Chapter 30 OUTCOME MEASURES FOR PELVIC ORGAN PROLAPSE
Developers of outcome measures for pelvic organ prolapse are faced with the difficult task of addressing a wide range of symptoms from the bowel, bladder, and uterus. Historically, instruments were developed that addressed a single organ, but they have progressed to validated tools that include information relating to all three organs. The modern tools should be completed as part of the patient’s medical record, along with the physical examination and diagnostic tests. They can be performed before and after medical or surgical treatment. They are an essential part of the clinician’s and researcher’s tools in partnership with diagnostic tests.
This chapter describes commonly used validated tools developed specifically for women with pelvic organ prolapse and related symptoms. The instruments can be broadly classified as those that quantify and stage prolapse and those that quantify the range of symptoms associated with prolapse. Some scales, such as the Pelvic Organ Prolapse Questionnaire (POP-Q),1 provide a means of accurately describing the position of the organs relative to one another and the amount of relative descent of each of the organs. Others provide a means of assessing the wide range of urinary tract, bowel, sexual, pain, and quality-of-life symptoms related to prolapse. Some symptom scales are comprehensive measures that try to address all symptoms resulting from bowel, bladder, and uterine prolapse. Others are focused scales that ask detailed questions about a single complex, such as sexual dysfunction.
QUANTIFYING AND STAGING PROLAPSE
Researchers and clinicians recognized the need for a more comprehensive staging system that included all the pelvic organs. Although some of the older scales, such as the traditional four-stage classification system,2 are still in limited use, the POP-Q is the most widely recognized internationally.3–6
Pelvic Organ Prolapse Questionnaire
The POP-Q provides a descriptive and quantifying system for the relative position of the organs within the pelvis and enables objective staging of pelvic prolapse. The system, adapted from several classifications by Baden and Walker,7 was developed by the International Continence Society Committee on Standardisation of Terminology, Subcommittee on Pelvic Organ Prolapse and Pelvic Floor Dysfunction, in collaboration with the American Urogynecologic Society and the Society of Gynecologic Surgeons.1 The POP-Q system arose from the efforts of the committee to develop a terminology standardization document. The original document was drafted in 1993 and refined in 1994. In 1994, it underwent a 1-year review and trial, during which time several minor revisions were made.
Reproducibility studies for the POP-Q were conducted in six centers in the United States and Europe, documenting interobserver and intraobserver reliability and clinical utility of the system in 240 women.8–12 Interobserver reliability was studied in 48 women with a mean age of 61 ± 14 years, parity of 3 ± 2, and weight of 74 ± 31 kg. Correlations for each of the nine measurements (r = 0.817, 0.895, 0.522, 0.767, 0.746, 0.747, 0.913, 0.514, and 0.488) were highly significant (P = 0.0008 to <0.0001). Staging and substaging were reported to be highly reproducible (taub = 0.702 and 0.652, respectively). In 69% of subjects, the stages identified were identical, and in the re-mainder, they did not vary by more than one stage among observers. Intraobserver reliability was studied in 25 women. Correlations (r) for the nine measurements were 0.780, 0.934, 0.765, 0.759, 0.859, 0.826, 0.812, 0.659, and 0.431. The position of the subject during measurement was found to affect staging, with upright examinations reflecting greater prolapse. Staging and substaging were reported to be highly reproducible (taub = 0.712 and 0.712, respectively). In 64% of subjects, the stages identified were identical, and in the remainder, they did not vary by more than one stage. All variation was increased in the upright position.12 The standardization studies were done in the English language, and the standardization document was formally adopted by the International Continence Society in October 1995.
The Pelvic Organ Prolapse Questionnaire Descriptive System
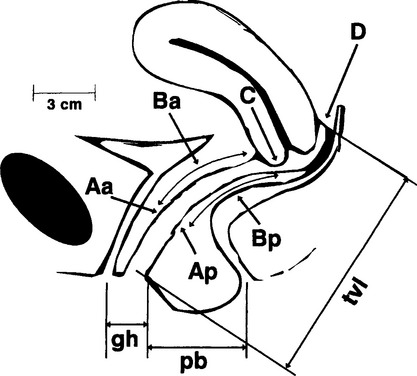
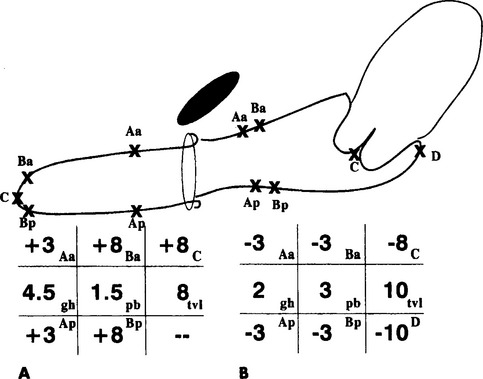
The POP-Q descriptive system allows the clinician to quantify precisely a woman’s pelvic support without assigning a severity value; to make accurate, site-specific observations of the stability or progression of prolapse over time; and to accurately describe outcome of surgical repair. The system uses six reference points (Fig. 30-1) and a 3 × 3 grid (Fig. 30-2) for recording a quantitative description of pelvic organ support.
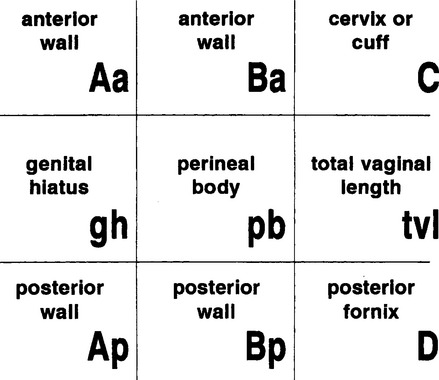
Figure 30-2 Three-by-three grid for recording a quantitative description of pelvic organ support.
(From Bump RC, Mattiasson A, Bo K, et al: The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10-17, 1996.)
Two points on the superior vagina represent the most proximal locations of the lower reproductive tract in a normal position. Point C represents the most distal or dependent edge of the cervix or the leading edge of the vaginal wall cuff (i.e., hysterectomy scar) after total hysterectomy. Point D represents the location of the posterior fornix or pouch of Douglas in a woman who still has a cervix and the level of uterosacral ligament attachment to the proximal posterior cervix. It is helpful in differentiating suspensory failure of the uterosacral–cardinal ligament complex from cervical elongation (symmetric or eccentric), in which the location of point C is significantly more positive than the location of point D. Point D is omitted in the absence of the cervix.