Chapter 33 Approach to the Dilated Bile Duct and Pneumobilia
The Dilated Bile Duct
Defining Dilated Bile Ducts
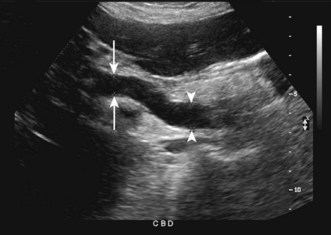
Dilation may be present in the isolated intrahepatic ducts, in the extrahepatic duct, or in both. If dilation is secondary to obstruction at a distal lesion, diffuse dilation of both intrahepatic and extrahepatic bile ducts will usually be seen. If obstruction is at a more proximal site, focal intrahepatic dilation will usually be observed. Normal intrahepatic ducts as small as 1 to 2 mm are seen as scattered and nonconfluent biliary branches on abdominal computed tomography (CT) or ultrasonography, and become confluent and more easily imaged as they move centrally, with diameters exceeding 2 mm (Fig. 33.1).1 Abnormal intrahepatic ducts are present when duct diameter exceeds 40% of the diameter of the adjacent intrahepatic portal vein and when the ducts appear as parallel tubes coursing together.1

Fig. 33.1 Extracorporeal ultrasound examination demonstrating intrahepatic ductal dilation (arrowheads).
An increase in diameter of the extrahepatic bile ducts, in particular the common hepatic duct (CHD) or common bile duct (CBD), is most often what is referred to as biliary dilation. The normal size of the duct varies at different levels and it varies from person to person based on individual characteristics.1,2 Numerous potential factors have been elucidated that may affect the measured diameter of normal extrahepatic ducts.
First, the imaging modality used to evaluate the biliary system can influence the reported duct diameter. Extracorporeal ultrasonography measures the internal diameter of the duct (Fig. 33.2).2,3 Measurements of the CHD are typically obtained at the level of the hepatic artery in the porta hepatis, anterior to the main or right portal vein; measurements of the CBD are obtained more proximal to this site.1,4 Using ultrasound, most studies have placed the upper limit of normal for the diameter of the CBD at 6 to 8 mm and that of the CHD at 6 mm.1,4–7 However, several studies using ultrasound have reported a different range and studies using different imaging modalities have reported various ranges. For example, a study using ultrasound to measure CBD diameters recorded normal values up to 8 to 10 mm in completely asymptomatic patients.5 This may reflect variation among operators obtaining the measurements and among interpreters of these imaging modalities. On CT, values of 8 to 10 mm are more commonly accepted as normal for the CBD (Fig. 33.3).1,2 This difference is in part due to measurements performed at different locations along the duct. Unlike ultrasound, CT can more easily image the mid to distal portions of the CBD, which are often larger in diameter.1 It also more readily identifies the fat around the duct and measurements by CT generally include the duct wall. Evaluation of the biliary system with cholangiogram, by endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic cholangiography (PTC), may also yield results different than those with other imaging techniques. A study of 135 patients who underwent imaging of their extrahepatic bile ducts with ultrasound and ERCP or PTC demonstrated normal duct size of up to 4 mm by ultrasound versus 10.4 mm and 10.6 mm by ERCP and PTC, respectively.8 This was likely a result of radiographic magnification of the cholangiogram and may also reflect distension from contrast injection.
Second, patient characteristics can affect measurement of duct size. One previously described study5 noted a trend toward increasing CBD diameters in older individuals, supporting a belief that the duct size may increase with age. Based on this hypothesis, authors have proposed adding 0.4 mm to the upper limit of normal for duct size for each decade of life or 1 mm per decade of life after age 60 years.7,9,10 However, a large ultrasound study of 1018 asymptomatic adults demonstrated a slight trend toward an increase in duct size with age but not as large as had been previously reported, with a mean diameter of 3.6 mm at age 60 years and 4 mm at age 85 years.7 In this study, 99% of patients had a CBD diameter less than 7 mm.
Patient characteristics other than age can affect the upper limit of normal for the CBD. Since Oddi first predicted the phenomenon in 1887, dilation of the CBD after cholecystectomy has remained controversial.11 Several prospective studies found no ductal dilation on ultrasound in patients before and after cholecystectomy.12,13 However, other studies have demonstrated a slight trend toward ductal dilation after cholecystectomy that was statistically significant over time.14–17 In a study of 234 patients undergoing cholecystectomy, the CBD increased after surgery from a mean of 5.9 mm before cholecystectomy to 6.1 mm at an average of 393 days after cholecystectomy.17 As in other studies, where dilation of the CBD was seen after surgery, the increase in diameter was on the order of 1 to 2 mm in the majority of patients. It has been suggested that the upper limit of normal based on ultrasound be adjusted to 8 mm in such patients.15 In a study of 24 patients undergoing elective cholecystectomy, two asymptomatic patients with normal laboratory results were noted to have an increase in ductal diameter of 4 mm or more with duct diameters of >9 mm and >10 mm at 5 years after cholecystectomy.16 Though most patients have minor if any dilation after cholecystectomy, there are clearly those who may manifest a more profound asymptomatic dilation of the ducts.
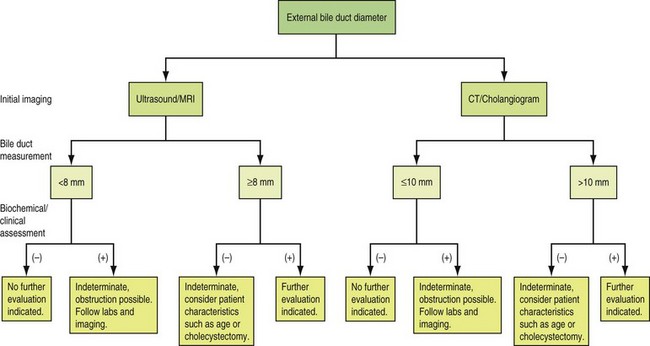
Finally, factors such as time of day, respiration, or patient positioning have all been shown to affect the normal caliber of the CBD.18–20 Given all possible circumstances that may affect the measurement of the extrahepatic biliary system, it is difficult to define an absolute measurement that will by itself yield satisfactory predictive values for pathologic dilation of the bile duct. Instead, duct diameter should be interpreted in the context of potential causes of obstructive or nonobstructive biliary dilation so that any pertinent findings from the clinical presentation or biochemical tests may be considered in the decision to pursue further diagnostic evaluation (Fig. 33.4).
Etiology
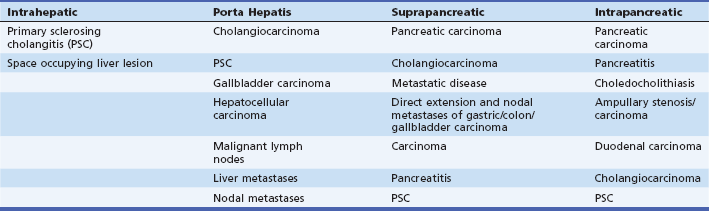
Once a dilated bile duct is noted and considered to be pathologic, identifying the etiology is the next step. Dilated bile ducts may be secondary to obstructive lesions or to nonobstructive lesions; obstructive lesions are more commonly encountered in the adult. Common causes of obstruction include both neoplastic and benign etiologies (Table 33.1).1,21,22 Among the most common etiologies for bile duct dilation in the United States is choledocholithiasis. Less common as an etiology in the United States, but more common worldwide, are infections such as parasitic diseases. A study on the use of endoscopic ultrasound (EUS) in the evaluation of a dilated biliary tree in 90 patients with an unrevealing abdominal ultrasound found 40 patients with choledocholithiasis, 13 with malignancy, 8 with benign stricture, 2 with choledochal cysts, 1 with Ascaris infection, and 24 dilated ducts without evidence of an obstructing lesion.23 These numbers are similar to other studies that have demonstrated the following general results in order of decreasing prevalence: choledocholithiasis, pancreatic cancer, ampullary carcinoma, and cholangiocarcinoma as causes of biliary dilation.6 Nonobstructive bile duct dilation can be seen in patients with choledochal cysts. Choledochal cysts are congenital malformations of the biliary system that result in varying degrees of biliary dilation. These cysts are important to recognize and classify because of the high associated risk of malignant transformation. Choledochal cysts are generally described by the Todani classification system in which type 1 represents a solitary cystic dilation of the CBD; type 2 represents an isolated diverticulum of the CBD; type 3 is a bulbous cyst in the distal most CBD within the intraduodenal segment of the CBD; type 4 is characterized by multiple cysts either in the CBD alone or in both the CBD and the intrahepatic ducts; and type 5 represents isolated intrahepatic dilation, known as Caroli disease. A further discussion of choledochal cysts can be found in Chapter 32. Assessing the a priori likelihood of a particular disease given the clinical scenario should influence the choice of the subsequent diagnostic evaluation.
Evaluation
Clinical Evaluation
The clinical presentation should be assessed for any signs or symptoms relating to biliary obstruction or its cause. For example, a thorough history should be obtained, including the presence or absence of symptoms such as abdominal pain, fever, weight loss, jaundice, pruritus, acholic stools, dark urine, or steatorrhea. The physical exam may be limited in its utility but special attention should be paid to the presence of abdominal tenderness or mass, hepatomegaly, jaundice, or lymphadenopathy. A positive history or physical examination may serve to lower the threshold for further diagnostic evaluation in those patients with an equivocal duct size on initial imaging. In the era of laparoscopic cholecystectomy, studies have attempted to develop models of clinical features in addition to biochemical values to predict choledocholithiasis prior to surgery. Some of these studies have demonstrated an increased likelihood for choledocholithiasis with jaundice or fever at presentation, acholic stools, dark urine, or an older patient age.24–27 However, it is difficult to draw a clear conclusion from these studies, as they differ in methodology and results.
Biochemical Evaluation
The principal markers of cholestasis are bilirubin and AP.28–30 The total bilirubin present in the serum represents a balance between input from production and output from hepatobiliary removal. In obstructive jaundice the serum bilirubin is principally in the conjugated form (water soluble). Hepatobiliary AP is present on the apical membrane of the hepatocyte and in the luminal bile duct epithelium. Increases in AP result from increased synthesis and release into the serum. As a result, levels may not rise until 1 to 2 days after biliary obstruction occurs. In addition, the enzyme has a half-life of 1 week and may therefore remain elevated for several days even after the resolution of biliary obstruction. Levels of AP up to three times normal are relatively nonspecific and occur in a variety of liver diseases. However, higher elevations are more specific for biliary obstruction (intrahepatic or extrahepatic) and infiltrating liver diseases. As AP can be produced in sources outside the liver, it may be necessary in certain instances to use other biochemical tests such as the AP isoenzymes or the gamma-glutamyl transpeptidase or 5′-nucleotidase to confirm the hepatobiliary etiology of an elevated AP.
The serum aminotransferases include AST and ALT. Transient elevations within 1 to 2 days with levels into the thousands may occur in acute CBD obstruction, from trauma, or typically in the instance of choledocholithiasis with subsequent rapidly declining levels.28–30 Aminotransferase levels may also rise from other subacute or chronic obstructions but typically remain less than 500 IU/dL.
It is difficult to interpret the predictive models using these markers in evaluating obstruction from choledocholithiasis, as the results vary among studies.24–27 In general, there is an increased likelihood for choledocholithiasis with abnormalities in bilirubin, AP, and transaminase levels. With these studies in mind, one can predict that it would be unusual for a lesion to cause biliary obstruction and dilation without any clinical or biochemical abnormality. However, this is not universal, and there have been case reports of patients with normal LAEs despite both dilated ducts and choledocholithiasis.31
Imaging
Ultrasound
Ultrasound is often the first-line imaging technique in the evaluation of the bile duct, gallbladder, and right upper quadrant (RUQ) and is usually the test initially demonstrating dilation of the bile duct. Ultrasound is noninvasive, inexpensive, and a quick procedure that may be done at the bedside. It does, however, require experience in technique and interpretation and may be limited due to interference from gas within the surrounding bowel or body habitus. Ultrasound has been shown to be one of the most accurate imaging studies in the evaluation of cholelithiasis, with both a sensitivity and specificity of up to 99%.4,32–34 It is also highly sensitive for detecting dilation of the biliary tree as a whole with a sensitivity greater than 90%.4,35 The ability of ultrasound to define the site and cause of biliary obstruction is slightly less reliable. A review of the literature with more than 700 patients demonstrated that ultrasound has a sensitivity of 71% in delineating the level of obstruction, a sensitivity of 57% in defining the etiology, and a sensitivity for choledocholithiasis of 32%.32 However, there is great variation with sensitivities ranging from 27% to 95% for the correct level of obstruction and 23% to 81% for the correct cause of obstruction.36–39 Some of this limitation may result from a relative inability to image the distal CBD due to bowel gas. This area is only well visualized in 40% to 50% of patients.4 Clearly the ease of use, widespread availability, and few contraindications place ultrasound early in the algorithm for evaluation of the biliary tract, but it may lead to further studies as it is often inconclusive and does not provide adequate staging or surgical information in the setting of suspected neoplasms.
Computed Tomography
Multidetector CT can obtain images at thin 1.25- to 2.5-mm intervals that can be reformatted with high resolution into views to reproduce the biliary tree.1,40,41 This technique, in conjunction with careful review of axial images, can provide a complete evaluation of the bile ducts. Infusion of intravenous (IV) contrast agents is necessary, to provide vascular landmarks and organ opacification, maximizing the visualization of the bile ducts.40 Unenhanced scans can highlight the presence of calcifications and aid in visualization of choledocholithiasis. Water may be used as an oral contrast agent when biliary tract abnormalities are suspected so as not to obscure potential pathology at the level of the ampulla of Vater.40 CT cholangiography has been evaluated in the United States and is used extensively in Asia and Europe. This employs the administration of IV contrast material to highlight the biliary tree. CT cholangiography has certain limitations, however, including that obstruction limits contrast excretion into the bile ducts and the higher incidence of adverse reactions to contrast agents.42 With new contrast agents and multidetector CT, this may be the preferred imaging technique in the future.
In a study evaluating the presence of biliary obstruction, defined as extrahepatic bile duct diameter >8 mm, the sensitivity and specificity of CT for diagnosing dilated ducts was 96% and 91%, respectively.40 CT is also accurate at defining the level of obstruction in 88% to 97% of cases as well as the cause of obstruction in 70% to 95% of cases.39,40,43,44
Although CT is a readily available test that can accurately identify a dilated CBD as well as provide important details as to the level and cause of obstruction, it too has limitations. It requires IV contrast for enhanced images, which may lead to adverse reactions, including potential nephrotoxicity. It also lacks sensitivity for a common cause of obstruction, choledocholithiasis, which is likely responsible for the lower rates of detection of the etiology of obstruction; approximately 20% to 25% of biliary stones are isoattenuating with bile, making them difficult to detect on CT.1,40 Sensitivity of CT for choledocholithiasis ranges from 70% to 94% depending on the use of indirect signs of obstruction that typically coincide with choledocholithiasis.1,45,46
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree