Pieter Evenepoel, Dirk R. Kuypers
Dermatologic Manifestations of Chronic Kidney Disease
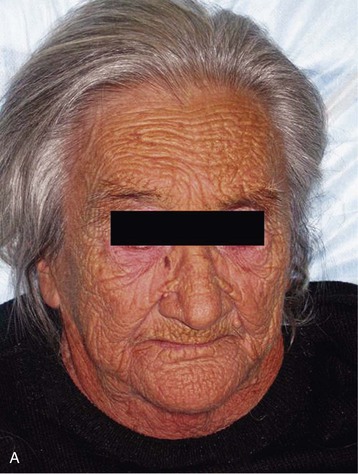
Cutaneous disorders are common in patients with end-stage renal disease (ESRD), with the most prevalent disorder being hyperpigmentation. Many of these cutaneous disorders are caused by the underlying renal disease, whereas others relate to the severity and duration of uremia.
Skin lesions associated with cutaneous aging have a high incidence in ESRD patients, including wrinkling, senile purpura, actinic keratoses, and diffuse hair loss. The prevalence of skin cancers does not appear to be increased unless the patient has received or is receiving immunosuppression.
Improved treatments in dialysis patients have resulted in changes in the frequency and types of skin disorders observed in conjunction with ESRD. Dermatologic conditions such as uremic frost, erythema papulatum uremicum, uremic roseola, and uremic erysipeloid now rarely occur. Pigmentary alterations, xerosis, ichthyosis, half-and-half nails, acquired perforating dermatosis, bullous dermatoses, pruritus, and calcific uremic arteriolopathy (CUA) are prevalent (Fig. 88-1), whereas nephrogenic systemic fibrosis is a rare and waning entity, now that the causative agent has been identified.1,2 The last four skin disorders are the focus of this chapter because they are associated with significant morbidity or mortality and represent an ongoing diagnostic or therapeutic challenge.
Uremic Pruritus
Clinical Manifestations
Uremic pruritus (UP) is a frequent symptom of ESRD with a reported prevalence ranging from 22% to 48%. Although its incidence in adult dialysis patients has declined as a result of improved dialysis efficacy and the introduction of so-called “biocompatible dialysis membranes,” pruritus remains a frustrating problem for patients, causing serious discomfort and skin damage, often in association with disturbance of day and night rhythm, sleeping disorders, depression, anxiety, and diminished quality of life.3,4 The intensity and spatial distribution of UP vary significantly among patients and over time throughout the course of renal disease. Excoriations, induced by uncontrollable scratching with or without superimposed infection, are frequently encountered in severely affected patients and rarely lead to prurigo nodularis, that is, a treatment-resistant lichenified or excoriated papulonodular chronic skin eruption (Fig. 88-2). The most frequently involved body areas are the back, limbs, chest, and face; 20% to 50% of patients report generalized pruritus.5
Pathogenesis
Many uremic factors are thought to contribute to UP. Parathyroid hormone (PTH) and divalent ions (calcium, phosphate, and magnesium) have been implicated because itching is a frequent symptom accompanying severe secondary hyperparathyroidism and elevated calcium-phosphate product. However, the lack of consistent correlations between serum and skin levels of PTH, calcium, phosphorus, and magnesium with the severity of UP indicates that other factors contribute to its development. Histamine released by mast cells has been implicated in UP. The number of dermal mast cells is increased in uremic patients, and higher tryptase and histamine plasma concentrations are reported in severe cases. Histamine release is triggered by substance P, a neurotransmitter involved in itch sensation. The role of elevated serotonin (5-hydroxytryptamine [5-HT3]) levels in dialysis patients with UP is debated; clinical trials using a selective inhibitor of 5-HT3 have yielded conflicting results (see later discussion). Xerosis is a common skin problem in dialysis patients (60% to 90%) that predisposes to UP. Skin dryness is caused by primary dermal changes associated with uremia, such as atrophy of sweat glands with impaired sweat secretion, disturbed stratum corneum hydration, sebaceous gland atrophy, and abnormal arborization of free cutaneous nerve fiber endings.
There are two major hypotheses of the mechanisms of UP. The opioid hypothesis proposes that UP is caused by overexpression of opioid µ receptors in dermal cells and lymphocytes. Consistent with this hypothesis, activation of the κ opioid system using a κ-receptor agonist was efficient in reducing pruritus in a mouse model. In contrast, the immune hypothesis considers UP an inflammatory systemic disease rather than a local skin disorder. Studies examining the beneficial effects of ultraviolet B (UVB) exposure on pruritus showed that UVB attenuates the development of Th1-type lymphocytes in favor of the Th2 type. Indeed, the number of CXCR3-expressing and interferon-γ–secreting CD4+ cells (indicating Th1 differentiation) is significantly increased in the circulation of dialysis patients with pruritus compared with those without. Levels of serum markers of inflammation, such as C-reactive protein, interleukin-2, and interleukin-6, are also higher in patients with UP.
Treatment
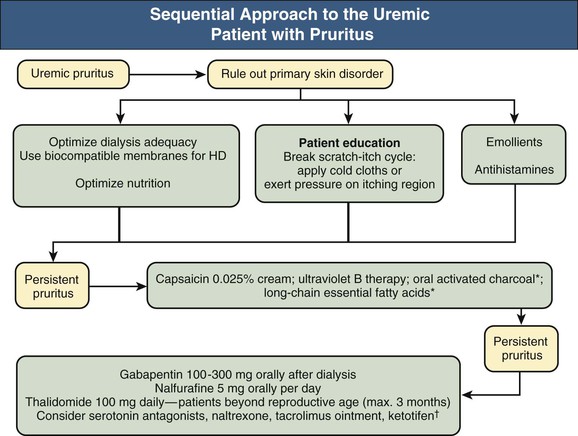
Common causes of UP in chronic kidney disease (CKD) and dialysis patients, such as primary skin disorders (e.g., urticaria, psoriasis, atopic and contact dermatitis), liver disease (e.g., hepatitis), and endocrine diseases (e.g., hypothyroidism, diabetes mellitus) should be ruled out and adequately treated. The treatment approach to UP is shown in Figure 88-3.
Optimizing Dialysis and Mineral Metabolism Therapy
Optimizing dialysis biocompatibility and efficacy and improving the nutritional status may result in a reduced prevalence and severity of UP. Adequate control of calcium and phosphorus serum concentrations by short-term use of dialysate with low calcium and magnesium concentrations ameliorated pruritus symptoms in only a few small studies and may lead to worsening of renal osteodystrophy in cases of prolonged use. Parathyroidectomy is not advocated for relief of UP because no consistent beneficial effects have been demonstrated.
Skin Emollients
Emollients continue to be the primary treatment given by nephrologists, although the literature is mixed on the overall efficacy of this approach. The use of simple emollients without perfumes or other additives is preferred. Continuous bath oil therapy containing polidocanol, a mixture of monoether compounds of lauryl alcohol and macrogol, seems to be of value for some patients. Sericin, a biopolymer protein from the silkworm (Bombyx mori) contains 32% serine, the main amino acid of the natural moisture factor in human skin, and suppresses the release of proinflammatory cytokines. Sericin was shown to effectively reduce UP score in a randomized, double-blind, placebo-controlled 6-week study in 50 dialysis patients.6
Antihistaminic Drugs
Classic antihistamines have limited efficacy and do not differ in efficacy compared with emollients; newer, second-generation antihistamines (e.g., desloratadine) might have some effect in UP. Ketotifen (2 to 4 mg/day), a putative mast cell stabilizer, was beneficial in one small study.
Phototherapy
Ultraviolet light, especially UVB (wavelength, 280 to 315 nm), is effective for treatment of UP and is well tolerated except for occasional sunburn. The duration of the antipruritic effect of thrice-weekly total body UVB therapy (total, 8 to 10 sessions) is variable, but it may last for several months. Potential carcinogenic effects of UV radiation require serious consideration, and its prolonged use is contraindicated in patients with a fair complexion (skin phototypes I and II).
5-Hydroxytryptamine Antagonist
Ondansetron, a selective 5-HT3 antagonist, was used successfully in a small study in peritoneal dialysis patients. However, a subsequent larger randomized, placebo-controlled study failed to show superiority over placebo in HD patients.
Opioid Receptor Agonists
A κ-opiate receptor agonist, nalfurafine, given intravenously after HD, was tested in two randomized, double-blind, placebo-controlled trials comprising 144 patients. Itching intensity, excoriations, and sleep disturbances were significantly reduced in patients receiving the active compound without an excess of drug-related side effects compared with placebo.7 Oral daily doses of 2.5 to 5 mg nalfurafine were equally effective in reducing UP scores compared with placebo during a 2-week treatment period in 337 dialysis patients.8 A subsequent 1-year study (n = 211) confirmed the sustained beneficial effect of 5 mg nalfurafine on UP, with the most frequently reported adverse events being insomnia (19%), constipation (7%), and increased blood prolactin concentrations.9
Gabapentin
Gabapentin, an anticonvulsant drug, administered after dialysis (300 mg) was effective in reducing pruritus. A reduced dose is required if it is given chronically to patients with ESRD, because it has a narrow therapeutic window, and it can accumulate and cause neurotoxic side effects.10 UP score was significantly reduced in two controlled studies after 4 weeks of gabapentin therapy at a dose of 100 to 300 mg administered thrice weekly after dialysis. Gabapentin was well tolerated; no patients stopped therapy because of side effects, which were limited to dizziness, somnolence, fatigue, and nausea. Similar effects were demonstrated in a smaller study using pregabalin.
Immunomodulators and Immunosuppressive Agents
A 7-day course of thalidomide reduced the intensity of UP by up to 80% in a placebo-controlled crossover study of 29 HD patients. Because of its strong teratogenic properties, thalidomide should probably be reserved for therapy-resistant severe UP in individuals outside the reproductive-age category. Adverse effects of thalidomide, such as peripheral neuropathy and cardiovascular side effects, limit its continuous longer use. A prospective, single-center study of 25 chronic dialysis patients with UP demonstrated that 6 weeks of treatment with tacrolimus ointment (0.1%) significantly reduced the severity of UP. Tacrolimus was well tolerated in this trial and caused no detectable systemic exposure or side effects.11 However, a subsequent, smaller vehicle-controlled trial showed equal relief of UP with vehicle and tacrolimus. The risks of long-term topical use of these agents are currently unknown, and their prolonged use is not recommended until more data are available.
Long-Chain Essential Fatty Acids
Oral administration of γ-linoleic acid (GLA)–rich primrose oil resulted in significant improvement of UP in chronic dialysis patients. Supplementation of GLA-rich primrose oil is thought to augment synthesis of anti-inflammatory eicosanoids. Similar effects could be obtained through use of fish oil, olive oil, and safflower oil.
Capsaicin
Capsaicin (trans-8-methyl-N-vanillyl-6-nonenamide) is a natural alkaloid found in the pepper plant that depletes the cutaneous type C sensory nerve endings of substance P. Two clinical studies showed that application of a 0.025% capsaicin cream significantly alleviated UP in dialysis patients, who exhibited no side effects.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree