Fig. 2.1
Outer port/cannula of a 10 mm dilating/non-cutting trocar
All modern trocars generally include a gas-tight valve, which allows for removal and introduction of instruments without the loss of pneumoperitoneum. In addition, new valveless trocars have been introduced that use the pressurized curtain of gas at the top of the instrument to reduce carbon dioxide leakage. There exists a variety of single-use and reusable laparoscopic trocars. Although reusable trocars may have advantages in terms of cost, with use their tips may become blunt and valves may become incompetent.
Trocar sizes range from 3 mm to 30 mm, with the size referring to the inside diameter. The 5, 8, 10, and 12 mm trocars are the most commonly used in advanced laparoscopic and robotic colorectal surgery. The trocar itself is made of an inner, removable obturator and outer port or cannula (Fig. 2.2), which remains in place for the passage of instruments. The sleeve may be metal, plastic, smooth, and/or threaded. The transparent trocars have the advantage of allowing the laparoscope to monitor the trocar as it passes through the abdominal wall. While metal trocars are more durable, they run the risk of capacitive coupling, resulting in unintentional thermal spread and injury, with improper use of energy devices such as the electrocautery.


Fig. 2.2
Multiple ports used in one case: robotic ports and two varieties of laparoscopic non-cutting dilating trocars
The trocar can be further categorized into cutting or dilating trocars. Cutting trocars can be metal or plastic and cut through the tissue as force is applied. There are designs that include a spring-loaded plastic shield that are intended to automatically cover the blade as it enters the abdominal cavity. The dilating trocars use a blunt, tapered tip that separates and dilates the tissue as it is inserted. The cutting trocars can decrease the amount of force required to enter the abdomen compared to the blunt-tipped dilating trocar. Although easy to insert, these bladed trocars were initially associated with occasional vascular and visceral complications, as well as abdominal wall hematoma, trocar site pain, and hernia. The newer-generation retracting tips seem safer but have not been proven to have a better safety profile [5]. Blunt tip/dilating trocars require a smaller skin incision and stretch the remaining abdominal wall, rather than incising, which may result in improved retention. The dilating trocars have been associated with decreased postoperative pain, port-site bleeding, smaller scars, and increased patient satisfaction. In summary, radially dilating trocars require an increased insertion force and have a smaller defect size compared to cutting trocars [6, 7]. Our preference for colorectal surgery is a variety of blunt tip/dilating 5, 10, and 12 m trocars to minimize risk to bowel and abdominal wall.
Instruments
Laparoscopic instrumentation is continuously evolving with new technology allowing for better ergonomics and tissue handling. Multiple companies manufacture the laparoscopic instruments; however, the principles remain uniform.
Camera/Laparoscope
Adequate visualization is an essential aspect of laparoscopic surgery. There is a wide range of available laparoscopes with regard to diameter and viewing angles. There are also flexible tip laparoscopes, which are advantageous in providing versatility in the angle viewed. Laparoscopes can be classified as a telescopic rod lens system, which are connected to a video camera, or a digital laparoscope with an integrated light source. Camera processor unit, light source, recording device, and monitors with articulating arms should be available (Fig. 2.3). Recently, high-definition scopes have become available. Individual choice of cameras is often dictated by surgeon preference and the hospital purchasing body or Value Analysis Committee. Regardless of which camera is used, it is important to test the camera and light source prior to gaining access to the abdomen as well as to “white balance” the camera for optimal color resolution. Typically, the surgeon stands on the opposite side of the abdomen from the pathology (and thus the expected resection segment), and the laparoscope points toward the pathology. A laparoscopic warmer and antifog solution should be available to allow for enhanced visualization. In many cases, the most junior member of the operative team is charged with “driving the camera.” Unfortunately, this often results in unnecessary confusion in the anatomy, lack of unity during the case (i.e., focusing in on a different viewpoint), prolonged operations, poor ergonomics, and overall increased frustration. The traditional guidance to “keep the camera buttons toward the ceiling” is ill advised and incorrect in colorectal surgery. Rather, proper education regarding recognition of the horizon and maintaining camera orientation to identify the correct field of view is crucial for colorectal operations, especially when transitioning between the various abdominal quadrants.


Fig. 2.3
Camera light source and video unit
Insufflator
Once abdominal access is gained, pneumoperitoneum is essential in providing adequate visualization and space to perform the operation. This is achieved via an insufflator. At the beginning of each case, prior to the incision, assure that the insufflator is working. Turn the insufflator on and check carbon dioxide cylinders to ascertain that adequate gas is available for the case. Always have an extra available container, as inevitably the tank will run out at a crucial moment if not prepared. Advanced, integrated surgical rooms will often have carbon dioxide lines directly attached to the insufflator, thus obviating the need for a tank. The insufflator will display the intra-abdominal pressure and contain an adjustable pressure selector and digital flow and volume displays. Once pneumoperitoneum is established, the setting should be placed on high flow (20–40 L/min), typically to achieve a steady 15 mmHg pneumoperitoneum. Select patients with cardiopulmonary issues may require lower levels of abdominal pressure to be maintained. The anesthesiologist will monitor the patient’s hemodynamics during insufflation, and it is important to continue good communication.
Graspers
Laparoscopic graspers represent the most varied yet most used type of instrument in laparoscopic colon surgery. They can be reusable or disposable and can have various types of handles, insulated shafts, and tips. Some versions can also have attachments for monopolar cautery. Diameters range from 1.8 to 12 mm, and lengths range from 30 cm upward. We prefer 5 mm, 30–35 cm length instruments for our average patients. However, 45 cm or even longer instruments should be available and are typically used when mobilizing the splenic flexure. The type of grasper used will be dependent on the task. Surgeon preference is key with regard to the handle of the instruments. A ring handle offers a greater precision compared to the diamond or pincer grip. However, handles that allow for a greater form of a palm grip can be used for tasks involving power over precision (Fig. 2.4). Certain graspers may also have a locking mechanism, which is ideal when position of the grasper must be maintained for a prolonged period of time.


Fig. 2.4
Handles of different instruments, demonstrating that ring handle offers a greater precision (a) secondary to the pincer grip compared to handles (b) that allow for a greater form of a palm grip can be used for tasks involving power over precision
Graspers used for bowel retraction should allow for a secure grip, without exerting excessive pressure. A variety of tips, including straight or flared, traumatic or atraumatic, single or dual, and fenestrated or solid, are available. To decrease traction injury, we prefer atraumatic fenestrated graspers (Fig. 2.5) with dull dual ends for most bowel retraction and bowel handling. Dual action is preferred, since single action type graspers with one movable jaw exert greater pressure on the tissue. Fenestrated tips exert less friction on grasped tissue, which also means they can be prone to slippage on the tissue. Care should be taken not to exert too much pressure, especially in directions perpendicular to the tip orientation. It is also pertinent to remember that the tip of the grasper, given its smaller surface area, exerts the greatest force. When retracting with the tip, avoid pushing blindly or excessively into the bowel wall to prevent inadvertent enterotomies.
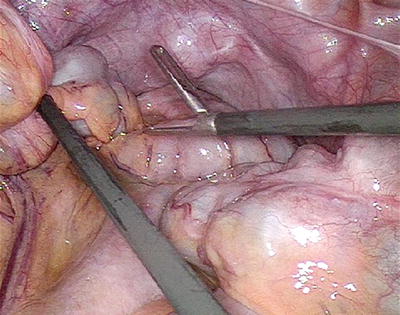
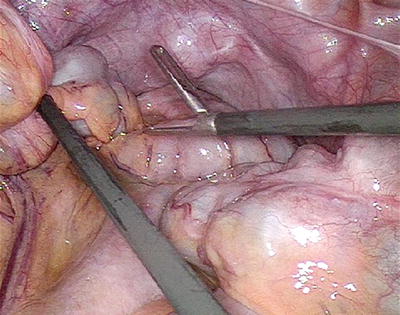
Fig. 2.5
Fenestrated nontraumatic graspers, used for grasping bowel
Dissector graspers, such as Maryland graspers, and right angle graspers should be available for blunt dissection as needed but are generally not to be used for handling the bowel.
Scissors
Laparoscopic scissors are also available as reusable, reposable (e.g., the tip is disposable while the shaft is reusable), or disposable. They can be used for sharp dissection and, with care, limited blunt dissection. In patients with prior abdominal surgery, scissors are invaluable with taking down adherent loops of bowel to the anterior abdominal wall. Monopolar cautery can be attached, allowing for use of energy during dissection for better hemostasis. Similar to graspers, these instruments are available in a variety of sizes and lengths.
Laparoscopic Staplers
There are a variety of surgical stapling devices available on the market. Laparoscopic staplers can be used in lieu of energy devices or suturing for vessel ligation, as well as in the creation of anastomoses. Large prospective randomized trials have failed to demonstrate superiority of either stapled or hand-sewn anastomoses [8, 9]. The linear stapler (e.g., laparoscopic GIA) places 4 staggered rows of titanium staples and then divides the tissue between the staple lines. The device failure rate has been reported as 0.2–0.3 % [10, 11].
The appropriate stapler should be selected based upon the required function. Staplers are also classified into linear versus circular staplers, articulating versus straight, and cutting versus non-cutting. Staplers are also offered in a powered design (Video 2.1). Theoretically, powered staplers may optimize stapler deployment thereby achieving superior tissue apposition. However, to date no studies have validated their superiority. Cartridge length is variable for the staplers and is generally available in 30–60 mm lengths, and appropriate size should be selected to decrease the number of staple lines. However, shorter cartridges may be easier to deploy in the narrow pelvis.
Staples come in a variety of heights (2–5 mm) and are color-coded based upon the height. There is no uniform color-coded standard for labeling the stapling heights, and each manufacturer has their own color code. Height should be chosen based upon the tissue thickness. Failure to choose an appropriate height may result in incomplete tissue apposition or conversely inadequate compression of tissue (Fig. 2.6a) [12]. Ideal staple height selection to match the tissue thickness should result in formation of a “B” shape of the staples (Fig. 2.6b). The rectum, which is typically thicker than the colon, should be divided with at least a 4.0 mm staple, while the small bowel and colon can be stapled with ~3.5 mm staples. Staple line buttressing is also available with a variety of reinforcement material, though various studies have failed to show a significant difference in outcomes, and in our general practice, we do not use reinforcement [13].
Fig. 2.6
(a) Failure to choose an appropriate height may result in incomplete tissue apposition or conversely inadequate compression of tissue. (b) Ideal “B”-shaped staple configuration. With Permission from Davis B, Rafferty JF. Technical Aspects. In: Steele SR, Maykel JA, Champagne BJ, Orangio GR, eds. Complexities in Colorectal Surgery: Decision-making and management. Springer, New York, 2014 © Springer in 2014
Low anterior resection (LAR) can pose specific challenges to the surgeon, notably during division of the rectum. Division low in the pelvis can be challenging in terms of both articulation of the stapler and in the length of the staple line, especially in a narrow pelvis. A curved stapler has recently become available for bowel division, and one study has demonstrated feasibility and safety [14].
Other Laparoscopic Instrumentation
Laparoscopic instruments that should also be available include needle driver for intracorporeal suturing, suction/irrigator device, and clip appliers for control of vessels. Clip appliers are indicated for ligation of appropriate size vessels or ducts. Clips vary in lengths (6–11 mm) and material (metallic or nonabsorbable plastic). They are available offered as disposable or reusable, and shaft diameters range from 5 to 11 mm.
Energy Devices
Adequate hemostasis is key in any surgical procedure and is critical in laparoscopic surgery. The rapid control of vessels and hemorrhage will allow for maintenance of visualization and for the procedure to continue laparoscopically. However, hemostasis remains a challenge in laparoscopic surgery, given that traditional methods of controlling/dividing a vessel (i.e., suture ligation) is technically challenging in the laparoscopic setting; therefore, we have come to rely more heavily on surgical clips and staplers. However, these devices do have limitations in function. The surgical evolution of energy devices has become central in the laparoscopic era, for they allow for rapid control and division of named vessels. A general understanding of principles and knowledge of the advantages and complications of energy devices should be appreciated by all users.
Monopolar Energy
Monopolar energy relies on electrical current flowing from the generator through the patient and return via a grounding pad. It can be used to facilitate dissection, achieve hemostasis, and ligate small vessels. Devices such as scissors, hook cautery, or graspers can be utilized, and the energy can be set as cutting or coagulation. Similar to monopolar “Bovie Electrocautery,” advantages include speed, low voltage, and rapid hemostasis. It is important to recognize, however, that standard monopolar devices rely on heat and time to perform their duty. They also require the circuit to be intact. Inadvertent alternate site burns can occur if energy is allowed to complete the circuit outside of the designated grounding pad. Other disadvantages to standard monopolar energy include an increased lateral thermal spread when compared to the bipolar devices. This may be critical when dissecting in confined spaces adjacent to critical structures such as the pelvic plexus during the anterior portion of an LAR, where thermal damage to the nerves may have long-term consequences.
Bipolar Energy
Traditional bipolar energy still relies on using electricity to perform its function. Unlike monopolar energy, bipolar energy requires no grounding pad, as the circuit is completed between the two instrument tips adjacent to one another. This results in a higher degree of current density at the tissue between the tips of the instrument. Advanced bipolar energy systems (i.e., LigaSure™, Covidien, CT, and Enseal™, Ethicon, Cincinnati, OH) add in the third component of vessel sealing (along with heat and time)—compression. This allows lower voltage to be used and, hence, lower heat to complete much larger tasks. Bipolar energy is used in a variety of vessel sealing devices and delivers a much smaller lateral thermal spread footprint. This energy, combined with the increased pressure delivered by the jaws of the instrument, allows for permanent sealing of up to 7 mm vessels (Video 2.2). The size of the vessel and thermal spread is variable depending on the instrument (Table 2.1). Many of these instruments are shaped in a blunt-tipped, versatile fashion. The advantage of bipolar devices is that these instruments can be used to grasp, dissect, and coagulate, thereby reducing the need to change instruments.
Device | Company | Thermal spread (mm) (reported) | Vessel seal (mm) |
|---|---|---|---|
Enseal Trio® | Ethicon | 1 | 7 |
Trissector PKS™ | Gyrus | 3.6 | 7 |
LigaSure™ | Covidien | 0–4.5 | 7 |
HALO PKS™ | Olympus | – | 7 |
OMNI PKS™ | Olympus | – | 7 |
Ultrasonic Energy
Devices such as Harmonic Scalpel® (Ethicon, Cincinnati, OH) and SonSurg® (Olympus, Southborough, MA) use ultrasonic technology. In essence, these devices convert electrical energy at the generator into mechanical motion at the jaw blade. Unlike monopolar and bipolar instruments, no energy flows through the patient. In fact, these instruments are more in line with surgical staplers than they are with the advanced bipolar devices. Yet, these devices can still reproducibly and reliably seal vessels ≤5 mm with minimal thermal damage, and newer models are FDA approved up to 7 mm vessels [15]. They only have one active blade that can be rotated. Depending on several factors such as the power setting at the generator, “max” or “min” activation at the device and degree of tissue tension applied by the user will all determine which end of the coagulation versus cut spectrum the device will function. These devices also have the advantage of serving multiple purposes (i.e., cut, coagulate, coapt, cavitate) and thereby eliminating the need to change instruments (Video 2.3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








