Chapter 30 Echoendoscopic Ultrasound–Guided Biliary Drainage
1. To describe the equipment needed for such procedures
2. To describe the technique of biliary drainage under EUS guidance (Box 30.1)
3. To describe the place of these techniques relative to ERCP (Box 30.2)
Box 30.1
EUS Techniques for Biliary Drainage
 Transduodenal hepatic wire access for rendezvous procedure
Transduodenal hepatic wire access for rendezvous procedure
 C-SEMS through SEMS for hepaticogastrostomy
C-SEMS through SEMS for hepaticogastrostomy
 SEMS through distal biliary stricture via transhepatic approach
SEMS through distal biliary stricture via transhepatic approach
Box 30.2
Indications for EUS Access into the Biliary Tree
Equipment
Interventional Echoendoscopes
Around 1990 the Pentax Corporation developed an electronic, convex curved, linear array echoendoscope (FG 32UA) with an imaging plane in the long axis of the device that overlaps the instrumentation plane. This echoendoscope, equipped with a 2.0-mm working channel, enabled fine-needle biopsy under EUS guidance. However, the relatively small working channel of the FG 32UA was a drawback for pseudocyst drainage since it necessitated the exchange of the echoendoscope for a therapeutic duodenoscope to insert either a stent or a nasocystic drain. To enable stent placement using an echoendoscope, the EUS interventional echoendoscopes (FG 38X, EG 38UT, and EG 3870UTK) were developed by Pentax-Hitachi. The FG 38X has a working channel of 3.2 mm, which allows the insertion of an 8.5 Fr stent or nasocystic drain, and the EG 38UT and EG 3870UTK have larger working channels of 3.8 mm with an elevator allowing the placement of a 10 Fr stent.1,2
Needles and Accessories for Drainage
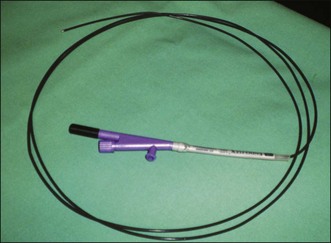
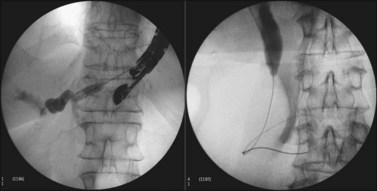
Some authors have used needle-knife catheters but the needle can be difficult to visualize endosonographically. The Zimmon needle knife (Cook Endoscopy, Winston-Salem, N.C.) has a large-gauge needle that is easier to visualize. Diathermy is usually required to penetrate a cyst, particularly when performed transgastrically (Fig. 30.1).3