(1)
Al Agouza, Cairo, PO, Egypt
10.1 Embryological Background
Nomenclature
The hymen is named after the God of marriage “Hymenaios” in classical Greek mythology. The word “hymen” is usually synonymous with virgin membrane.
The human female is the only primate member to possess a hymen. However, Balke et al. reported the presence of membranous constriction (hymen) with an orifice, less than 2 cm in diameter in nulliparous elephants, that is not broken by mating but only during birth [1].
Embryological development of vagina results from lower portion paramesonephric ducts fusion and regression forming the uterovaginal primordium (gives rise to the uterus and superior part of vagina). Contact of the uterovaginal primordium with the urogenital sinus induces formation of paired outgrowths named sinovaginal bulbs. The sinovaginal bulbs fuse to form the vaginal plate. The cells of the fused bulbs undergo apoptosis to form the lumen of the vagina (Fig. 10.1).
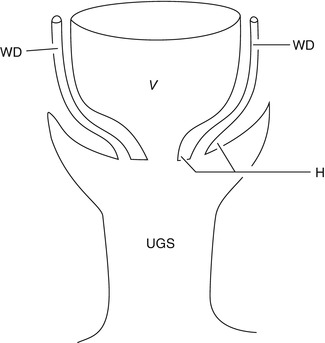
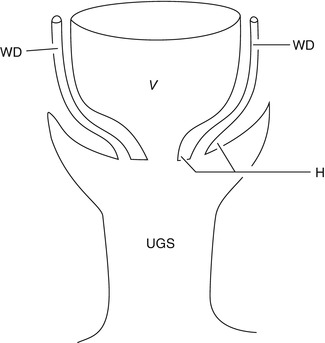
Fig. 10.1
Embryological development of the vagina at 8 weeks, showing Wolffian ducts issuing between layers of hymen into the urogenital sinus. V vagina, WD Wolffian duct, UGS urogenital sinus, H hymen [2]
The hymen demarcated the junction between the Müllerian and urogenital structures. It is derived from the epithelium of the urogenital sinus, and during the fetal stage, it represents the distal part of vagina. By the fifth month of gestation, the canalization of the vagina is complete. Histologically, the hymen is composed mainly of elastic and collagenous connective tissue, covered by stratified, squamous epithelium, and the caudal layer belongs to the urogenital sinus, but the cranial layer is derived from the Müllerian duct. The epithelium is thicker at the attached edge. Nerve fibers are scarce, at the free margin of the hymen. No nerve cells and fibers are present at the free edge of the hymen. There is no trace of glandular or muscle element. The hymen is relatively an avascular membrane so it is unlikely to bleed significantly even if it is torn.
The normal hymen is described as fairly thin, elastic, and translucent. Until late fetal life, the lumen of the vagina is separated from the cavity of the urogenital sinus by a membrane, the hymen, but the configuration of hymen differs dramatically from one female to another one. At birth, it is commonly annular in shape, while the crescentic configuration is most prevalent in children over the age of 3 years. Furthermore, the redundancy of the hymen decreased in 75 % of girls. In the newborn, the hymen is vascular and its epithelium is thick. In the prepubertal female, the lack of estrogen renders the hymenal tissue thin and friable.
Function of the hymen: The hymen has no known biologic function, but it may have a role in the protection of the vaginal mucosa from contamination by fecal and other materials, at the early stage of life.
Misdevelopment can result in any of the following three congenital anomalies:
Imperforate hymen (failure of epithelial degeneration)
Low, mid, or high transverse septum of the vagina (incomplete unit)
Atresia of the vagina resulting in persistence of a portion of solid cell cord.
Recently, interest has focused on expression and function of the mammalian HOXA genes as a possible etiology of many genitourinary developmental abnormalities including the female genital system [3].
10.2 Variation in Hymenal Development
Regular development of ringlike hymenal structure provides normal vaginal outflow. Until late fetal life, the lumen of the vagina is separated from the urogenital sinus by invagination of the posterior wall forming a hymenal membrane. The hymen usually ruptures during the perinatal period and remains as a thin fold of mucous membrane circumferentially at the entrance of the vagina [4].
A smooth hymen with a central orifice was observed in 53.5 % of the female neonates, a folded hymen with a central orifice in 27.3 %, a folded hymen with eccentric orifice in 4.5 %, an anterior opening of the hymen in 10.8 %, a posterior opening in 0.6 %, a hymenal band in 3 %, and an almost imperforate hymen in 0.3 % of the newborns. The presence of an anterior opening, posterior opening, hymenal band, or almost imperforate hymen may interfere with free vaginal discharge. A ruffled, irregular hymen and a hymenal band require a careful investigation for other genital malformations [5].
Variants in hymenal configuration are often seen, varying from hymen semilunaris, anularis, cribriformis, septus, fimbriatus, and navicularis. Estrogen withdrawal at an older age may convert some of the annular types into this crescentic-shaped configuration.
In spite of the recommendations for early inspection of the external genitalia in newborns, variations in hymenal anatomy can escape diagnosis until the time of menarche. There is a spectrum of variations in hymenal configuration, like different types of fenestration, septa, etc., with more or less clinical significances. According to the age of the examined girl, the hymen may be fimbriated, which is the most common type (46 %) in infants aged 12 months or younger, and crescentic, the most common (51 %) in girls older than 24 months. No significant difference was noted in hymen configuration by race. Hymenal bumps (mounds) were observed in 7 % and hymenal tags in 3 % [6] (Fig. 10.2).
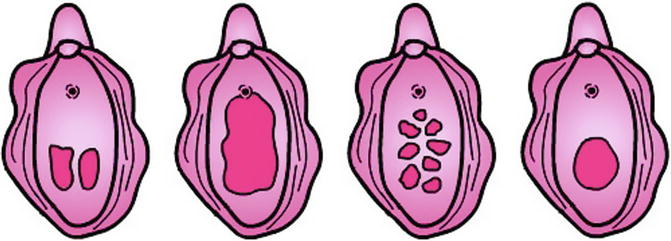
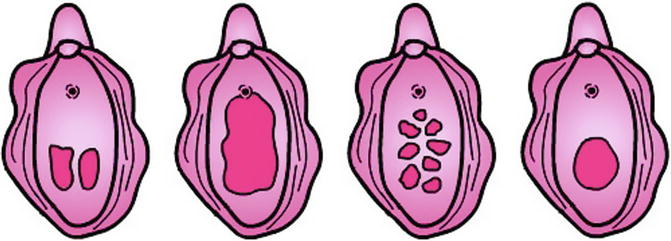
Fig. 10.2
Normal variations in hymenal configuration
10.3 Imperforate Hymen (IH)
Hydrocolpos
Hematocolpos
Hydrometrocolpos
Pyocolpos
Nomenclature
Hymen imperforatus or atresia hymenalis
Definition
IH is an external congenital genital anomaly when the nonperforated membrane of the hymenal tissue covers the entrance into the vagina; the membrane is composed of vaginal epithelium and epithelium of the urogenital sinus interposed by mesoderm. Imperforation of hymenal tissue may also be present in variations as microperforate, septate, stenotic, or cribriform hymen (Fig. 10.3).
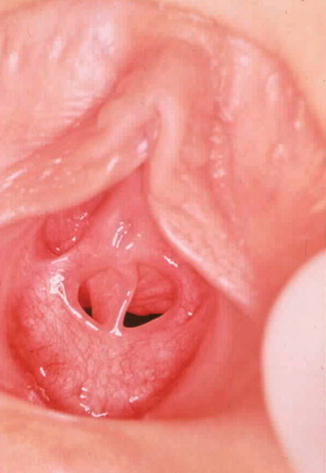
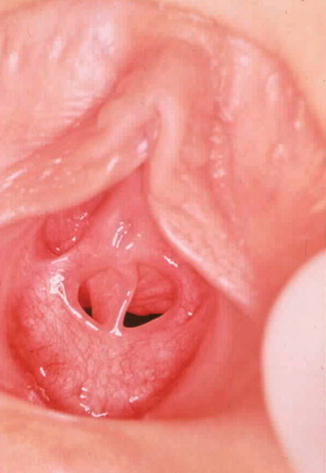
Fig. 10.3
Septated hymen in a newborn
The hymen consists of a membrane separating the evaginated caudal end of the fused paramesonephric ducts from the repaginated urogenital sinus. A highly placed transversal septum is often found, and it is important to distinguish imperforate hymen from other anomalies.
Historical Background
Hydrocolpos secondary to imperforate hymen was first recognized as early as 1856 by Godefroy [7]. A detailed description of the disorder was reported by Mahoney and Chamberlain in 1940, but almost 350 years has passed since Pare first described hematocolpos as a complication of imperforate hymen [8]. The first detailed report on neonatal hydrometrocolpos was that of Mahoney and Chamberlain in 1940 [9].
Incidence
Imperforate hymen is relatively rare and the reported incidence ranges from 0.014 % to 0.1 %, but a higher incidence of 3.8 % had been reported [10].
Etiology
The hymen may persist if the centrally placed epithelial cells do not degenerate and produce the expected lumen. An imperforate hymen is usually the result of the urogenital sinus not canalizing. In pathological conditions, it becomes thickened, fibrotic, and nonelastic. The maternal hormones affect the reproductive tract of the female infant both in utero and during the early neonatal period, increasing the secretions of the uterine and cervical glands. The possible explanation of IH is that the target tissue may be more sensitive to or exposed to higher levels of maternal estrogen. By the age of 1 month, vaginal secretion becomes poor and alkaline, the epithelium is thin, the individual cells small and devoid of glycogen, and the basal layer comparatively inactive; if maternal estrogenic stimulation and vaginal obstruction coexist, hydrometrocolpos will develop [11].
Families with more than one individual affected by imperforate hymen have been described, but no common mode of inheritance has been identified. It is not known whether it is an autosomal or an X-linked transmission, but an autosomal recessive mode of transmission was suggested; also some rare syndromes have been described which are characterized by imperforate hymen. Ulnar–mammary syndrome is associated with upper limb structures, apocrine/mammary hypoplasias, dental abnormalities, and genital anomalies including imperforate hymen [12].
In 1964, McKusick and coworkers reported two related Amish sibships with four girls suffering from hydrometrocolpos, suggesting that at least one form of hydrometrocolpos is inherited as an autosomal recessive disorder. Later, it was realized that hydrometrocolpos, polydactyly, and congenital heart disease belong to the same genetic entity [13].
It is difficult to dispute the theory claiming an acquired etiology of few cases of IH after repeated infection in the neonatal period or trauma from sexual abuse later at childhood with subsequent cicatrization and occlusion of the hymenal apparatus [14].
Associated Anomalies
Only a few associated anomalies with imperforate hymen have been reported, such as polydactyly, bifid clitoris, duplication of the ureter, ectopic ureter, hypoplastic kidney, multicystic dysplastic kidney, urethral membrane, imperforate anus, and low anorectal anomaly. However, imperforate hymen with its sequels has been reported in 50 % of cases of cloacal anomalies in female.
10.3.1 Microperforate Hymen
A microperforate hymen is essentially an imperforate hymen with a very small hole within it. The hole may be large enough for mucus and/or blood to come through the hymenal opening, but the child at menarche instead of having a regular menstrual period lasting 4–7 days may have a period which lasts longer. This is due to the fact that the blood cannot come out at a normal rate. A microperforate hymen may resolve spontaneously and the opening may get larger as a child becomes older. A surgical approach can be undertaken to resect the excess hymenal tissue.
10.3.2 Hydrocolpos
The newborn may present with a whitish bulging mass filling the introitus (hydrocolpos or mucocolpos). If hydrocolpos is small or not detected at birth, secretions resorb up to the end of the first months of life, and the condition may be undetected until puberty when it will be presented as a hematocolpos; also if there is a low level of maternal hormones, there is no extra genital secretion and the obstruction will usually remain unnoticed until puberty, where hematocolpos occurs after menarche. The presence of an interoital bulge differentiates hydrocolpos due to imperforate hymen from hydrocolpos due to vaginal atresia and vaginal septum (Fig. 10.4).


Fig. 10.4
Hymenal bulge due to IH and hydrocolpos
Occasionally, the presence of mucocolpos and abdominal mass with urinary retention has been described in infancy and childhood, and usually the vaginal and uterine contents will not have an access to the peritoneal cavity through the ostium of the fallopian tube, but few cases of ruptured tube and peritonitis had been recorded [15].
The retained fluid in hydrometrocolpos consists of vaginal and uterine secretions and may be acidic and serous or mucoid, containing large numbers of desquamated epithelial cells, leukocytes, and erythrocytes. In hydrocolpos the vagina is usually distended with clear fluid but the uterus is displaced upward, but why the uterus is not always dilated is not known.
10.3.3 Pyocolpos
Rarely the vaginal content may be infected and the neonate may present with a distended vagina and uterus with pure pus, especially if a fistula with the urogenital sinus is present, so attention should be paid to diagnose the possibility of coexistence of such fistula by cystourethrography after surgery. Pyocolpos may result in life-threatening sepsis, and it is essential to diagnose and treat it early; aspiration of the pus and its culture and detection of the most sensitive antibiotic are essential before hymenal incision (Fig. 10.5).










