Chapter 28 ERCP in Pregnancy
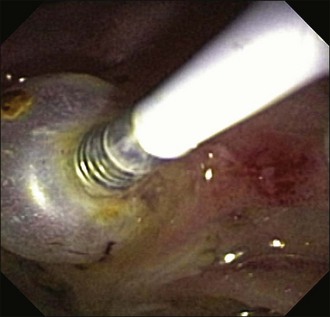
Physiologic alterations during pregnancy, such as weight gain and hormonal changes, increase the risk of cholelithiasis. Elevated estrogen levels are believed to increase bile lithogenicity, while a rise in progesterone causes smooth muscle relaxation and bile stasis, thereby promoting gallstone formation.1,2 The incidence of gallstones in the general population is approximately 10%, with gallstones and biliary sludge reported in up to 12% and 30% of pregnant patients, respectively.3,4 Choledocholithiasis during pregnancy is much less frequent and has been reported to occur in 1 in 1200 deliveries.5 Common bile duct (CBD) stones (Fig. 28.1) may lead to adverse events such as pancreatitis and cholangitis and generally require prompt therapeutic intervention.
Older literature suggests that open cholecystectomy with CBD exploration during pregnancy poses significant risks to the fetus.6 Although newer reports suggest laparoscopic cholecystectomy is safer, the presence of choledocholithiasis still necessitates CBD exploration.7 Although endoscopic retrograde cholangiopancreatography (ERCP) during pregnancy has become increasingly used in recent years, it was not always accepted as an appropriate therapeutic modality. Concerns about potential teratogenic effects of fluoroscopy and adverse events such as pancreatitis that could potentially harm both the mother and the fetus were raised. It was not until 1990 that Baillie and colleagues at Duke University Medical Center reported the first experience of ERCP during pregnancy. Five pregnant women underwent ERCP with sphincterotomy without any adverse events to the mother or fetus.8 Since that time over 300 cases of ERCP during pregnancy have been reported.9 It is now considered a safe and effective treatment for pregnant women when performed for appropriate indications with the support of a multidisciplinary team.
Indication
It is essential to have a sound indication before performing ERCP on a pregnant woman. ERCP in pregnancy is most commonly performed for management of choledocholithiasis. Strong suspicion for the presence of a CBD stone is necessary before considering ERCP. There is no place for diagnostic ERCP, given advances in diagnostic imaging. ERCP has also been performed during pregnancy for cholangitis (Fig. 28.2), biliary pancreatitis, and bile duct injury.10,11 There have been a few reports of performing ERCP in pregnant patients for management of choledochal cysts, parasitic infestation of the biliary tree, and pancreatic adenocarcinoma.12–14 Unusual situations such as these warrant careful evaluation on a case-by-case basis with a thorough assessment of the risks and benefits before pursuing ERCP. Serious obstetric adverse events, such as placental abruption, eclampsia, rupture of membranes, or imminent delivery, are contraindications to endoscopy. Rapid pregnancy testing prior to endoscopy is now commonplace and should be considered the standard of care prior to ERCP in women of childbearing age. Box 28.1 lists the indications for ERCP in pregnancy.
Alternative Diagnostic Imaging Modalities
Transabdominal ultrasonagraphy is commonly used because of its safety profile and low cost. It is a sensitive method of detecting gallstones but has a low sensitivity for detecting CBD stones.15 It should still be used as an initial test, as a dilated CBD in the right clinical setting is often sufficient evidence to pursue ERCP. It is important to keep in mind that the symptoms of biliary disease (i.e., nausea, vomiting, abdominal pain) can often be encountered as a part of normal pregnancy, potentially obscuring the clinical picture.
Computed tomography (CT) scan is not recommended in the pregnant patient due to radiation exposure and poor sensitivity for choledocholithiasis.16 Magnetic resonance cholangiopancreatography (MRCP) is an excellent imaging tool for detection of CBD stones with a reported sensitivity of 92%.17 There are no known deleterious effects of magnetic fields on the fetus. Magnetic resonance imaging (MRI) is indicated in pregnancy in a diagnostic-therapeutic urgency when the information needed cannot be obtained by other nonionizing imaging.18 It should be kept in mind that paramagnetic contrast agents (gadolinium) cross the placenta. Though there are no reports of harmful effects on the fetus, the molecule theoretically remains in the fetoplacental system and for this reason these agents are generally not recommended for use in the pregnant patient.19 Fortunately MRCP does not require paramagnetic contrast to image the biliary and pancreatic ductal systems, although imaging of other structures is limited without contrast. It should be noted that MRCP is less sensitive for detection of smaller stones (<6 mm).20
Endoscopic ultrasound (EUS) has emerged as a highly sensitive and specific test for choledocholithiasis (Fig 28.3) and can reduce the need for intervention in low or moderate probability cases.21,22 Only a few cases of EUS in pregnancy have been reported.9 The risk of a diagnostic EUS during pregnancy is believed to be minimal. It is reasonable to consider EUS immediately prior to ERCP in indeterminate cases of biliary obstruction if MRCP is not available or is contraindicated.
Timing
The optimal time to perform ERCP is during the second trimester, although it has been performed safely throughout gestation. ERCP during the first trimester should be avoided if possible due to fetal exposure to ionizing radiation during the period of organogenesis and the risk of spontaneous abortion. In the general population, 15% to 20% of clinical pregnancies end in spontaneous abortion, with most of these occurring during the first trimester.23 This may represent a confounding factor if miscarriage occurs after an ERCP performed in the first trimester. ERCP during the third trimester may be complicated by distortion of anatomy by the gravid uterus and risk of preterm labor. In the presence of an urgent indication, ERCP should be performed regardless of the stage of pregnancy.
Surgery for gallbladder disease during pregnancy is controversial. Some surgeons favor early surgical management while others prefer to wait until after delivery.7 If possible, surgery should be avoided in first trimester during the period of organogenesis. Laparoscopy in the third trimester may be problematic due to the enlarged uterus, which can obscure surgical anatomy and limit access to the gallbladder fossa. The second trimester and early third trimester provide the best window should surgery be necessary.24 Recent reports suggest that laparoscopic cholecystectomy can be performed safely throughout gestation.7
Radiation Exposure during ERCP
The risks of radiation to the fetus include abnormalities in growth and development, malformations, and increased risk of future cancer. Deterministic effects on growth and development have a threshold of approximately 100 milligray (mGy) and are at greatest risk of occurring between the second and fifteenth weeks of gestation.25 According to the American Congress of Obstetricians and Gynecologists, “exposure to less than 5 rad [50 mGy] has not been associated with an increase in fetal anomalies or pregnancy loss.”26 The risk of developing cancer from radiation, although small, is a stochastic effect and has no threshold level.25 (For gamma radiation: 100 rem = 100 rad = 1 gray = 1 sievert.)
Multiple studies have estimated radiation exposure levels to the fetus and have reported an average exposure between 10 and 310 mrad.27,28 The largest study by Kaheleh et al.29 examined radiation exposure in 15 pregnant women undergoing ERCP. Techniques were used to minimize fluoroscopy time and exposure levels were monitored by thermoluminescent dosimeters. The mean estimated fetal exposure level was 40 mrad (range of 1 to 180 mrad), which is well within the accepted teratogenic threshold. Samara et al.30 studied potential conceptus radiation doses using simulated mathematical models in 24 nonpregnant patients undergoing ERCP. These models took into account not only the effect of the primary radiation beam on the fetus, but also internal “scatter” radiation. The authors found that radiation exposure to the fetus may occasionally exceed 10 mGy. Though most pregnant patients are probably exposed to much lower levels, this finding underscores the importance of minimizing radiation exposure to pregnant women.
A variety of techniques can be used to reduce radiation exposure to pregnant patients (Box 28.2). Most importantly, fluoroscopy time should be minimized. Short “taps” of fluoroscopy can be used to confirm the position of the wire and catheter in the duct. A sphincterotome should be used for the procedure to avoid unnecessary catheter exchanges. “Hard copy” images should be avoided, as they expose the patient to higher levels of radiation. Instead, the “last-image-hold feature” should be used to review the study. Low-dose-rate pulsed fluoroscopy should be used with tight collimation in the area of interest to reduce the amount of scatter radiation. The x-ray tube should be kept as far from the patient as possible, while the image receptor should be kept as close as possible. Magnification can amplify radiation levels and its use should be avoided.31 Lead shielding can also be used to protect the fetus. It is important to place the lead apron beneath the patient, where the x-ray beam originates (Fig. 28.4). Lead shielding may reduce levels of primary radiation to the fetus but will not affect scatter radiation within the mother. Some have found the effect of lead shielding to be negligible.30 Nonetheless, it is still recommended as a simple method of decreasing radiation exposure without adding any risk. A dosimeter may be attached over the gravid abdomen to estimate levels of exposure to the fetus.29 Consultation with a radiation physicist may be helpful in planning ERCP in a pregnant patient. In recent years novel techniques have evolved for performing ERCP without fluoroscopy. This topic will be covered later in this chapter.
Box 28.2
Techniques to Reduce Radiation Exposure
 Use sphincterotome for cannulation to avoid catheter exchanges
Use sphincterotome for cannulation to avoid catheter exchanges
 Use short “taps” of fluoroscopy
Use short “taps” of fluoroscopy
 Use “last-image-hold” feature to review images
Use “last-image-hold” feature to review images
 Use low-dose-rate pulsed fluoroscopy
Use low-dose-rate pulsed fluoroscopy
 Collimate x-ray beam to smallest possible field
Collimate x-ray beam to smallest possible field
 Place patient far from radiation source and close to image receptor
Place patient far from radiation source and close to image receptor
 Consider use of choledochoscopy or EUS to confirm clearance of CBD
Consider use of choledochoscopy or EUS to confirm clearance of CBD
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree