Chapter 36 AUTOLOGOUS FASCIAL SLINGS
HISTORICAL BACKGROUND
Slings are relatively old procedures; they have in use sporadically since the turn of the last century.1 Since the 1960s, slings have been used mainly to treat recurrent stress urinary incontinence (SUI) after one or more failed operative procedures and in reconstructive surgery on the urethra.2–4 These applications of the sling technique developed because operative failure was common for traditional SUI procedures. Anterior repairs failed at least 50% of the time, a rate which led to adoption of the retropubic suspension as the standard operation for SUI. Although retropubic operations had better outcomes than anterior repairs, they also had high late failure rates.5
Autologous fascial slings used to treat incontinence that persists or develops after a prior retropubic or needle suspension operative procedure have relatively good outcomes.6 Because good results were obtained in these cases and in other complex urethral reconstructive procedures performed with autologous slings, surgeons began using slings as a primary procedure for most patients with SUI. The introduction of slings made from synthetic materials was based on the realization that a sling provided superior support for the urethra. Early experience with synthetic slings was not good, but recent changes in materials used for slings have led to vastly improved results and dramatic decreases in the complications related to synthetic materials.
Uncomplicated primary SUI associated with urethral mobility can be very successfully treated with synthetic slings.7–9 Some authors have suggested that synthetic material slings can be used for severe intrinsic sphincter deficiency (ISD) and even for neuropathic urethral dysfunction.10,11 On the other hand, autologous fascial slings have an excellent record in reconstructive urethral surgery and in neuropathic urethral dysfunction, in which proximal urethral failure leads to severe incontinence.12–14 In these cases, compression of the urethra by the sling is a requirement to reestablish urethral continence function. Synthetic materials do not allow much tension to be applied, because they tend to erode into the urethra if used in that manner. There are data suggesting that patients with ISD, defined by videourodynamics, do not do as well with synthetic material slings.15
SPECIFIC INDICATIONS FOR AUTOLOGOUS PUBOVAGINAL SLINGS
Neuropathic Urethral Dysfunction
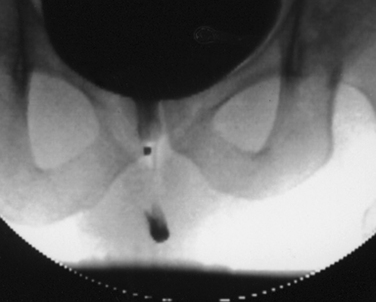
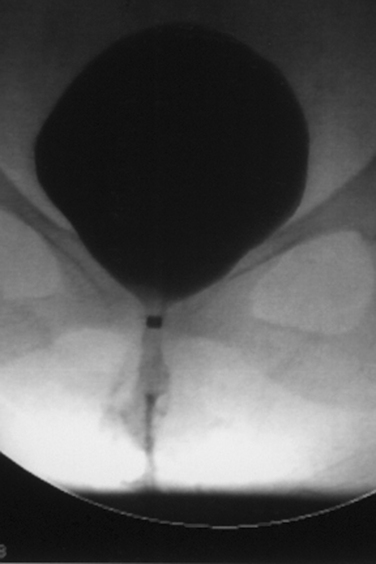
Neuropathic conditions are not always associated with urethral dysfunction, but specific neural conditions are associated with total absence, or loss of, proximal urethral function and severe SUI.16–18 Prototypical proximal urethral failure occurs in myelodysplasia affecting the lumbosacral area; in sacral agenesis; after injury to the T12-L1 spinal cord segments, where the sympathetic nerve supply to the urethra originates; and after peripheral pelvic neural injury, for example that sustained during extirpative surgery on the rectum or uterus. It can also occur in patients with pelvic fracture. All of these urethral conditions are associated with a neural lesion which almost always also produces decentralization of the bladder. The bladder is thus areflexic, but it is not flaccid by any means. The decentralized bladder reacts to volume increments, although the pressure developed is controlled by the magnitude of the outlet resistance associated with residual urethral closing function. That is, in an untreated situation, the bladder gains pressure related to incremental volume until the urethra leaks. Although the bladder can develop dangerously high pressures if the distal sphincter urethral resistance is high, proximal urethral function from the bladder outlet to the distal sphincter mechanism is simply lost. There is no function, reflex or static, in the proximal urethra. The urethra is open and stays that way (Fig. 36-1). This condition is associated with very low abdominal pressure–driven leakage from the urethra (Fig. 36-2). Leakage occurs with movement, transfers, coughing and straining, and the upright position.
Patients with proximal urethral and bladder decentralization after pelvic surgery preserve partial reflex and full volitional function of the distal sphincter. Partial preservation of reflex activity of the distal sphincter refers to the fact that sphincteric activity is no longer linked to detrusor behavior. There is no neural network to support that activity. Thus, relatively fixed urethral resistance is offered by the distal sphincter to detrusor pressure generated by incremental bladder volume. The latter is the result of constant urine production. Distal urethral closure does not mean that the urethra is stress competent, and severe SUI in men and women is the rule in these cases. Nevertheless, the distal sphincter closing function does require a certain detrusor pressure to induce leakage, and that can be a problem. This same situation occurs in the other causes of neuropathic urethral dysfunction, such as myelodysplasia and T12 spinal cord injury, although distal sphincter function is less well preserved in these cases.
A concrete risk of upper tract damage is related to the detrusor pressure at leakage.18 Although any urethral resistance results in changes in detrusor storage behavior, this is dangerous if the outlet resistance approaches 40 cm H2O. That degree of outlet resistance leads to high ambient storage pressures that overwhelm ureteral peristaltic function. One example of this are the problems that developed in children with myelodysplasia treated with a bladder neck artificial sphincter. The device effectively raised both the detrusor and abdominal leak point pressure and was associated with upper tract deterioration.19 Similar problems were associated with the Kropp urethral reimplantation procedure in children with myelodysplasia.20
The problem here is to gain closure of the proximal urethra without increasing the detrusor leak point pressure. Slings—either the standard posterior vector force sling, the fascial urethral wrap, or the crossover sling—increase the Valsalva leak point pressure substantively but change the detrusor leak point pressure either very slightly or not at all.4 Therefore, these are safe procedures.
Acquired Urethral Incompetence
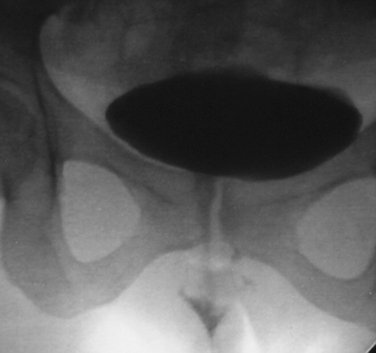
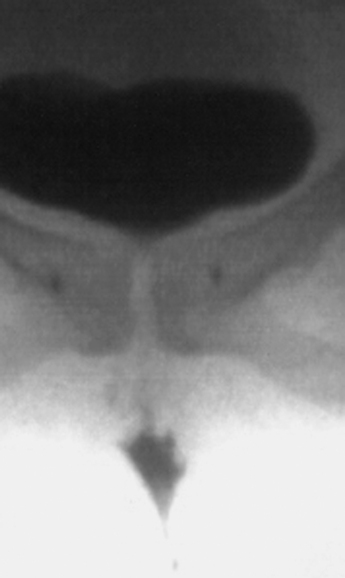
Severe loss of proximal urethra function can occur after erosion of synthetic slings into the urethra, after urethral diverticulectomy, or in association with other types of urethral trauma, including surgery (Figs. 36-3 and 36-4). Acquired loss of proximal urethral function is associated with a very low abdominal leak point pressure but usually with little or no urethral mobility on an upright videourodynamic study. Erosion into the urethra after placement of synthetic slings or of donor fascia slings suspended with bone anchors can be associated with urethrovaginal fistulas that are difficult to recognize in the face of severe constant urethral urinary loss.
Very severe urethral dysfunction is also associated with chronic indwelling catheters, especially in patients with neurogenic conditions, in whom complete loss of closing function often occurs. In addition, complete or partial urethral erosion is associated with chronic catheterization (Fig. 36-5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree