Chapter 17 Balloon Dilation of the Native and Postsphincterotomy Papilla
Endoscopic sphincterotomy has become the procedure of choice for removal of stones from the bile duct, especially in patients who have had a cholecystectomy.1,2 The procedure is successful in 90% to 98% of patients, and 86% to 91% of all bile duct stones can be extracted using this technique.3–5 Large stones, barrel-shaped stones, and tapering of the lower common bile duct (CBD) can make this procedure difficult6 and in such cases other techniques, such as mechanical lithotripsy, are required. After using mechanical lithotripsy, the success rate increases to 79% to 98%.7–11 However, endoscopic sphincterotomy is associated with adverse events such as bleeding, pancreatitis, and perforation,12–14 and concerns about causing permanent damage to sphincter function have led to the proposal and investigation of alternatives to sphincterotomy.
Endoscopic papillary balloon dilation (EPBD) is an alternative to endoscopic sphincterotomy (ES) for removing bile duct stones.15–18 In an effort to avoid permanent destruction of the biliary sphincter, EPBD seemed to be an attractive alternative to early investigators, such as Staritz and Meyer zum Buschenfelde, who first reported it in 1983.19 In this procedure a balloon is inflated to enlarge the opening of the bile duct at the level of the biliary sphincter. The main theoretical advantage of this technique is that it does not involve cutting the biliary sphincter. Therefore acute adverse events such as bleeding and perforation should be less likely, and the function of the biliary sphincter is also preserved.16
The enthusiasm for the potential advantages of EPBD over ES for the avoidance of short-term adverse events of bleeding and perforation, while preserving the biliary sphincter and possibly reducing the long-term sequelae of ES, was soon dampened by reports of serious postprocedure pancreatitis.20 Therefore EPBD was nearly abandoned as a treatment for bile duct stones, but its use was revived with the development of laparoscopic cholecystectomy. With several groups reporting favorable results using EPBD for stone extraction, conservation of the biliary sphincter regained popularity in the 1990s. In 1995 Mac Mathuna et al. reported good results with EPBD for treating bile duct stones in 100 consecutively treated patients.15,16
Video for this chapter can be found online at www.expertconsult.com.
The results of subsequent randomized controlled trials comparing ES to EPBD are conflicting. Some authors have reported an increased incidence of postprocedure pancreatitis while others have not, and an argument has been presented against EPBD and its failure to provide adequate access for extracting difficult (large or multiple) bile duct stones.17,18,21 The final success rates for ES and EPBD are comparable; the reported success rates of stone removal are 81% to 99% for EPBD15,17,18,21 and 85% to 98% for ES.17,18 Randomized trials comparing EPBD with ES suggest that EPBD is at least as effective as ES in patients with small to moderate-sized bile duct stones.16,17,21,22
The lower rate of stone clearance, along with a higher usage of mechanical lithotripsy in EPBD is most likely because EPBD does not enlarge the bile duct opening to the same extent as ES. Ersoz et al.6 reported the use of large balloon dilation after endoscopic sphincterotomy for removal of bile duct stones that were difficult to extract by conventional sphincterotomy and extraction devices. Endoscopic papillary large balloon dilation (EPLBD) has been introduced as an adjunctive tool to ES for removing large or difficult common bile duct stones. The concept is to combine the advantages of sphincterotomy with those of balloon dilation. Theoretically, risk of perforation or bleeding would be reduced by performing a less than maximal sphincterotomy, and risk of pancreatitis from balloon dilation would be reduced by first separating the biliary and pancreatic orifices with ES.
Technique of Balloon Dilation of the Native Papilla
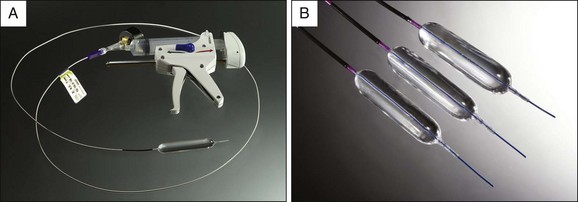
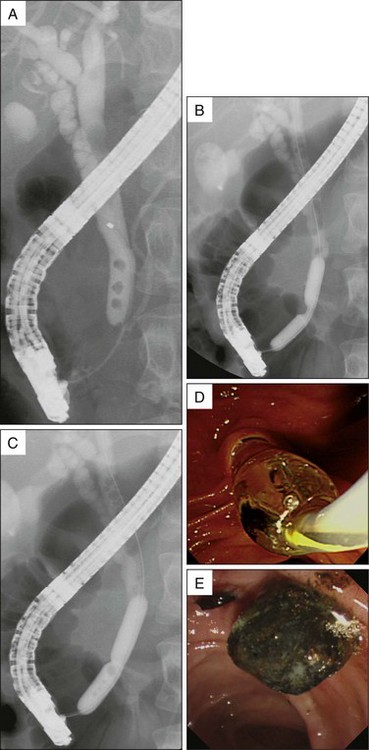
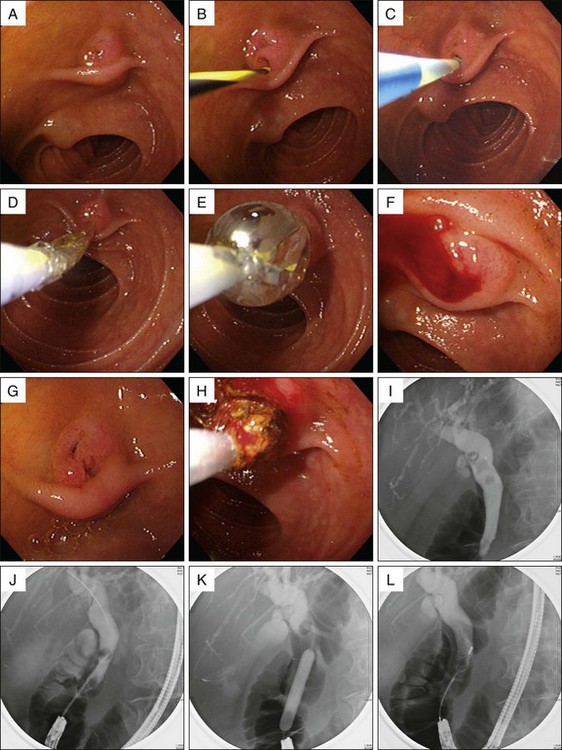
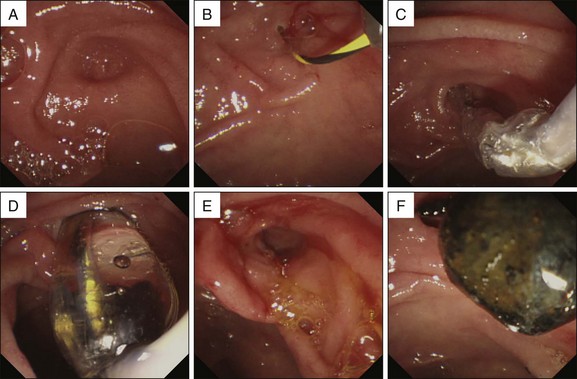
During the informed consent process, the risks and benefits of EPBD compared to ES should be discussed with patients and consent obtained if EPBD is being considered. Preprocedural antibiotics are administered as appropriate. The procedure is performed using a standard duodenoscope. During the procedure, identification of candidates for whom the EPBD is indicated can be simplified by comparing the bile duct stone size to the diameter of the duodenoscope on the same radiographic image; patients with stones that have a diameter equal to or less than that of the duodenoscope are considered eligible. After diagnostic ERCP and selective bile duct cannulation, a standard 0.025- or 0.035-in guidewire is inserted into the bile duct. After removing the cannula, a 6- to 10-mm balloon-tipped catheter (CRE Wireguided Balloon, Boston Scientific, Natick, Mass.) is passed over the guidewire (Fig. 17.1). The balloon is positioned so that two thirds of it is inside the distal CBD and a third of it is outside the papillary orifice and inflated with diluted contrast (Fig. 17.2). The balloon is expanded slowly with a mixture of contrast medium and saline (50/50), paying close attention to the waist of the balloon. When the waist disappears, the inflation is stopped. Care must be taken to avoid rapid application of excessive pressure (Fig. 17.2). The dilation is maintained for 15 to 30 seconds. When the bile duct is less than 8 mm in diameter, a 6 × 2–cm balloon can be used. Other dilator balloons can also be used. The smaller balloons pass readily through a diagnostic duodenoscope, such as an Olympus JF-240 260V, whereas the 24 Fr balloon requires a biopsy channel of at least 3.2 mm.
After papillary dilation, the stones are removed using Dormia baskets or retrieval balloon catheters (Fig. 17.2). Mechanical lithotripsy (BML-V237 QR-30 or BML-V242 QR-30, Olympus Medical Systems, Tokyo) can be used to fragment stones if they are over 10 mm in diameter as determined from the cholangiogram. The initial ERCP session is performed within 60 minutes, and if complete clearance of the stones fails, a biliary stent or nasobiliary catheter can be inserted to prevent stone impaction. Stent placement is not required after EPBD is performed.
Indications for EPBD
In the recent meta-analysis by Baron et al., the incidence of bleeding was significantly less after EPBD compared to ES.23 Clinically significant post-ES bleeding occurs in 2% to 5% of ES patients.12,22 In addition, patients with coagulopathy and those requiring anticoagulation within 3 days of the procedure are at increased risk for bleeding.12 Thus transient discontinuation of anticoagulation, correction of coagulopathy with fresh frozen plasma, or platelet transfusion are frequently used to avoid bleeding after ES, though these measures may be inadequate to prevent it. EPBD provides a useful alternative to ES in such cases. No articles have described bleeding after EPBD.15,17,18,21 In light of this, EPBD should be considered a viable alternative to ES in patients with an underlying coagulopathy or the need for anticoagulation following ES, as such patients have a higher incidence of post-ES bleeding.12 EPBD may significantly reduce the risk of bleeding compared to ES in patients with advanced cirrhosis and coagulopathy. In these patients, EPBD is recommended over ES for treating choledocholithiasis.24 Other populations in which EPBD may be an attractive option are those patients who refuse blood transfusion for religious reasons and patients with difficult anatomy that prevents safe orientation of the papillotome for ES (e.g., prior Billroth II gastrectomy, Fig. 17.3, or intradiverticular location of the papilla, Fig. 17.4).25
Bergman et al. reported a randomized trial of EPBD and ES for removing bile duct stones in patients with a prior Billroth II gastrectomy.25 Compared to patients with a normal anatomy, patients with a prior Billroth II gastrectomy had a significantly increased risk of bleeding after ES. Early adverse events occurred in 19% of the patients who underwent EPBD as compared to 39% of the patients who underwent ES. Endoscopic stone removal in patients with a prior Billroth II gastrectomy and Billroth II anastomosis poses one of the great challenges to the biliary endoscopist.
Currently the most widely accepted technique consists of a needle-knife sphincterotomy over a previously inserted endoprosthesis.26 Compared to standard ES in the normal anatomic situation, all of these techniques are more demanding and probably associated with a smaller sphincterotomy incision, less successful stone removal, and a higher rate of acute adverse events.25 When ES is used for such patients, careful consideration must be given to the direction and length of the incision, and a high level of skill is required to avoid severe adverse events. With EPBD, however, once a catheter is inserted into the common bile duct, the balloon catheter is simply inserted and the balloon is inflated. Therefore patients with Billroth II anatomy appear to be especially suited for stone removal using EPBD.
Limitations and Recommendation of EPBD
The success of stone removal and procedure time varies between EPBD and ES. Vlavianos et al. performed a univariate logistic regression analysis assessing the success of bile duct stone removal after EPBD. The following parameters were analyzed: sex, age, randomization, presentation with jaundice, acute cholangitis or acute pancreatitis, diameter of the CBD on the initial cholangiogram, number of stones, and size of the largest stone. Of these, age, diameter of the CBD, and size and number of stones were significantly associated with success. Multivariate logistic regression analysis showed that only the size of the largest stone was an independent predictor of success for duct clearance. On average these patients had a 12-mm diameter CBD and up to two 10-mm stones. These were taken as cutoff points in the statistical analysis.27
Larger stones are more difficult to remove using EPBD because the biliary opening is enlarged to a greater degree with ES. In fact, in the studies examined in the analysis by Baron et al. comparing EPBD to ES, many patients were excluded based on stone size or number. Patients were excluded if CBD stones had a diameter of 12,28 14,29 15,21 or 20 mm30 or if there were more than five30 or ten21 stones. The limitation of EPBD for extracting large bile duct stones is highlighted by the more frequent need for mechanical lithotripsy as an adjunctive procedure. This likely lengthens the procedure time. Indeed, in three studies used in this analysis, the protocol called for the use of mechanical lithotripsy in the EPBD group if the diameter of any CBD stone was 8,16 11,31 or 12 mm.32 Therefore EPBD may be more technically difficult to perform and more time consuming than ES.28
EPBD is a possible alternative to ES, especially in patients with impaired hemostasis. However, large stones may be difficult to remove with EPBD alone. Therefore ideal patients for selecting EPBD over ES (Box 17.1) are those with a limited number of CBD stones (≤3), CBD stones with a maximum diameter of 10 mm, and minimally dilated bile ducts.21,27,30,32 It is also important to use extreme caution when EPBD is applied in the following clinical settings: the presence of severe acute cholangitis, a history of previous or ongoing acute pancreatitis, age of 50 years or more, and difficult biliary cannulation,33 especially because of reports describing fatal pancreatitis in younger patients.34 In patients with severe cholangitis, one should consider placing a biliary stent to ensure adequate drainage if EPBD is performed. In the other clinical settings mentioned, placement of a pancreatic duct stent could be considered to prevent post-ERCP pancreatitis.
Adverse Events of EPBD
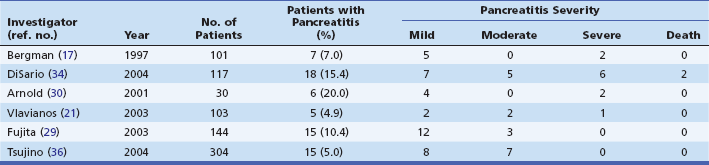
Early adverse events, defined as those occurring within 24 hours of the procedure, are pancreatitis, bleeding, infection (cholangitis or cholecystitis), and perforation. The meta-analysis of randomized controlled trials by Baron et al. showed that the early adverse event rate of EPBD was comparable to ES for removing common bile duct stones during ERCP.23 Overall, the early adverse event rates were similar in EPBD and ES, 10.5% versus 10.3%, p = 0.9. Of note, the bleeding rate was higher in the ES group (2.0% versus 0%, p = 0.001), while the rates of infection (2.7% for EPBD versus 3.6% for ES, p = 0.3) and perforation (0.4% versus 0.4%, p = 1.0) were similar (Table 17.1). The rate of pancreatitis was higher in the EPBD group (7.4% versus 4.3%, p = 0.05) (Table 17.1). One patient death occurred in each group, yielding a mortality rate of 0.2%.
Table 17.1 Procedure-Related Adverse Events Based on Prospective Trials Comparing Endoscopic Papillary Balloon Dilation (EPBD) and Endoscopic Sphincterotomy (ES) for Treating Choledocholithiasis
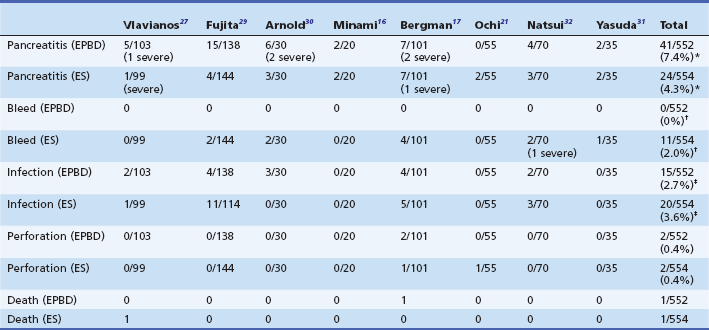
*p = 0.05 (pancreatitis in EPBD versus ES)
†p = 0.001 (bleeding in EPBD versus ES)
Hemorrhage is one of the most common and serious adverse events of ES, and the presence of coagulopathy is one of the risk factors for hemorrhage. In the meta-analysis by Baron et al.,23 bleeding was clearly reduced when EPBD was performed as compared to ES for the removal of CBD stones, but nearly all comparative studies of EPBD and ES excluded patients with coagulopathy and liver disorders. When bleeding occurs in cirrhotic patients, they may also develop further adverse events, such as hepatic failure. Komatsu et al. treated 24 cirrhotic patients with CBD stones using EPBD.18 Although hemostasis was impaired due to liver dysfunction, no bleeding occurred and all patients responded well to treatment. In particular, no adverse events were seen in four patients with Child-Pugh class C cirrhosis or in six patients with severe coagulopathy. The rate of ES-related hemorrhage was 30% (6 of 20 patients) whereas the rate for EPBD-related hemorrhage was 0% (p = 0.009). Regarding the rates of hemorrhage in relation to Child-Pugh class, most (n = 5) of the bleeding adverse events occurred in patients with Child-Pugh class C cirrhosis, while bleeding occurred in only one patient with Child-Pugh class B cirrhosis.24 Based on these results, EPBD appears to be the preferred strategy in patients with CBD stones and an underlying coagulopathy and those who require full anticoagulation within 72 hours of stone removal35 since these patients are at higher risk for postsphincterotomy bleeding following ES.12
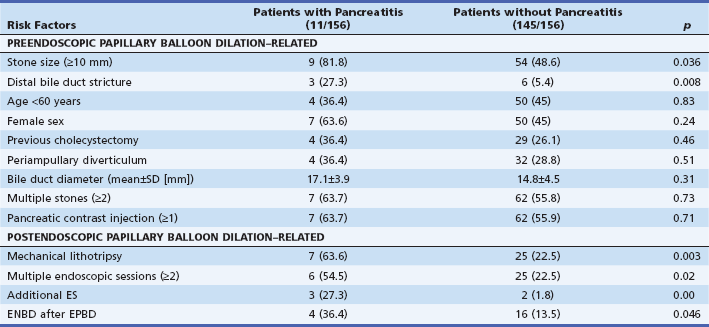
Procedure-related pancreatitis needs to be addressed. In recent years five prospective randomized controlled trials of EPBD versus ES have been performed.17,27,29,30 The frequency and severity of post-EPBD pancreatitis are summarized in Table 17.2.36 Of these, the Dutch12 and United Kingdom27 studies showed similar efficacy and safety between the two methods. Their incidence of pancreatitis was similar in patients undergoing EPBD and ES, in the range of 5% to 7%. In the Japanese study29 the rate of pancreatitis was slightly higher with EPBD than with ES; however, there were no reports of severe pancreatitis and all patients recovered with conservative treatment. In addition, Mac Mathuna et al.15 and Komatsu et al.18 conducted large-scale studies, but they were not randomized controlled trials; the incidence rates of pancreatitis were 5% and 7%, respectively. No severe pancreatitis or fatalities occurred (Table 17.2).
The mechanism of post-EPBD hyperamylasemia and pancreatitis is not clear, although it seems to be multifactorial. Balloon compression of the papilla or the pancreatic duct orifice may provoke peripapillary edema or sphincter of Oddi spasm.30,37 Bile duct cannulation per se or transpapillary manipulation (stone extraction, nasobiliary drainage) may also induce edema or spasm. The peripapillary edema or spasm may in turn obstruct the flow of pancreatic juice and eventually induce pancreatic edema or pancreatitis associated with hyperamylasemia.30,37 Contrast medium injection or cannulation of the pancreatic duct is also likely to have some effect on the pancreas and pancreatic secretions.38
Several studies have examined the risk factors for post-ERCP pancreatitis. The most important risk factors were related to either patient characteristics or the ease of cannulation. In the study by Bergman et al.,37 none of these factors was associated with EPBD-induced pancreatitis. However, a univariate analysis revealed that stone size, distal bile duct stricture, mechanical lithotripsy, multiple endoscopic sessions, additional ES, and endoscopic nasobiliary drainage after EPBD were significant risk factors for the development of acute pancreatitis after EPBD (Table 17.3), although in the multivariate analysis mechanical lithotripsy was the only risk factor for pancreatitis after EPBD (Table 17.4).39,40
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree