(1)
Al Agouza, Cairo, PO, Egypt
9.1 Anatomical and Embryological Background (Fig. 9.1)
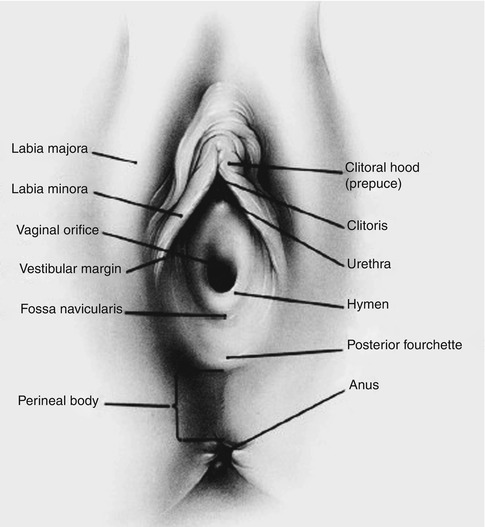
Fig. 9.1
Anatomy of the labia
In girls, the unfused parts of the labioscrotal (genital) swellings give rise to the labia majora; the folds fuse anteriorly to form the mons pubis and anterior labial commissure and posteriorly the posterior labial commissure. The urethral folds fuse posteriorly to form the frenulum of the labia minora. The unfused urethral (urogenital) folds give rise to the labia minora. The unfused genital swellings enable the urogenital sinus to open into the anterior (urethral) part of the vagina and the vaginal vestibule. The genital tubercle becomes the clitoris and is recognizable by the 14th week [1].
Labia Majora
The labia majora are prominent cutaneous folds located between the mons pubis and the perineum mainly consisting of adipose tissue, hair follicles, and sebaceous glands. They unite anteriorly to form the anterior commissure of the labia majora and posteriorly fuse with the surrounding tissues to form the posterior commissure. The outer surfaces of the lips of the labia majora are covered with pigmented skin containing many glands. The insides of the labia are smooth, pink, and hairless. The labia majora resemble the anterior abdominal wall in structure. Camper’s fascia with predominance of fat is superficially located, and the thicker Colles fascia forms the deeper layer and corresponds to the Scarpa’s fascia in the abdominal wall. The Colles fascia is inferiorly attached to the ischiopubic rami, posteriorly to the urogenital diaphragm, but lacks anterior attachment. This prevents spread of hematomas and infections to the thigh, but spread can occur to the anterior abdominal wall. The round ligament of the uterus and the obliterated processus vaginalis terminate in the labia majora. Both labia function as fat pads and specifically function as protection from trauma and the labia minora close together, protecting their inner mucous membrane and closing off the vaginal entrance.
Labia Minora
Alternatively termed nymphae or labium minus pudendi, they are two longitudinal, cutaneous folds that typically vary in size. They are situated internally between the labia majora on each side immediately adjacent to the vestibule, devoid of fat, and rich in sebaceous glands. There is a core of connective tissue and vascular erectile tissue with sensory nerve endings to which they are loosely attached. Each labium minus splits anteriorly around the clitoris, uniting with the labium minus from the contralateral side to form the prepuce or the preputium clitoridis over and frenulum under the clitoris, which overhangs the glans clitoris, in a subset of girls; the posterior ends of the labia minora may be joined across the midline by a fold of skin, named the frenulum labiorum pudendi (i.e., fourchette or posterior commissure of the labia minora). The labia minora are often asymmetrical.
Intense estrogen receptor staining is seen in the epidermis and dermis of the labia minora, but it was only detected in a restricted area closer to the clitoris. There were also basal and suprabasal receptors in the epidermal cell membrane restricted to superficial sections of the labia minora; estrogens may modulate the behavior of epidermal keratinocytes, especially in the genital skin [2].
9.2 Labial Hypertrophy
Definition
Hypertrophy of the labia minora is defined as a protuberant labial tissue that extends beyond the labia majora. Labial hypertrophy may simply be a normal variant; additionally, asymmetry of the female genitalia is a natural occurrence, thus making a clear distinction between normal and abnormal anatomy challenging.
Etiology
Labial hypertrophy is most commonly congenital in origin, but acquired causes must be considered, such as exogenous androgenic hormones in infancy, sensitivity to topical estrogen, dermatitis secondary to urinary incontinence, vulvar lymphedema (i.e., infection by Filaria sanguinis hominis, which invades lymph channels, especially in tropical countries). Transient hypertrophy of the labia minora is not rare in neonates and premature girls due to transient hyperestrogenemia (Fig. 9.2).


Fig. 9.2
Transient temporary labial hypertrophy in neonate
Also both labia majora and minora hypertrophy is common with cases of adrenogenital hyperplasia (Fig. 9.3).


Fig. 9.3
Marked labial hypertrophy in a case of adrenogenital hyperplasia
Rarely, hypertrophy of one or both labia majora may cause unilateral or bilateral prominence of the labial structure. Herniation of an ovary into the labium should be easily ruled out by physical examination. Vascular or lymphatic malformations must be ruled out in bilateral lesions, but many unilateral cases are idiopathic. Resection of the hypertrophic tissue may be indicated when the lesion appears to be idiopathic (Fig. 9.4).


Fig. 9.4
Prominent idiopathic left labium majus hypertrophy
Clinical
Felicio [3] has proposed a classification system for hypertrophy of the labia minora based on length: labia less than 2 cm (type I), 2–4 cm (type II), 4–6 cm (type III), and more than 6 cm (type IV). Some physicians believe that 5 cm is the upper limit of normal labial size.
Labial hypertrophy may lead to chronic local irritation, problems with personal hygiene after bowel movements, and discomfort during walking, cycling, or sitting. Karyotyping and hormonal studies should be performed, and in a case of normal laboratory results in an XX neonate, follow-up should be performed because some of these changes in the female genitalia are transient and benign.
Management
Surgical correction may be offered in cases of aesthetic concern, physical discomfort, or dyspareunia, and usually reduction labioplasty procedures are not indicated in the pediatric age group, but some authors indicated such surgery in adolescence, when different techniques could be applied, but the main goals which should be fulfilled are (1) reduction of the hypertrophic labia minora, (2) maintenance of neurovascular supply, (3) preservation of introitus, (4) optimal color/texture match of labial edge, and (5) minimal invasiveness [4].
9.3 Labial Hypoplasia
For unclear reasons, one or both labia may not develop normally; this may be evident in childhood or may only be evident through development in puberty as one side develops normally and the other side is noted to be smaller or absent. Absence of labia or hypoplastic labia has been reported in cases of adrenogenital hyperplasia, and it is also reported in popliteal pterygium syndrome, also the labia may be short with hypoplastic or absent at its posterior part, covering only the anterior two-thirds of the introitus, and doesn’t lit posteriorly to form the posterior commissure and forming only short arced folds on both sides (Fig. 9.5).


Fig. 9.5
Deficient posterior part of the labia minora
9.4 Labial Fusion
Nomenclature
Labial agglutination, vulvar fusion, and synechia of the vulva
Definition
Labial fusion refers to partial or complete adherence of the labia minora; rarely, the labial fusion is so nearly complete as to make the girl having no vaginal orifice or misdiagnosed as a case of intersex; also it may cause urinary outflow obstruction with resultant bladder distention or even hydronephrosis.
Incidence
Acquired labial fusion is most commonly noted between 3 months and 4 years of age and has a peak incidence of 3.3 % between 13 months and 23 months of age; true congenital fusion is rarely seen as an isolated anomaly, but extensive labial agglutination sufficient to obscure the hymen was noted in 5 % of cases of partial agglutination [5] (Figs. 9.6 and 9.7).



Fig. 9.6
Acquired labial adhesion

Fig. 9.7
An evident vulvovaginitis seen proximal to the separated labia
Etiology
Labial fusion is considered as an acquired condition secondary to hypoestrogenism and vulvovaginitis, and in countries where female genital mutilation is practiced (female circumcision), a dense fibrous adhesion after this procedure in some cases may lead to an acquired form of labial fusion [6] (Figs. 9.8 and 9.9).
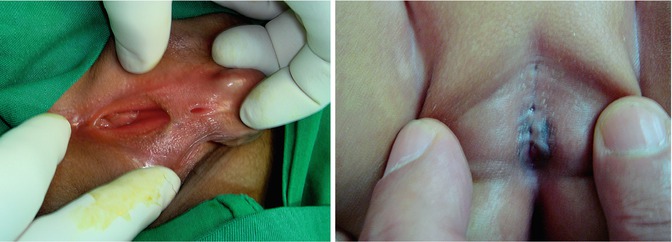
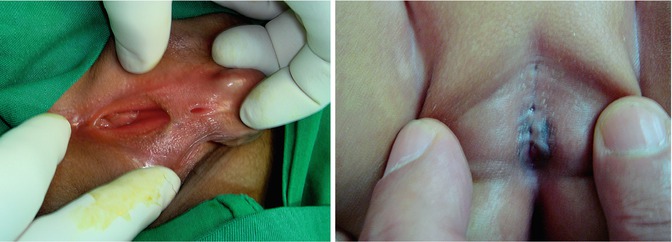
Figs. 9.8 and 9.9
Cicatricial labial fusion after female circumcision
Congenital fusion of the labia is typically associated with virilization from congenital adrenal hyperplasia; however, cases of familial labial fusions not associated with adrenal hyperplasia have been reported. The true labial fusion as a defect in the early development of the middle parts (usually not fused) of the urogenital folds is much less frequent than a posterior fusion due to inflammatory-type reactions, and it is attributed to early intrauterine exposure to androgen, and in cases of adrenogenital hyperplasia, some cases of imperforate anus may be associated with a true labial fusion (Fig. 9.10).


Fig. 9.10
A case of congenital labial fusion with imperforate anus
Powell et al. defined four distinct types of urogenital sinus anomalies based on vaginal location, and type I is presented as a labial fusion [7].
Clinical
Many cases of labial adhesions, if noticed by a concerned mother or inexpert general practitioner, may be misdiagnosed as a case of hermaphrodite, and a lot of worries and extensive investigations done to assign the exact nature of baby sex. Usually, the adhesions are asymptomatic, but the urine trapped in these labial folds may act as a source of urinary tract infection, post-micturition dribbling, or even urinary incontinence. Severe vulvovaginitis may superpose labial adhesions and offensive discharge may be evident.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








