal pathology in patients with higher body mass indexes (BMIs) has led to modified digital fluoroscopy equipment with improved resolution, reduced radiation exposure, and the ability to function continuously during long procedures without overheating. The use of mobile or fixed C-arm systems is often employed to improve visualization of the biliary tree by changing the plane of examination to profile the bifurcation and selected ductal system (see Chapter 3). Additional space for supplemental equipment for performing manometry, cholangioscopy, EUS (with rendezvous), laser lithotripsy, deep enteroscopy, and other techniques has increased the size requirements of the typical ERCP room. The need for space for anesthesia equipment has further increased the area needed at the patient’s head. The obesity epidemic has also led many centers to modify their approach to room design. The use of fixed fluoroscopy systems with wider tables (≥30 in) and increased weight limits (≥450 lb) has become the norm. Access to the x-ray table with larger stretchers and beds has required room designs with additional space for these situations (Fig. 2.1). Transferring the sedated or recovering patient from the fluoroscopy table to the stretcher or bed can be challenging and is facilitated with sliding boards and access to the back of the fluoroscopy table. All of these factors in combination with the need to use and store a large variety of devices in close proximity to the endoscopist have driven the size of well-designed, advanced interventional endoscopy rooms to greater than 500 square feet.
Staffing for the ERCP Procedure
Staffing for ERCP procedures is a major factor in determining the size and layout of the ERCP room and remains variable around the world. Typically an endoscopist and a minimum of two assistants are necessary to complete an ERCP. The first assistant (nurse or technician) stands adjacent to the endoscopist and operates devices, manipulates guidewires, and performs other maneuvers to facilitate completion of the procedure. A registered nurse or member of the anesthesia staff is positioned at the head of the patient and administers moderate sedation or anesthesia while monitoring the patient’s respiration and cardiac status throughout the procedure (see Chapter 5). Often a second assistant (nurse or technician) is in the room and assists in preparing devices for use and for documentation of the specifics of the procedure. In many settings a radiology technician is also present. This creates a close working environment during the procedure with at least three individuals clustered in close proximity to the patient’s head. A well-designed workspace makes this proximity tolerable, efficient, and even enjoyable.
Room Layout
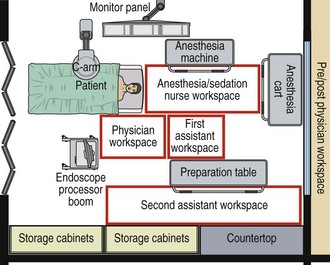
The key to a successful room design is early collaboration with the critical partners that make the ERCP room functional and beneficial to all parties. Collaborative input from endoscopists, the endoscopy nursing team and technicians, the anesthesia team, radiology support staff, the radiation safety officer, an ergonomics consultant, and the construction or design team can result in substantial design evolution that allows the final design to be successful and optimized for the work group. The layout of a typical tertiary-level ERCP room is depicted in Fig. 2.2. The ERCP room can be divided into multiple work areas. The epicenter of the ERCP room is the fluoroscopy table on which the patient is positioned. The endoscopist stands adjacent to the patient’s head. In the room design depicted in Fig. 2.2 the endoscopist also has direct access to the radiographic equipment controls that allow movement of the fixed C-arm or table to obtain the optimum radiographic imaging of the pancreaticobiliary tree. The workspace of the assistant involved with device manipulation is immediately adjacent to the endoscopist. Adjacent to this area is a preparation area in which a second assistant can prepare devices for use, with a countertop or movable table. This space should be immediately adjacent to the in-room storage of essential devices that are used for all ERCPs. Directly at the patient’s head is a space for the sedation nurse or anesthesia team member that also includes room for all necessary medications, monitoring equipment, and resuscitative equipment. A separate space for radiograph review and report generation should be available for the endoscopist. This space may be behind a protective lead glass screen or in a separate workspace. In some situations a separate control room for radiology equipment may be necessary. Alternatively, a radiation technologist may be in the room with the team operating the equipment.
The endoscopist should have immediate access to all endoscopic and radiographic controls that are necessary to complete the ERCP. The use of ceiling booms greatly facilitates the placement of processors and devices in close proximity to the endoscopist and assistant with minimal cords or tubing on the floor (Fig. 2.3). The boom can be used to house the endoscope processor and light source, electrocautery unit, and other ancillary equipment such as carbon dioxide (CO2) insufflator, water irrigation, EUS equipment (if compact), and other devices. The typical room design has the endoscopic and radiographic monitors directly across the patient’s head to allow a direct line of sight by the endoscopist. The monitors should be adjustable in height to accommodate short and tall endoscopists1 as well as patients in the supine position (see Chapter 9). An ancillary monitor to display additional images or information such as choledochoscopy, manometry, EUS, and patient vital signs greatly facilitates completion of procedures without awkward head angulation by the endoscopist (Fig. 2.4, A). Rooms with video integration systems are available that allow multiple video sources to be displayed on the monitor array in the ERCP room. This can be particularly helpful if a computed tomography (CT) scan, previous cholangiogram, or other radiograph needs to be reviewed during the procedure. The monitors should be in the line of sight of the first assistant as well to allow coordinated device manipulation with both endoscopic and fluoroscopic guidance. There should be ample space for ancillary devices (EUS processors, choledochoscopy devices, etc.) to be placed in the room in close proximity to the endoscopist. In the overall layout there should be sufficient space for patient movement into and out of the room on large stretchers or beds. For improved efficiency, easy access to the endoscopic reprocessing room should be considered (Fig. 2.5), which allows rapid movement of contaminated endoscopes to the cleaning room and facilitates room turnover.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree