Chapter 17 CLINICAL DIAGNOSIS OF OVERACTIVE BLADDER
TERMINOLOGY
Overactive bladder (OAB) is a newly described condition. It was probably first alluded to by Dudley in 1905 when he distinguished between active and passive incontinence due to sphincter weakness.1 In 1917, Taylor and Watt reported the importance of urgency, as a symptom, during history taking, to distinguish incontinence with and without urgency.2 Bates and colleagues introduced the term unstable bladder in 1970 when they used cinecysturethrography to investigate urge incontinence.3
The International Continence Society (ICS) established a committee for the standardization of terminology of lower urinary tract function to facilitate comparison of results and enable effective communication by investigators. Since 1976, a large number of standardization reports have been published, the latest in 2002.4–19
In 2002, the ICS subcommittee restated the principle of describing any lower urinary tract dysfunction from four aspects: as a symptom (taken by detailed history), a sign (physical examination and bedside tests), a condition, and a urodynamic observation in addition to the terminology related to therapies.1
 Increased daytime frequency is the complaint by the patient who considers that she voids too often by day. This term is equivalent to “pollakisuria,” a term used in many countries.
Increased daytime frequency is the complaint by the patient who considers that she voids too often by day. This term is equivalent to “pollakisuria,” a term used in many countries. Nocturia is the complaint that the patient has to wake at night one or more times to void. The term nighttime frequency differs from nocturia, because it includes voids that occur after the patient has gone to bed but before he or she has gone to sleep, as well as voids that occur in the early morning and prevent the patient from getting back to sleep as he or she wishes. These voids before and after sleep may need to be considered in research studies (e.g., nocturnal polyuria). If this definition were used, then an adapted definition of daytime frequency would need to be used with it.
Nocturia is the complaint that the patient has to wake at night one or more times to void. The term nighttime frequency differs from nocturia, because it includes voids that occur after the patient has gone to bed but before he or she has gone to sleep, as well as voids that occur in the early morning and prevent the patient from getting back to sleep as he or she wishes. These voids before and after sleep may need to be considered in research studies (e.g., nocturnal polyuria). If this definition were used, then an adapted definition of daytime frequency would need to be used with it. Urinary incontinence (UI) is the complaint of any involuntary leakage of urine. In each specific circumstance, UI should be further described by specifying relevant factors such as type, frequency, severity, precipitating factors, social impact, effect on hygiene and quality of life, measures used to contain the leakage, and whether the patient seeks or desires help because of UI. Urinary leakage may need to be distinguished from sweating or vaginal discharge.
Urinary incontinence (UI) is the complaint of any involuntary leakage of urine. In each specific circumstance, UI should be further described by specifying relevant factors such as type, frequency, severity, precipitating factors, social impact, effect on hygiene and quality of life, measures used to contain the leakage, and whether the patient seeks or desires help because of UI. Urinary leakage may need to be distinguished from sweating or vaginal discharge. Urgency urinary incontinence (UUI) is the complaint of involuntary leakage accompanied by or immediately preceded by urgency. UUI can manifest in various symptomatic forms; for example, as frequent small losses between micturitions or as a catastrophic leak with complete bladder emptying.
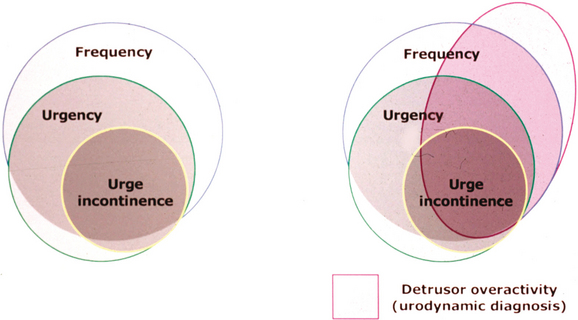
Urgency urinary incontinence (UUI) is the complaint of involuntary leakage accompanied by or immediately preceded by urgency. UUI can manifest in various symptomatic forms; for example, as frequent small losses between micturitions or as a catastrophic leak with complete bladder emptying.These symptom combinations of OAB are suggestive of detrusor overactivity (DO), a urodynamic diagnosis, which is characterized by involuntary detrusor contractions during bladder filling; it may be spontaneous or provoked. Figure 17-1 represents the relationships among OAB, UUI, and DO.
EPIDEMIOLOGY
Almost all surveys on UI concluded that stress urinary incontinence (SUI) is the most common type of UI in women. In the large Epidemiology of Incontinence in the County of Nord-Trondelag (EPINCONT) study, 50% of the incontinent women had SUI, 36% had mixed urinary incontinence (MUI), and 11% had UUI.20 The recent literature review by Minassian and colleagues reported similar prevalence rates for the various types of UI.21 The survey carried out by Diokno and associates22 showed that symptoms of MUI were most frequently reported; however, this study differed from the others in that only elderly people were assessed.
The results of these studies were based on symptoms only; if urodynamics had been used to confirm the diagnosis, the results might have been different. In one study with 863 women, most of the subjects with symptoms of MUI were diagnosed to have pure SUI (42%) during urodynamic testing.23 Weidner and Sanvik and their colleagues showed similar results.24,25 This reinforces the fact that SUI is the major type of UI in women.
A large population-based survey that was conducted in France, Germany, Italy, Spain, Sweden, and the United Kingdom defined OAB as the presence of chronic frequency, urgency, and urge incontinence (either alone or in any combination). This definition is somewhat different from the new ICS definition, which uses urgency as the cornerstone of the diagnosis. The authors reported that the overall prevalence of OAB symptoms in subjects aged 40 years or older was 16.6%. Frequency (85%) was the most commonly reported symptom, followed by urgency (54%) and urge incontinence (36%). The prevalence of OAB symptoms increased with advancing age. Overall, 60% of respondents with symptoms had consulted a doctor, but only 27% were currently receiving treatment.26
The NOBLE study does not support the commonly held notion that women are considerably more likely than men to have urgency-related symptoms. However, sex-specific anatomic differences may increase the probability that OAB is expressed as urge incontinence among women compared with men.27 The prevalence of OAB among women in this study was higher than what was reported by Milsom26 but similar to the prevalence of UI reported by Simeonova28 and by Samuelsson (20- to 59-year-olds).29
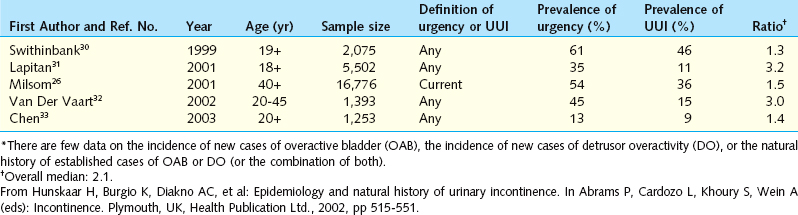
Not all studies distinguish wet from dry OAB. On average, urgency without UI appears to be as common as urgency with UI (Table 17-1).
EVALUATION
Quantification of Symptoms
Questionnaires
Taking a detailed history from the patient depends to a great deal on the physician’s skills. The questions, and the aspects tackled, are different for each clinician. Another issue is the embarrassment of the patient, which can lead her to avoid talking about some or all of her symptoms. In addition, clinicians tend to rate the patient’s quality of life lower than the patients themselves do.36 For all of these reasons, patient-completed questionnaires were developed. They provide details regarding the presence of symptoms, their frequency, their severity, and the bother caused to the patient. Questionnaires also assess quality of life in general and in relation to the symptoms. In theory, validated questionnaires can be used for making the diagnosis, as a tool in prevalence studies, and to measure the outcome of treatment.
Several questionnaires have been developed to assess UI. The modular International Consultation on Incontinence Questionnaire (ICIQ) has been validated and includes modules for lower urinary tract symptoms (LUTS) as well as OAB.37 ICIQ-OAB is a short form based on the Bristol Female Lower Urinary Tract Symptoms Questionnaire (BFLUTS) and should be a helpful tool in assessing these patients (Box 17-1).38,39 The full list of ICI questionnaires may be found by visiting the web site, www.iciq.net.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree