Fig. 13.1
Port placement for a total proctocolectomy with IPAA
Some flexibility in port placement is also important. In obese patients, the umbilicus may be significantly more caudal relative to abdominal/pelvic structures, necessitating a more cephalad point of entry into the abdomen.
Ordering the Elements of the Procedure
A laparoscopic proctocolectomy is essentially comprised of multiple smaller operations: (1) right colon mobilization, (2) hepatic flexure mobilization, (3) left colon mobilization, (4) splenic flexure mobilization, (5) rectal mobilization, (6) division of the anorectum, (7) transection of colon mesentery, (8) ileoanal pouch formation/anastomosis, and (9) ileostomy formation. There are many “correct” ways to order the elements of a laparoscopic proctocolectomy, several impractical ways (difficult to transect the rectum before mobilizing it!), and a few inadvisable ways.
We recommend against transecting the left colon/sigmoid mesentery before mobilizing the rectum, as these attachments provide important caudal retraction when the patient is in Trendelenburg position. It also is important to make a strategic decision to divide transverse colon mesentery intra- vs. extracorporeally. If a vertical incision is planned, then this can facilitate an extracorporeal transection of the transverse colon mesentery, as well as pouch formation. Also, it is our preference not to divide major vascular pedicles early in the procedure, as this avoids an ischemic portion of colon remaining within the abdomen for extended periods of time. Hence we utilize a lateral-to-medial approach to mobilization of the intra-abdominal colon, which preserves the vascular pedicles. In general, however, the various elements of the case can be ordered according to surgeon preference.
Right Colon Mobilization
For this maneuver, the OR table is placed in steep Trendelenburg, with the right side elevated. The small bowel is swept out of the pelvis and to the left using atraumatic techniques. The omentum is swept into the left upper quadrant. Commencing at the right pelvic brim, the peritoneal reflection bridging between the terminal ileum/cecum and the retroperitoneum is scored with the cautery scissors (Figs. 13.2 and 13.3). In patients with normal BMI, the ureter can often be visualized through the peritoneum, whereas in heavier patients this is more readily seen after opening the retroperitoneal plane. This dissection along the white line of Toldt continues superiorly and medially, taking care to remain in the correct plane anterior to Gerota’s fascia (Videos 13.1 and 13.2). Throughout the dissection, care is taken to identify and protect the right ureter, inferior vena cava, and the duodenum. Some visual cues are useful here: (1) if the iliopsoas muscle is visualized, this implies that the dissection is too posterior, (2) the contour of the kidney should be seen posterior (not medial) to dissection, and (3) the peritoneum of the right colon mesentery should not be breached—if the dissection is occurring through fatty tissue, this should prompt a reevaluation. Occasionally, due to scarring from inflammatory disease processes or prior surgery, this plane can be difficult to elucidate. In these cases, the right colon can be mobilized in a counterclockwise direction, starting at the level of the hepatic flexure and proceeding proximally. This portion of the dissection can be considered completed when inferior and anterior surfaces of the duodenum are exposed. The peritoneum around the base of the terminal ileal mesentery is fully dissected to the level of the duodenum to facilitate subsequent “reach” of the pouch, when a pouch-anal anastomosis is intended.
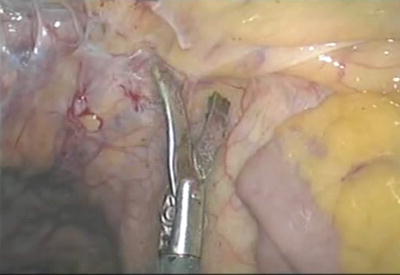
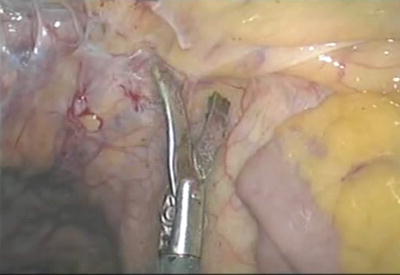
Fig. 13.2
Mobilization of the terminal ileum. Courtesy of Conor Delaney, MD, with permission
Fig. 13.3
Lateral-to-medial mobilization of the right colon
Hepatic Flexure Mobilization
For this maneuver, the OR table is placed in steep reverse Trendelenburg, with the right side elevated. The operating surgeon, standing on the patient’s left, can use the supraumbilical trocar to place caudal retraction on the hepatic flexure. With this retraction, the hepatocolic attachments between the superior margin of the colon and the inferior aspect of the liver are placed under tension and can be divided and swept off the underlying retroperitoneum. From the left abdominal trocar, an energy delivery device can be used to divide these tissues. Dissection continues posteriorly, inferiorly, and medially to expose the anterior surface of the duodenum and the interface between the duodenum and pancreas. This dissection should readily merge with the mobilization, which has already been performed of the right colon. As dissection moves medially (clockwise), the lesser sac is entered.
Left Colon Mobilization
The mobilization of the left colon typically starts at the level of rectosigmoid. This area is a well-defined starting point for both more proximal and more distal dissection. The patient is placed in Trendelenburg position, with the left side elevated. The sigmoid colon is grasped and retracted medially using the right-sided trocar, and the lateral peritoneal attachments are taken sharply using the suprapubic trocar (Fig. 13.4). Gentle sweeping of the peritoneal reflection laterally with judicious cautery will reveal the underlying ureter and iliac vessels underneath the peritoneal covering (Video 13.3). The white line of Toldt “stays with the patient,” i.e., the plane of dissection is immediately medial to the white line, and this is the most reproducible method of finding the ureter. This dissection proceeds distally to the pelvic brim and proximally to the splenic flexure (Video 13.4).


Fig. 13.4
Lateral-to-medial mobilization of the left colon
Splenic Flexure Mobilization
Splenic flexure mobilization is a critical and frequently challenging technical element of a proctocolectomy. The mobilization can be challenging, primarily due to issues regarding exposure and the risk of injuring the splenic capsule, vessels within the splenocolic ligament, or the colon mesentery. The flexure can be approached in one of two directions—clockwise or counterclockwise—usually both directions need to be undertaken in order to perform a complete mobilization.
The counterclockwise dissection is a natural continuation of the sigmoid and left colon mobilization (Video 13.5). For this portion of the maneuver, the operating surgeon can work either from the patient’s right side or between the patient’s legs. The OR table should be in steep reverse Trendelenburg position and tilted slightly to the right. Adequate tension must be maintained medially as the splenic flexure is approached, in order to avoid wandering into or behind the kidney. As the apex of the flexure is mobilized, the underlying pancreas should be identified in order to prevent injury. The splenocolic ligament and other attachments between the transverse colon mesentery and the retroperitoneum are best divided using an energy delivery device.
The clockwise dissection begins in the area of the mid- to distal transverse colon (Video 13.6). A decision needs to be made whether or not to remove the greater omentum with the specimen or preserve it. If the intent is to leave the omentum, then the lesser sac can be entered by dissecting the omentum from the anterior surface of the transverse colon and reflecting it into the upper abdomen. The left and inferior trocars can be used to retract the omentum cephalad and the colon caudal. Using the right trocar, an energy delivery device can be used to open the lesser sac, moving distally. Alternatively, the omentum can be removed en bloc with the transverse colon. In these cases, the greater omentum is incised just caudal to the gastroepiploic vessels, superior to approximately the midpoint of the transverse colon, and the lesser sac is entered. The colon and omentum are retracted caudally, and the lesser sac is opened by dividing the gastrocolic and splenocolic attachments, moving toward the spleen. Finally, the retroperitoneal attachments need to be divided to ensure complete mobilization of the splenic flexure. This is facilitated by caudal retraction on the colon, keeping the tension on the adhesions and dividing from the apex (Video 13.7).
Splenic flexure mobilization can be made difficult by previous surgery, body habitus, or anatomical variations. In these situations, the placement of an additional trocar in the right upper quadrant may be of use, especially during the clockwise dissection. A grasper placed through this trocar can facilitate with anterior/cephalad retraction and exposure of the lesser sac.
Rectal Mobilization
Mobilization of the rectum begins with the caudal continuation of the sigmoid/left colon dissection. The OR table is placed in Trendelenburg position, with the left side elevated. Using the right trocar as a grasper, the rectosigmoid junction is retracted medially (Video 13.8). A dissecting instrument is placed through the suprapubic trocar, and this is used to incise the reflection between the mesorectum and the pelvic sidewall. Notably, this maneuver can be accomplished with the operating surgeon on either the patient’s right or left side. While it may seem initially awkward, it is our preference to perform this maneuver with the operating surgeon standing on the patient’s left, using an instrument placed through the left trocar as a retractor.
During the course of this dissection, great care needs to be taken to identify the appropriate plane that separates the mesorectum from retroperitoneum. The left ureter and superior hypogastric nerve should be clearly identified. Proceeding distally, the peritoneum between the mesorectum and the lateral pelvis should be incised. Careful inspection of the left side of the rectum should demonstrate “white tissue” (pelvic sidewall tissues) laterally and “yellow tissue” (mesorectum) medially. The line between these two types of tissues marks the appropriate point of entry into the presacral plane.
This left-sided dissection then continues as far as possible prior to moving to the right side. The right-sided dissection uses similar landmarks to divide the pelvic peritoneum, separating the mesorectum from the pelvic sidewall. Once again, care needs to be taken to identify the superior hypogastric nerve and ureter, although the right ureter is usually not endangered during this portion of the operation. Moving medially and distally, the plane of dissection joins with the dissection already performed on the left side. With the rectum elevated anteriorly, the dissection continues distally as far as possible, occasionally necessitating further attention to lateral attachments (Video 13.9).
With the posterior and lateral attachments of the rectum mobilized, attention can be turned to the anterior plane. In a male, this begins with incising the peritoneal reflection and dissection to expose the seminal vesicles and subsequently the prostate. In the course of exposing this anterior plane, the suprapubic instrument is the most useful in attaining effective cephalad retraction. Importantly, the patient should be in steep Trendelenburg positioning to maximize the use of gravity as a “second assistant.” There is significant confusion regarding the anatomy of Denonvilliers fascia in this area, and the importance of removing it during the course of a proctectomy. In the absence of an anterior rectal cancer in this location, there is no need to fashion a plane of dissection that denudes the prostate or seminal vesicles (see Fig. 10.8).
In females, the peritoneal reflection is significantly deeper within the pelvis (Fig. 13.5). The uterus is frequently a significant barrier to visualizing the anterior reflection. If this is the case, then the uterus can be retracted anteriorly with either a transvaginal uterine retractor or a transabdominal suture. In order to suture the uterus out of the field of dissection, a straight needle is passed through the abdominal wall inferior to the suprapubic port, through the fundus of the uterus, then exited through the abdominal wall and tied.