Chapter 28 PELVIC FLOOR REHABILITATION IN THE MANAGEMENT OF URINARY STRESS INCONTINENCE
Stress urinary incontinence (SUI) is the complaint of involuntary leakage on effort, exertion, sneezing, or coughing.1 It results from specific damage to the muscles, fascial structures, and nerves of the pelvic floor.2 Commonly accepted etiologic factors include perinatal damage, pregnancy, hereditary predisposition, strenuous physical activity, chronic cough, obesity, and aging.3,4 Many women have difficulty participating in physical exercises and social activities because of urinary leakage. SUI is not a condition that improves over time without treatment,5,6 and it is remarkable that so few women seek professional care or advice for their symptoms.
The pelvic floor has an important function in relation to lower urinary tract function. The levator ani complex provides anatomic support to the bladder outlet. Parts of the levator collectively play an important role in maintaining the position of the pelvic viscera. Contraction of the attachments of the levator ani to the vagina and external sphincter is responsible for the anterior movement of these viscera toward to the pubis symphysis.7,8 Urethral support is an important factor in SUI in women, because support in symptomatic women may be inadequate. According to De Lancey and Delmas,8 the connections of the vagina and urethra to the levator ani muscles and arcus tendineus fasciae pelvis determine the structural stability of the urethra. If the connective tissue fails, the urethral supports cannot stay in their normal alignment, and SUI often occurs. Conversely, if the muscles are damaged, their action in supporting the urethra may be lost. Genuine SUI is defined as an involuntary loss of urine caused by an increase in intra-abdominal pressure that overcomes the resistance of the bladder outlet in the absence of a true bladder contraction. The decrease in bladder outlet or urethral resistance may result from poor anatomic support of the bladder neck (i.e., urethral hypermobility), loss of urethral function (i.e., intrinsic sphincter deficiency), or low urethral closure pressure, alone or in combination with other factors.9 The anatomic support of the bladder outlet, which is critical to maintaining continence, is provided by constant levator tone in normal females.10,11
Physiotherapy for SUI is a widely accepted mode of conservative treatment that involves pelvic floor muscle exercises (PFMEs), with or without biofeedback, electrical stimulation, and weighted vaginal cones and balls. The purpose of pelvic floor re-education is to increase the strength and functional activity of the pelvic floor muscles, which may reduce the problem of SUI.12 Because conservative therapy seems to have no side effects, it should be the first choice for treating SUI.13
PELVIC FLOOR MUSCLE EXERCISES
According to Gilpin and associates,10 within the pelvic floor, the distribution of fiber types is approximately 70% slow-twitch fibers and 30% fast-twitch fibers. These investigators also described a decrease in type II fibers in the periurethral and perianal area in women with symptoms of genitourinary prolapse or urinary stress incontinence. This finding suggests that changes in pelvic floor muscle function are associated with prolapse and incontinence.
During periods of increased intra-abdominal pressure, the pelvic floor muscles are believed to act as a type of platform or hammock, as described by DeLancey.14 The hammock of muscles under the urethra allows the increased intra-abdominal pressure to compress the urethra against this resistance, preventing urine leakage. Recognizing the role of the endopelvic fascia, Petros and Ulmsten15 proposed the integral hypothesis based on the view that the pelvic floor is a single functional unit. If a part of the structure (e.g., the pubourethral ligament) is weakened, the hammock loses some of its original function and cannot perform efficiently. The integral theory also suggests that obstruction of the urethra is caused by sphincter activity and compression of the urethra as a result of contraction of the pelvic floor muscles.
Dougherty16 postulated that the effects of pelvic floor muscle training (PFMT) on the symptoms of stress incontinence are the result of muscle hypertrophy. Muscle hypertrophy accounts for most gains achieved by skeletal muscle; however, Dougherty also suggests that neuromuscular coordination is at least as important as hypertrophy for the successful treatment of stress incontinence. In 1998, Miller and colleagues17 described a study of older women (mean age, 68 years) who had symptoms of mild to moderate stress incontinence. The intervention group was taught the technique of intentionally contracting the pelvic floor muscles before and during a cough, a method called the knack. Within a week, the results showed a significant reduction in urine loss when the women used the knack compared with coughing without precontraction of the pelvic floor.
PFME therapy has proved effective for all three forms of incontinence,18 and PFMEs are recommended as the first choice of treatment for women with these types of urinary incontinence after remediable conditions have been excluded. In prior studies, up to 70% of patients were cured or improved after therapy,13 but success rates declined during follow-up as adherence to the program deteriorated.19–21 An intervention aimed at promoting long-term adherence to PFME therapy seems warranted. Various investigators have pointed out that patient education in physiotherapy, especially the part of encouraging adherence behavior, lacks a systematic behavioral approach.22 A literature search was conducted to evaluate approaches designed to improve adherence to PFME therapy. In four studies, the PFME program included adherence-promoting strategies: audiocassette tapes to guide exercising at home, telephone calls as reminders, and follow-up visits to provide feedback and reinforcement. One study found that after 6 weeks of training at home, adherence was significantly better in the group that had used an exercise tape, compared with the group without the23 tape. Surprisingly, in the other three studies, adherence behavior itself was not measured24 or not related to the adherence-promoting strategies,25 and the efficacy of these strategies therefore remains unclear.
Adherence to PFME therapy was operationalized according to the following behavioral advice:
Most women seem to have learned to adapt their adherence behavior to their symptoms. A similar adaptation pattern was found in the study of Burns and colleagues,24 who argued that women with mild symptoms may not perceive their incontinence as a problem warranting sustained effort, whereas women with many daily losses recognize it as an ongoing problem and make a persistent effort as a positive response occurs. This structure, coupled with an enthusiastic physiotherapist, seems most important for realizing long-term effects and optimal adherence behavior of organized training.
PELVIC FLOOR MUSCLE TRAINING PROGRAMS
Kegel26 recommended performing as many as 300 to 400 pelvic floor muscle contractions daily but gave little information about the intensity of each contraction. As described by Bø,27 the two main principles of strength training for skeletal muscles are overload and specificity. Specificity is particularly important in relation to the pelvic floor muscles because approximately 30% of women have difficulty performing a correct contraction on the first attempt. The pelvic floor is surrounded by many larger groups of muscles, such as the quadriceps and glutei. Women often incorrectly contract these muscle groups when attempting to contract the pelvic floor muscles.
Another common mistake is to produce a Valsalva, or bearing-down, maneuver. Bø27 also describes the importance of instructor-conducted exercises in establishing the correct action of the pelvic floor muscle and maintaining motivation to continue with the exercise program.
In addition to the muscle group being exercised, specificity concerns the type of training used in relation to the dysfunction and symptoms. For example, in a case of urinary stress incontinence, the function required of the pelvic floor muscles is to assist the urethral closure pressure provided by the urethral sphincter, the resting tone of the levator ani, and mucosal coaptation. This requires a quick, maximum voluntary contraction of the pelvic floor muscles; in this case, the training program must emphasize type II fibers. During contraction of the pelvic floor muscles, motor units are recruited in order of increasing size, with type I fibers recruited at low intensity and type II fibers recruited only at high intensity. The training program therefore must include high-intensity exercises. Type II fibers fatigue rapidly because of the rapid depletion and slow replacement of adenosine triphosphate. For this reason, the exercise program should allow relaxation between contractions. The contribution of type I fibers should not be overlooked; they are responsible for maintaining the postural position of the pelvic floor, from which type II fibers can then function effectively.28
Traditionally, PFMEs are practiced in isolation, without activity of the abdominal or hip muscles. However, Sapsford and colleagues29 describe how this practice has been challenged by a number of physicians, who noticed activity in the rectus abdominis in association with pelvic floor muscle contraction and palpable coactivation of the abdominal muscles during functional activities, such as raising the head and shoulders. Sapsford and colleagues29 showed that the rectus abdominis, obliquus internus abdominis, obliquus externus abdominis, and transversus abdominis are coactivated with maximal contraction of the pelvic floor muscles. Sapsford and colleagues29 also showed that the reverse occurs; pubococcygeal electromyographic activity in-creased in response to isometric contractions of the abdominal muscles. These investigators suggested that this activity could be used for therapeutic effect by encouraging submaximal deep abdominal isometric contractions to enhance pubococcygeal training. The study also considered the effect of altering the position of the lumbar spine during exercise and concluded that a neutral or extended position is preferable.
The functional evaluation of pelvic floor musculature is rife with technologic and cultural challenges. Compared with muscles outside of the pelvis, quantitative and reproducible evaluation of the levator ani kinesiologic function is difficult. The levator ani muscles are attached to the bony surfaces of the pelvis, which hinders the measurement of an isometric contraction in a reproducible manner. These data demonstrate that pelvic floor muscle strength increases with exercise training, which is consistent with previous studies that have determined quantitative increases in perineometry,17 digital pelvic muscle strength scores,30,31 and gross vaginal electromyographic activity24,31 with PFMT. The variations in quantitative alterations reported in these studies no doubt reflects variations in training regimens and recording techniques.
Maximal contractions of skeletal muscle increase strength by a combination of an increase in the efficiency of motor unit activation and hypertrophy of type I (slow-twitch) and type II (fast-twitch) muscle fibers,32 which lead to an increase in muscle volume. The pelvic floor musculature is uncommon in that it is the only group of voluntary muscles except for the respiratory diaphragm in which type I fibers predominate.10 The mechanism of efficacy of PFMT is unknown, but it is logical that hypertrophy of the striated levator ani33 with concomitant increases in kinesiologic function should improve continence by increasing bladder outlet resistance during physical stress and during moments of urgency and inappropriate detrusor activity. Studies of muscles outside of the pelvis in elderly women have demonstrated that strength training preferentially increases the diameter of type I fibers with no alteration in the ratio of fiber types within the muscle. In addition to the absolute strength of a pelvic floor muscle contraction, it is possible that the timing of the contraction can affect leakage during physical stress17 or urge.
Response to PFMT may in part depend on alterations in neurophysiologic performance of the neuromuscular unit. Studies of muscles outside the pelvis demonstrate that training increases the efficiency of neural activation,34 and in middle-aged and elderly subjects, increases in muscle strength seem to depend more on increased motor unit activation than on muscle fiber hypertrophy.35 This type of electromyographic testing has not been used to evaluate pelvic floor muscle response to training. Given that pelvic floor musculature has a high proportion of type I (slow-twitch) muscle fibers, it is likely that improvements in resting pelvic floor muscle tone are important in improving continence during daily activities.
Clinical Studies of Pelvic Floor Muscle Training Programs
Few researchers have analyzed the results comparing strength increase or maximal strength with improvement in urinary incontinence after training, and the results of the few published studies are contradictory. Dougherty and colleagues,36 Hahn and coworkers,37 and Boyington and associates38 did not find any correlation between a change in pelvic floor muscle strength and urine loss. However, modifying their analysis, Boyington and colleauges38 found an association between a decrease in urine loss variables and increases in pelvic floor muscle pressure curve variables.
Conflicting results have been shown in case-control studies measuring pelvic floor muscle strength in continent and incontinent women. Some researchers have shown a significantly higher degree of pelvic floor muscle strength in continent women.39–41 In other studies, no differences have been demonstrated.36,42 The conflicting results may reflect small sample sizes, use of unreliable and insensitive outcome measures, and use of unreliable and insensitive methods to measure pelvic floor muscle strength.
We43 demonstrated that intensive PFME combined with weekly group training was significantly more effective than the same exercises conducted at home. Because all women participating in this study had learned to contract the pelvic floor muscle correctly and had had the same monthly individual follow-up with measurement of pelvic floor muscle strength, development of muscle strength could be analyzed by combining results from responders and nonresponders from both groups. Another justification for analyzing all participants together is that the study is not looking for treatment effect but instead seeks the relationship between pelvic floor muscle strength and other outcomes.
There is no consensus about which outcome measure to choose for assessing cure or how to classify a responder to treatment for incontinence. However, combinations of subjective report and laboratory measurement of the condition have been recommended.44,45
In the few published studies in this area,46 different methods have been used to evaluate pelvic floor muscle function and showed that urine loss decreased as pelvic floor muscle function increased. Boyington and colleagues,38 measuring vaginal squeeze pressure, did not find a correlation between an increase in muscle strength and improvement in leakage.
To achieve reduction of urinary leakage by PFMT, the training has to be of sufficient intensity, frequency, and duration to cause a significant change in muscle function.47 The intensity of the contraction is the most important factor in developing muscle strength.32 To improve the neural adaptation (i.e., recruitment of efficient motor units and frequency of excitation) and hypertrophy, the training period should be at least 5 months.48 Lack of or insufficient improvement in muscle strength after PFME may explain why some researchers have failed to find significant differences between methods49,50 or correlation between the independent and dependent variables.37
Several studies have demonstrated that more than 30% of incontinent women are unable to contract the pelvic floor muscle correctly.30,51 Bump and coworkers51 showed that only 49% of the women able to contract the pelvic floor muscle performed a contraction effective enough to increase urethral pressure.
This may explain who some researchers have failed to find a correlation between increased vaginal pressure and reduction of leakage. Measurement of voluntary contraction in a supine position may not be a valid assessment of automatic co-contraction during an increase in abdominal pressure in an upright position. One study52 investigated the effect of two approaches to PFMT in stress incontinent women (N = 128). It is common practice for women to receive instruction in strength training combined with advice to voluntarily contract the pelvic floor muscles to prevent leakage with increases in intra-abdominal pressure (e.g., cough). The use of a voluntary contraction before an increase intra-abdominal pressure, called the knack, and is based on motor relearning principles.
The confidence intervals for the difference in leakage episodes and cough test do not rule out clinically important differences. Despite an attempt to design a study of adequate power, a larger trial is needed to address the question of important differences between these two approaches to PFMT. One study53 was undertaken to determine the degree to which complete loss of the pubococcygeal muscle affected women’s ability to volitionally augment their urethral closure pressures by using a volitional pelvic floor muscle contraction (i.e., Kegel effort). The sample consisted of a subset of women who volunteered as healthy controls in a larger study approved by an institutional review board. They were free of urinary leakage or prolapse and had a negative stress test result. Multiplanar, proton-density magnetic resonance images of the pelvis were obtained in all women. A trained observer evaluated each scan to determine pubococcygeal muscle status. Women were selected for analysis if they demonstrated an intact pubococcygeus muscle (n = 28; mean age, 54 years) or absent pubococcygeal muscle (n = 17; mean age, 59 years). Women with parietal defects (e.g., one side only) were excluded. Women were then asked to perform two or three Kegel efforts while the transducer was held at the point of maximal urethral closure pressure. The investigators concluded that women with an absent pubococcygeal muscle are only one half as likely to be able to increase their urethral closure pressure more than 5 cm H2O and generate 43% less pressure with pelvic muscle contraction compared with women with normal women muscle training.
BIOFEEDBACK THERAPY
As described in the Chapter 19, biofeedback can be defined as the use of monitoring equipment to measure internal physiologic events or various body conditions of which the person is usually unaware. The basic approach is to provide individuals with information about the physiologic activities in their bodies, including their brains. These include sensors (i.e., electromyographic and pressure sensors) for detecting and measuring the activity of anal or urinary sphincters and pelvic floor muscles. Techniques have been also developed to measure activity of urinary stress incontinence. One aim of physical therapy has always been to assist patients by improving physiologic self-regulation within their natural environment.
Pelvic Floor Muscle Biofeedback
Several approaches have been used for measuring pelvic floor muscle activity to provide biofeedback, including urethral, vaginal, or anal feedback using manometry or electromyography. An important technical issue is the quality of the signal source used for feedback. As early as the 1940s, Kegel28,54 developed and used the perineometer, an instrument that consisted of an intravaginal balloon attached to an external pressure gauge, which registered the pressure exerted by the pubococcygeus muscles. It was the first biofeedback device for PFMT. This method uses manometry (pressure) biofeedback by means of an intravaginal or intrarectal device. An advantage of pressure manometry is that as the patient contracts her pelvic floor muscles, the device produces a resistive pressure that may give additional feedback to the patient. After the vaginal manometry method, electromyography emerged for recording pelvic floor muscle activity. Different signal sources have been used, but electromyographic activity has evolved as the preferred signal source for many types of biofeedback therapy.55
Electromyographic activity of pelvic floor muscle contractions has become a common signal source for the treatment of urinary incontinence.56 Vaginal electromyographic activity is recorded by means of surface electrodes in the vaginal introitus or a vaginal probe with electrodes embedded. The vaginal probe is easy to insert and remove, and it is usually comfortable.
Biofeedback of the urethral or anal sphincter or pelvic floor muscles is used in the management of urinary incontinence and voiding difficulties. The external anal sphincter and the external urethral sphincter have similar innervation through branches of the pudendal nerves. Although there are conflicts in the literature about the issue of correspondence between the anal and urethral sphincters, several studies indicate that these muscles act in concert,57 and data indicate that training and controlling the anal sphincter results in urinary sphincter activity that corresponds in magnitude.58 Anal sphincter activity can be measured by pressure balloons located by the external anal sphincter (for manometry) or by surface electrodes placed around the anus at the 10-o’clock and 2-o’clock positions.
Electromyographic activity can be measured by electrodes embedded in a rectal probe. The electromyographic instruments are designed to detect the weak electrical signals generated during muscle contraction. Surface electrodes are electrically conductive pathways in contact with the skin (over abdominal muscles) or mucosa (vaginal or anal tissue). Continuous monitoring of the electromyographic signal is important to ensure that there is no undetected signal interference and that electrode placement provides an appropriate signal. Correct placement of surface electrodes is fundamental to detect and measure a signal accurately. The three common signal sources (bladder pressure, anal sphincter pressure, and vaginal electromyographic activity) are signi-ficantly altered by increases in intra-abdominal pressure. Simultaneous measurement of abdominal activity should be done with all biofeedback therapy techniques. Intra-abdominal pressure can be measured easily using an internal rectal balloon. Electromyographic activity of the rectus abdominis muscles can be determined by surface electrodes. The abdominal muscle activity is displayed by means of two active electrodes placed 3 cm apart just below the umbilicus. A ground electrode is placed on a convenient bony prominence, such as the iliac crest.59–61
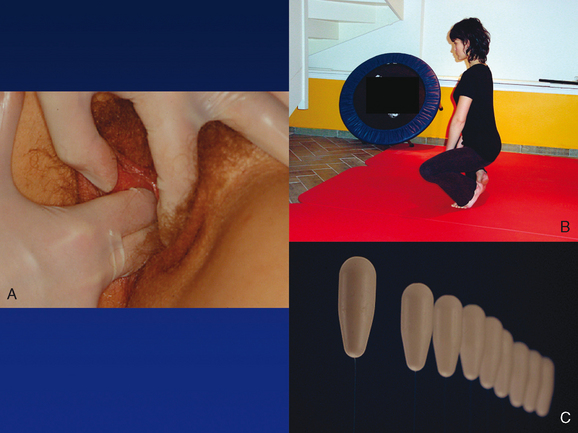
Electromyographic biofeedback training is used to increase the activity of weak muscle groups and to promote relaxation of spastic or tense muscles.62 In the case of urinary stress incontinence, the function required is to assist the urethral closure pressure provided by the urethral sphincter. This requires a quick, maximal voluntary contraction of the pelvic floor muscles, and the training program must emphasize type II fibers. However, the contribution of type I fibers should not be overlooked. They are responsible for maintaining the postural position of the pelvic floor, from which type II fibers can function effectively (Fig. 28-1).
