Fig. 7.1
Positioning of the patient on a split-leg table
The surgeon should confirm that all equipment is either in the room or is readily available (Table 7.1). A 30° angled laparoscope is used to look over the horizon of the operative field; this scope is more versatile than a standard 0° scope. Additional suggested equipment includes a colonoscope (CO2 insufflation is preferred over ambient air) and lighted handheld deep pelvic retractors that facilitate pelvic dissection through the hand-port access. In general, disposable devices (hand port, energy device, and suction irrigator) are not opened until the surgeon enters the abdomen and confirms the feasibility of a hand-assisted approach.
Table 7.1
Equipment
• 5 mm 30° laparoscope |
• Trocars (5 mm × 4), hand-access port |
• Laparoscopic blunt atraumatic graspers and scissors |
• 5 mm blunt tip LigaSure™ (Covidien, Mansfield, MA) or other energy device, per surgeon preference |
• Bowel stapler with appropriate loads |
• End-to-end stapling device (appropriate sizes available) |
• Colonoscope with carbon dioxide insufflation device |
• Standard laparoscopic instrumentation (i.e., atraumatic graspers, Maryland dissector, etc.) |
Procedure Steps
Hand-Assisted Left Colectomy (Videos 7.1, 7.2, and 7.3)
Port Placement
Hand-port placement: A Pfannenstiel incision placed two fingerbreadths above the symphysis pubis is used for the majority of patients. In patients with prior lower midline incisions and in patients considered at higher risk of conversion, a lower midline incision is typically used. When dissecting through the subcutaneous fat down to the fascia through a Pfannenstiel incision, avoid skiving towards the symphysis pubis as placing the port too close to the pubis may restrict access through the port and may cause the hand port not to sit well. Adequate flaps must be created between the anterior rectus sheath and the rectus muscle to ensure sufficient space for the operating surgeon’s hand. Once the abdomen is entered, inspection of the field and palpation through the wound allows the surgeon to determine whether or not to proceed in hand-assisted fashion. If confirmed, a reusable 5 mm camera port is then placed near the umbilicus with the surgeon’s hand within the abdomen protecting the viscera, and the abdomen is insufflated. Two additional 5 mm working ports are placed under direct laparoscopic visualization in the left lower quadrant and right lower quadrant lateral to the inferior epigastric vessels (Fig. 7.2). Once the ports are placed, and before the dissection is begun, the abdomen is surveyed and thoroughly explored for any abnormalities (metastases, adhesions, injury due to port placement, etc.).
Fig. 7.2
Hand-assisted device and port site placement for a left colectomy
In patients likely to have adhesions from prior surgery that might interfere with hand-assisted colectomy, it may be preferable to place upper quadrant ports to evaluate the adhesions and to potentially perform adhesiolysis to allow hand-port placement.
A laparotomy pad (with an attached radiopaque ring) is placed within the abdomen prior to securing the hand-port device. The pad facilitates exposure by keeping the small bowel out of the field, keeping the operative field dry, and allowing the surgeon to clean the scope without actually removing the scope from the abdomen. In order to reduce the risk of a retained foreign body, a hemostat is placed on the surgeon’s surgical gown as a reminder that a laparotomy pad is within the abdomen. When the pad is removed and handed back to the scrub nurse, the hemostat is handed back as well.
Left Colon Dissection
Mobilization of the splenic flexure: In the majority of cases, the splenic flexure will need to be mobilized to ensure a tension-free colorectal anastomosis. In order to decrease the risk of splenic injury, care should be taken to avoid undue traction on splenic attachments during the mobilization. Manipulation of the splenic flexure mesentery must also be done carefully, as injury to the marginal artery may compromise the vascular supply to the bowel being used for the anastomosis. There are several ways to approach taking down the splenic flexure (medial at the inferior mesenteric vein (IMV), lateral up the left paracolic gutter, entering the lesser sac at the midline). Typically, and especially in cases with an extreme splenic flexure, a combination of all three approaches is utilized to mobilize the flexure all the way to the ligament of Treitz.
Medial-to-Lateral Approach at the IMV
This is the preferred approach to the flexure because it allows relatively easy mobilization of the colon and mesocolon up off of the retroperitoneum, while the lateral-to-medial approach requires the surgeon to dissect in a plane while looking up over the horizon. Placing the patient in reverse Trendelenburg position with the table tilted right side down allows the small bowel to be placed in the right side of the abdomen and aids in exposing the anatomy. The assistant stands on the right side of the patient holding the camera and using a grasper through the right-sided port to retract the greater omentum and transverse colon cephalad over the liver exposing the paraduodenal fossa with the left colon mesentery and ligament of Treitz (Fig. 7.3). The surgeon, standing between the legs with the left hand in the abdomen and the energy device in the left-sided port, should appreciate the location of the aorta, the 4th portion of the duodenum, and the IMV. The intra-abdominal laparotomy pad helps to keep the small bowel out of the field of dissection. The peritoneum overlying the paraduodenal space is incised and a retromesenteric plane is developed in medial-to-lateral fashion (Fig. 7.4). This peritoneum should be taken sharply to avoid using energy so close to the duodenum. The retroperitoneum including the ureter, the gonadal bundle, and Gerota’s fascia are pushed dorsally and the mesocolon is swept ventrally. If the correct plane is entered, this dissection is relatively avascular. This dissection is carried as far laterally to the abdominal wall as possible and cephalad to the inferior border of the pancreas. Care should be taken to avoid dissecting behind the pancreas or into the retroperitoneum as this can jeopardize the retroperitoneal structures. Once this dissection is completed, the IMV can be divided using the energy device.

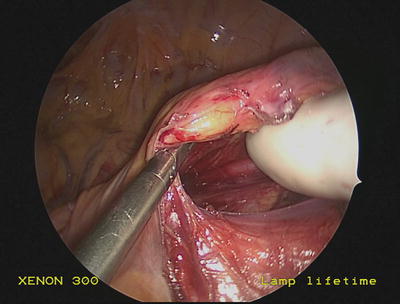

Fig. 7.3
Paraduodenal fossa at the ligament of Treitz demonstrating the inferior mesenteric vein (IMV)
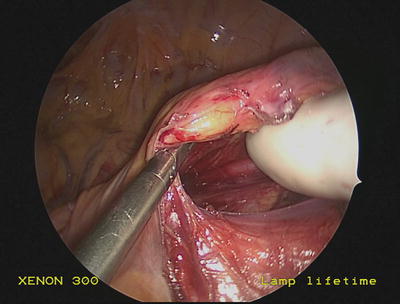
Fig. 7.4
Medial-to-lateral dissection at the IMV in the avascular plane
The greater omentum is retracted anteriorly and cephalad by the assistant and the transverse colon is retracted caudally by the surgeon. This retraction facilitates exposure to enter the avascular plane that separates the greater omentum from the transverse colon and mesocolon (Fig. 7.5). This dissection, most easily started near the midline at the falciform ligament, enters the lesser sac and is carried laterally towards the splenic flexure (Fig. 7.6), fully releasing the omentum, which can now serve as an omental pedicle flap. During the dissection, the surgeon’s left hand protects the colon and the stomach from collateral damage from the energy device. As the dissection progresses along the left transverse colon, it is important to use tissue triangulation to actually see the colon as it courses cephalad into the left upper quadrant at the splenic flexure; this helps prevent injury to the colon.

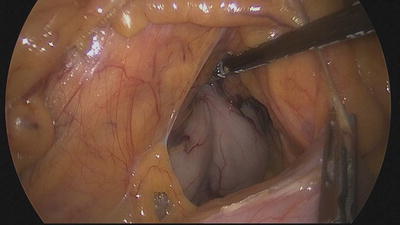

Fig. 7.5
Entering the lesser sac near the midline
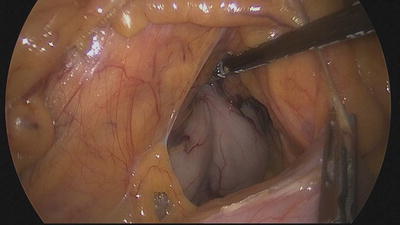
Fig. 7.6
The lesser sac is entered—notice the back wall of the stomach
While the left colon is gently retracted by the assistant grasping an epiploica, the surgeon’s left hand is placed into the retromesenteric space and is used to demonstrate the plane of dissection. Using the energy device through the left-sided port, the colon is released from its lateral attachments (commonly referred to as the white line of Toldt), and the retromesenteric dissection plane that had been mobilized previously in medial-to-lateral fashion is entered. The dissection is carried cephalad towards the splenic flexure (Fig. 7.7). The mesocolon is dissected free from the inferior border of the pancreas, completely releasing the splenic flexure. Once the left colon is mobilized, the surgeon performs a sweep with his hand to confirm the colon is completely mobilized from the retroperitoneum, the omentum, and the spleen, as persistent attachments can jeopardize reach to the pelvis and the ability to exteriorize the specimen.