Clinical Practice and Techniques
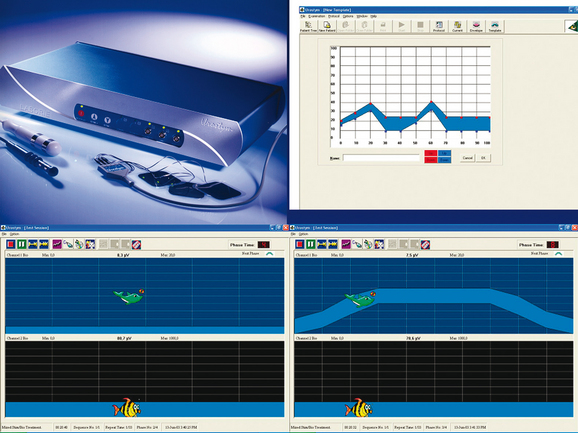
Using three-channel biofeedback, patients are taught to contract and relax pelvic floor muscles selectively without increasing bladder pressure or intra-abdominal pressure. In our practice,62–64 my colleagues and I use a microcomputer-based system with a wide range of parameters that allows us to regulate the treatment according to the specific requirements of the patient, especially in daily activities. The system records simultaneous measurements of electromyographic activity of the pelvic floor muscles, rectus abdominis muscles, and other skeletal muscles (e.g., gluteal, adductors).
In clinical practice, I use pelvic floor therapy systems, which include products for home-based and office-based treatments and provide the most comprehensive and advanced platforms for treatment of pelvic floor dysfunction. The available equipment typically ensures effective treatment outcomes for most patients. The most important features are adjustable color and screen configuration, session graphs with summaries of data, audio and visual goal setting, annotated markers, templates, and animation (see Fig. 19-5 and 19-6 in Chapter 19). Using such equipment, it is possible to provide more enjoyable exercise programs (i.e., various levels of difficulty) and to conduct statistical analyses (Fig. 28-2).
Muscle Strengthening
The pelvic floor muscles hold the pelvic organs like a hammock, providing support and stabilization. Normally, when the woman is erect, the levator ani muscles, together with the respective fasciae, contribute to the support of the vaginal canal, urethra, and rectum. In patients with pelvic relaxation, this normal muscular support is lost. The levator ani hiatus is wider, and the levator plate is weakened and relaxed. When the pubococcygeal portions of the levator ani sling contract, they shorten lengthwise, gaining thickness and lessening the pelvic floor aperture transversely, thereby reducing the anteroposterior diameter considerably.65 A tonic contraction of the levator ani maintains a high position of the vesical neck and may compensate for an increase in intra-abdominal pressure. The levator ani support66 is provided predominantly by slow-twitch fibers, which are responsible for maintaining static muscle tone. During stressful events, phasic fast-twitch fibers provide a rapid forceful contraction.67,68 When muscles have weakened, there is little perception of the contraction because the intensity of the proprioceptive feedback to the brain is relative to the amplitude of the muscle contraction. Muscle strength can be improved through a program of PFMEs.
In planning a PFME program, it is important to follow some basic guidelines. Patients should be selected according to grades of the pelvic floor muscles. A trained therapist should be present to give proper instruction about the level of contraction, and the exercise program should be tailored to the individual. Body positions should be modified after several sessions, and types of contraction should be alternated. During exercise sessions, it is important to recruit fast-twitch fibers by fast contractions to develop strength and recruit slow-twitch fibers by slow contractions to increase endurance.67 Regular strength training increases the number of activated motor units, frequency of excitation, and muscle volume. To induce hypertrophy, both fast- and slow-twitch fibers should be contracted. To achieve these objectives, a successful PFMT program must include rapid forceful con-tractions, sustained maximal voluntary contractions, and fast contractions superimposed on the end of each prolonged contraction.
Effective strength training relies on specificity (i.e., co-contraction of other groups of muscles such as the glutei and hip adductors should be minimized) and overload (i.e., increasing length and duration of contractions and reduction of rest periods). The only anatomic relationship between the levator ani and the other pelvic floor muscles is provided by the obturator internus. The pubococcygeal segment of the levator ani originates in the tendinous arch, a thickening of the obturator fascia; the iliococcygeus begins at a membranous insertion to the inner surface of the obturator internus at the tendinous arch of the levator ani.68
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree