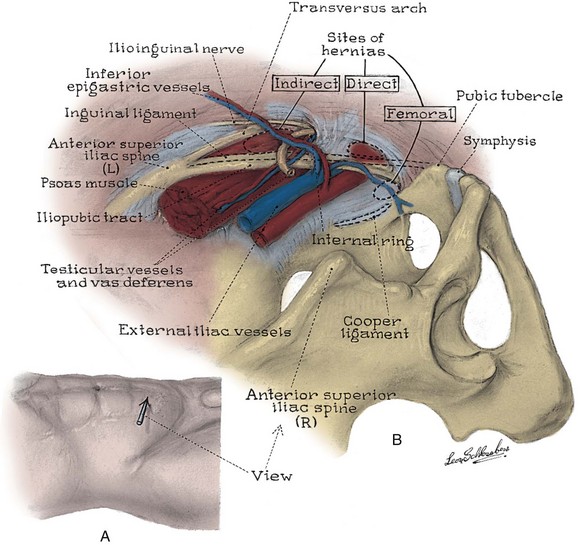
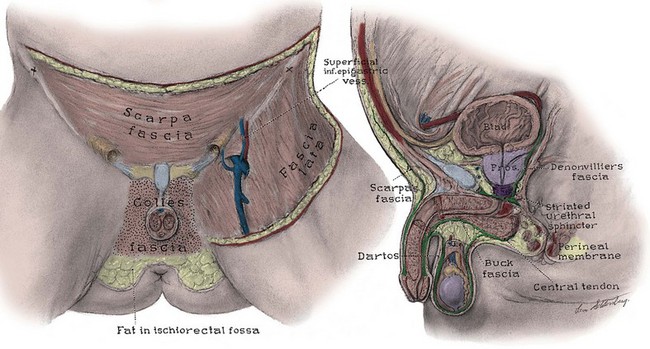
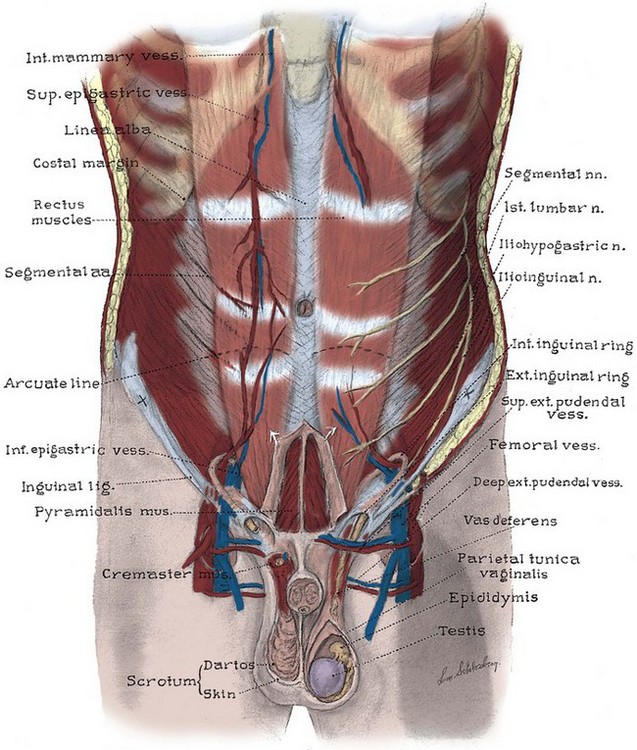
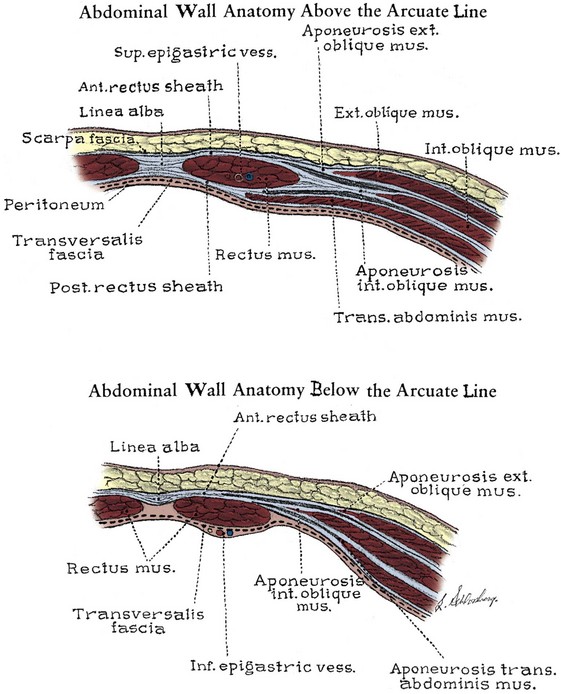
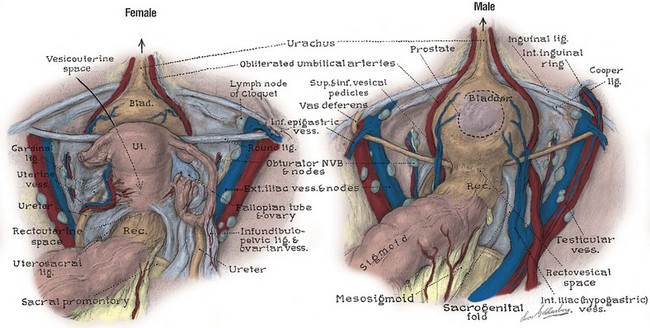
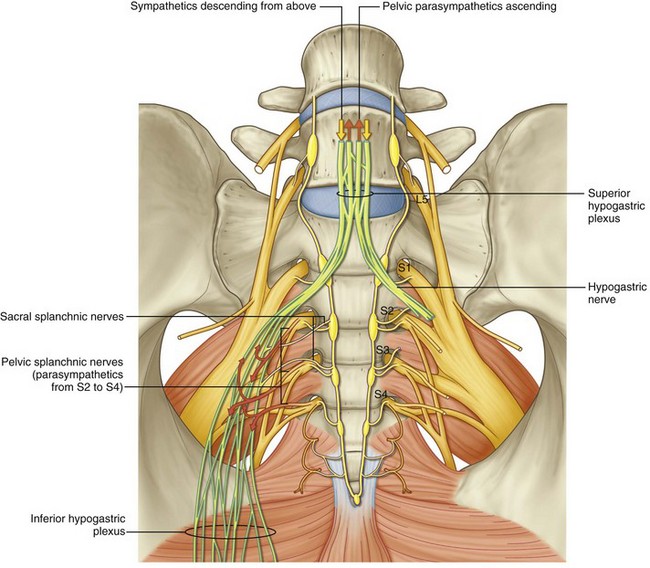
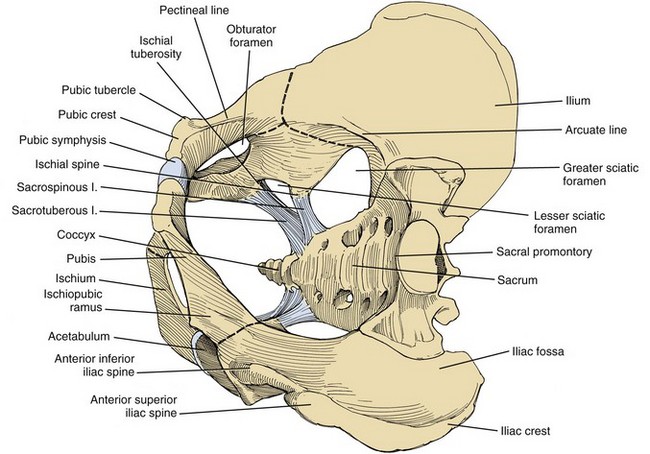
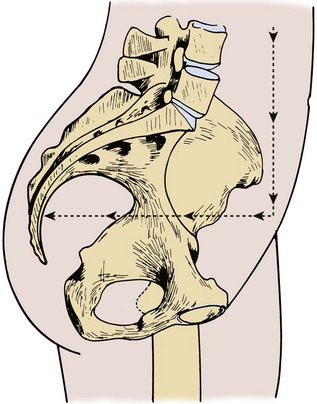
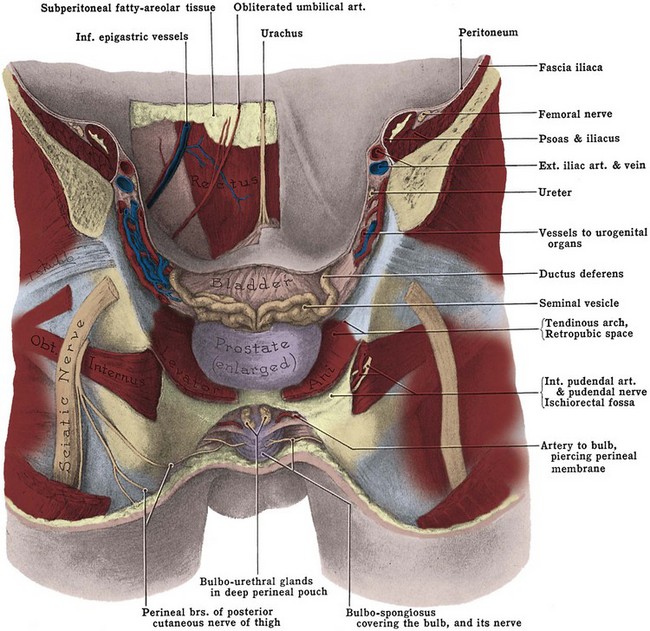
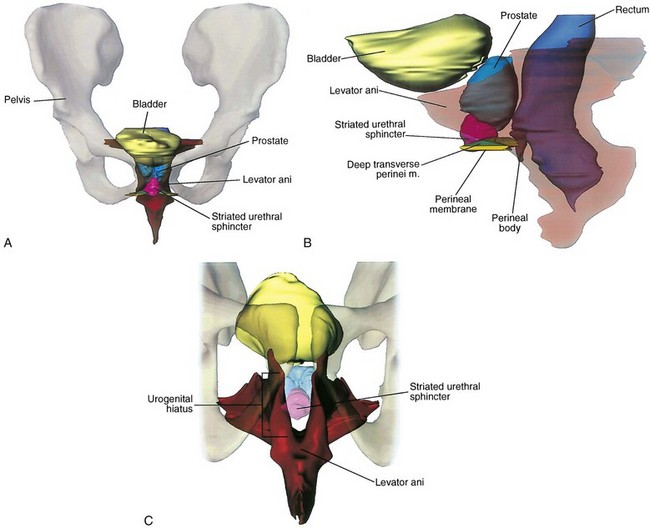
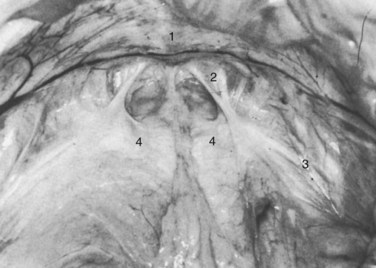
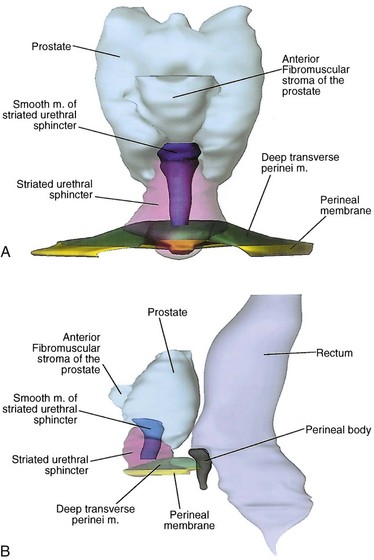
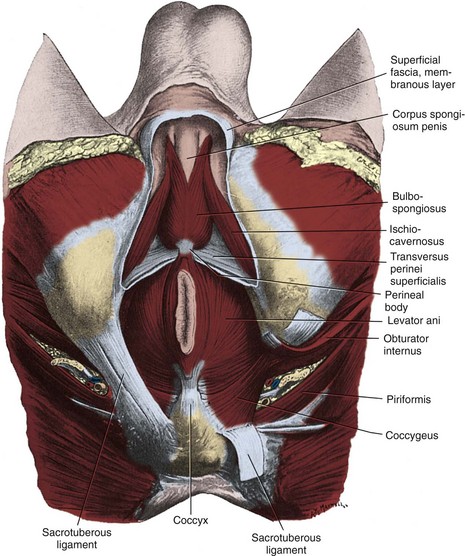
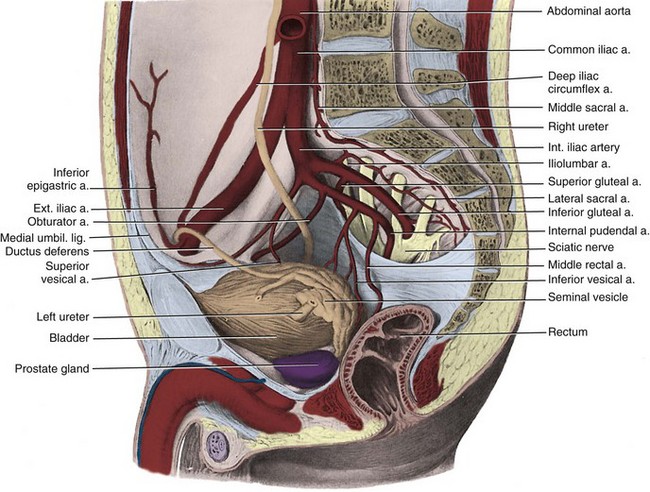
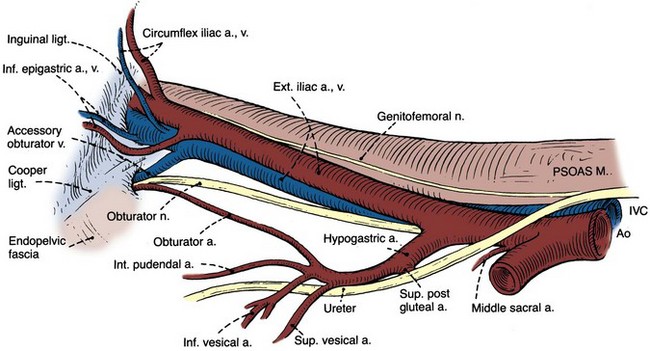
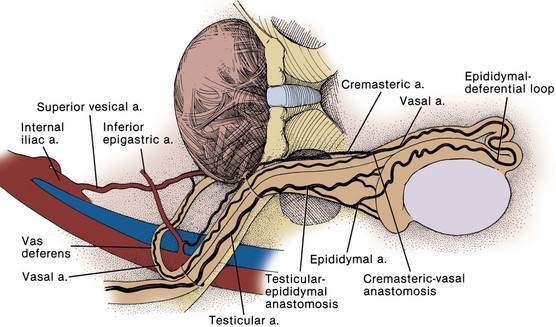
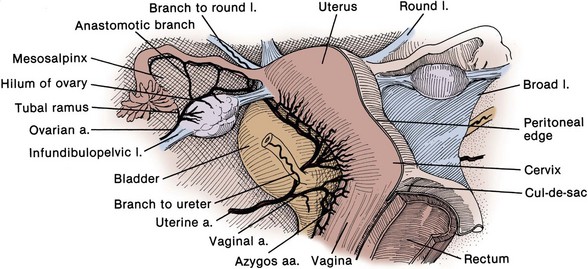
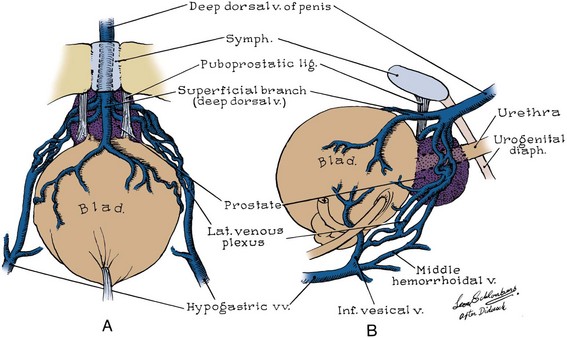
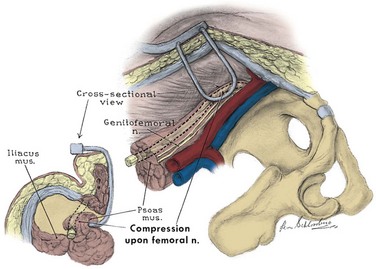
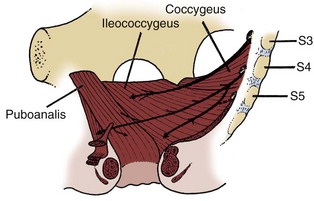
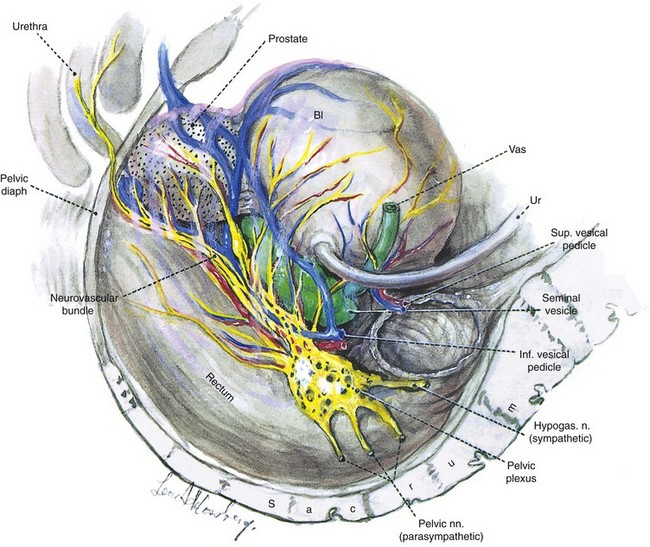
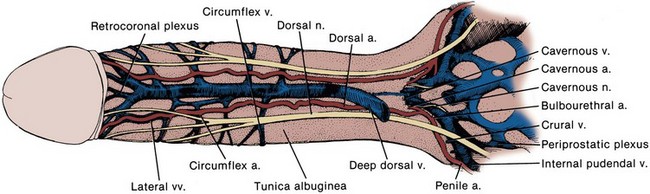
Benjamin I. Chung, MD, Graham Sommer, MD, James D. Brooks, MD The pelvic bones are the sacrum (the termination of the axial skeleton) and the two innominate bones. The latter are formed by the fusion of the iliac, ischial, and pubic ossification centers at the acetabulum (Fig. 2–1). The ischium and pubis also meet below, in the center of the inferior ramus, to form the obturator foramen. The weight of the upper body is transmitted from the axial skeleton to the innominate bones and lower extremities through the strong sacroiliac (SI) joints. As a whole, the pelvis is divided into a bowl-shaped false pelvis, formed by the iliac fossae and largely in contact with intraperitoneal contents, and the circular true pelvis wherein the urogenital organs lie. At the pelvic inlet, the true and false pelves are separated by the arcuate line, which extends from the sacral promontory to the pectineal line of the pubis. The lumbar lordosis that accompanies erect posture tilts the axis of the pelvic inlet so that it parallels the ground; the pelvic inlet faces anteriorly, and the inferior ischiopubic rami lie horizontal (Fig. 2–2). When approaching the pelvis through a low midline incision, the surgeon gazes directly into the true pelvis. Figure 2–1 The bones and ligaments of the pelvis. (From Hinman F Jr. Atlas of urosurgical anatomy. Philadelphia: WB Saunders; 1993. p. 196.) Figure 2–2 Pelvis in standing position. The axis of the pelvic cavity is horizontal because of lumbar lordosis. (From Zacharin RF. Pelvic floor anatomy and the surgery of pulsion enterocele. New York: Springer-Verlag; 1985. p. 15.) The anterior and posterior iliac spines, the iliac crests, the pubic tubercles, and the ischial tuberosities are palpable landmarks that orient the pelvic surgeon (see Fig. 2–1). Cooper (pectineal) ligament overlies the pectineal line and offers a sure hold for sutures in hernia repairs and urethral suspension procedures (Fig. 2–3). The ischial spine is palpable transvaginally and attaches to the pelvic diaphragm and the sacrospinous ligament. The sacrospinous ligament separates the greater and lesser sciatic foramina. Together with the sacrotuberous ligament, it stabilizes the SI joint by preventing downward rotation of the sacral promontory. The SI joint, synovial in type, gains additional strength from anterior and posterior ligaments. In pelvic trauma, fractures virtually never involve this joint but occur adjacent to it. The pubes, the thinnest of the pelvic bones, are nearly always fractured, and their fragments may injure the adjacent bladder, urethra, and vagina. Resection or congenital nonunion of the pubes (e.g., bladder exstrophy) does not affect ambulation because of the strength of the SI joint (Waterhouse et al, 1973; Golimbu et al, 1990). To minimize scarring, incisions of the anterior abdominal wall and flank should follow Langer lines of cleavage. These lines parallel dermal collagen fibers and are oriented along lines of stress. They correspond to the segmental thoracic and lumbar nerves. The skin is backed by Camper fascia, a loose layer of fatty tissue that varies in thickness with the nutritional status of the patient. The superficial circumflex iliac, external pudendal, and superficial inferior epigastric vessels branch from the femoral vessels to run in this layer (Figs. 2-4 and 2-5). The superficial inferior epigastric vessels are encountered during inguinal incisions and can cause troublesome bleeding during placement of pelvic laparoscopic ports. Scarpa fascia forms a distinct layer deep to Camper fascia, although it may be difficult to discern in older patients. Superiorly and laterally, it blends with Camper fascia. Inferiorly, it fuses with the deep fascia of the thigh 1 cm below the inguinal ligament along a line from the anterior superior iliac spine to the pubic tubercle. Medially, it is continuous with Colles fascia of the perineum (see Fig. 2–4). Colles fascia attaches to the posterior edge of the urogenital diaphragm and the inferior ischiopubic rami. It is continuous with the dartos fascia of the penis and scrotum. These fasciae can limit both the spread of infection in necrotizing fasciitis of the scrotum (Fournier gangrene) and the extent of urinary extravasation in an anterior urethral injury. For instance, blood and urine can accumulate in the scrotum and penis deep to the dartos fascia after an anterior urethral injury. In the perineum, their spread is limited by the fusions of Colles fascia to the ischiopubic rami laterally and to the posterior edge of the perineal membrane; the resulting hematoma is therefore butterfly shaped. Because of these fasciae, bleeding, infection, or urinary extravasation will not extend down the leg or into the buttock but can freely travel up the anterior abdominal wall deep to Scarpa fascia to the clavicles and around the flank to the back. The abdominal musculature lies immediately below Scarpa fascia. The origins of the external oblique, internal oblique, and transversus abdominis muscles and the orientation of their fibers are presented in Chapter 1. These muscles terminate on the anterior abdominal wall as broad, tough aponeurotic sheets that fuse in the midline (linea alba) and form the rectus sheath (see Fig. 2–5). The linea alba is avascular and is a convenient point of access to the peritoneal and pelvic cavities. In its upper portion, the anterior rectus sheath is formed by the aponeurosis of the external oblique muscle and a portion of the internal oblique muscle (Fig. 2–6). The posterior sheath is derived from the remaining internal oblique aponeurosis and the transversus abdominis aponeurosis. Two thirds of the distance from the pubis to the umbilicus, the arcuate line is formed, as all aponeurotic layers abruptly pass anterior to the rectus abdominis, leaving this muscle clothed only by transversalis fascia and peritoneum posteriorly. The rectus abdominis arises from the pubis medial to the pubic tubercle and inserts on the xyphoid process and adjacent costal cartilages. The muscle is crossed by three or four tendinous intersections that are firmly attached to the anterior rectus sheath; thus the muscle can be divided transversely without significant retraction. It is supplied by the last six thoracic segmental nerves that enter it laterally. Paramedian incisions lateral to the rectus divide these nerves, cause atrophy of the rectus, and predispose to ventral hernia. Anterior to the rectus and within its sheath, the triangle-shaped pyramidalis muscle arises from the pubic crest and inserts into the linea alba (see Fig. 2–5). It is supplied by the subcostal nerve (T12). The inguinal canal transmits the spermatic cord in the male, the round ligament in the female, and the ilioinguinal nerve in both sexes (Fig. 2–7; see also Fig. 2–5). Its anterior wall and floor are formed by the external oblique muscle, which folds over at its inferior edge as the inguinal ligament. Above the pubic tubercle, the fibers of the external oblique aponeurosis split to form the lateral edges (crura) of the external inguinal ring. Transverse (intercrural) fibers bridge the crura to form the superior edge of the external ring. By dividing the intracrural fibers, the external oblique can be separated along its fibers to gain access to the cord. The posterior wall of the canal is formed by the transversalis fascia, which lines the inner surface of the abdominal wall. The cord structures pierce this fascia lateral to the inferior epigastric vessels at the internal inguinal ring (see Fig. 2–3). The internal inguinal ring lies midway between the anterior superior iliac spine and the pubic tubercle, above the inguinal ligament, and 4 cm lateral to the external ring. Fibers of the internal oblique and transversus abdominis arise from the iliopsoas fascia and inguinal ligament lateral to the internal ring and arch over the canal to form its roof. They fuse as the conjoint tendon, pass posterior to the cord, and insert into the rectus sheath and pubis. The conjoint tendon reinforces the posterior wall of the inguinal canal at the external ring. With contraction of the internal oblique and transversus muscles, the roof of the canal closes against the floor, preventing herniation of intra-abdominal contents into the canal. Hernias into the canal may occur medial (direct) or lateral (indirect) to the inferior epigastric vessels (see Figs. 2-3 and 2-7). Approached laparoscopically, three elevations of the peritoneum, referred to as the median, medial, and lateral umbilical folds, are visible on the anterior abdominal wall below the umbilicus (Fig. 2–8). The median fold overlies the median umbilical ligament (urachus), a fibrous remnant of the cloaca that attaches the bladder to the anterior abdominal wall. The obliterated umbilical artery in the medial umbilical fold serves as an important landmark for the surgeon. It may be traced to its origin from the internal iliac artery to locate the ureter, which lies on its medial side. During transperitoneal laparoscopic pelvic lymph node dissection, the obturator packet is accessed by incising the peritoneum lateral to the obliterated umbilical artery. In addition, during the performance of transperitoneal laparoscopic or robotic radical prostatectomy, the medial umbilical folds are used as landmarks to guide the dissection of the bladder to expose the space of Retzius. The lateral umbilical fold contains the inferior epigastric vessels as they ascend to supply the rectus abdominis. Figure 2–8 Male pelvis and anterior abdominal wall viewed from behind. The sacrum and ilia have been removed. (From Anderson JE. Grant’s atlas of anatomy. 7th ed. Baltimore: Williams & Wilkins; 1978. Fig. 3–41.) Muscles and fascia line the true pelvis and form its floor. The obturator internus arises from the inner surface of the obturator foramen and the obturator membrane and passes through the lesser sciatic foramen to insert on the femur (see Fig. 2–8). The fascia on the pelvic surface of this muscle is thickened into a tough line extending from the lower half of the pubis to the ischial spine. This tendinous arc of the levator ani serves as the origin of the muscles of the pelvic diaphragm: pubococcygeus and iliococcygeus (Fig. 2–9). These muscles are not truly separable, and they form a diaphragm that closes the pelvic outlet. Anteriorly, a narrow U-shaped hiatus remains, through which the urethra and rectum exit in the male, and the urethra, vagina, and rectum exit in the female (Fig. 2–10). The muscle bordering this hiatus has been referred to as pubovisceral because it provides a sling for (pubourethralis, puborectalis), inserts directly into (pubovaginalis, puboanalis, levator prostatae), or inserts into a structure intimately associated with the pelvic viscera (Lawson, 1974). The pubovisceral group provides strong fixation and support for the pelvic viscera. The coccygeus muscle extends from the sacrospinous ligament to the lateral border of the sacrum and coccyx to complete the pelvic diaphragm. Muscles of the pelvic diaphragm contain type I (slow-twitch) fibers, which provide tonic support to pelvic structures, and type II (fast-twitch) fibers, for sudden increases in intra-abdominal pressure (Gosling et al, 1981).The piriformis muscle arises from the lateral aspect of the sacrum and passes through and fills the greater sciatic foramen to form the posterolateral wall of the pelvis. (From Brooks JD, Chao W-M, Kerr J. Male pelvic anatomy reconstructed from the visible human data set. J Urol 1998;159:868–72.) It is important to recognize that the pelvic diaphragm is not flat or bowl shaped, as it is frequently depicted. At the urogenital and anal hiatus, the muscles lie in a near-vertical configuration and are thickened inferiorly (see Fig. 2–10) (Brooks et al, 1998; Myers et al, 1998). Behind the anus, they flatten to form a nearly horizontal diaphragm, referred to as the levator plate. In the female, the levator plate provides critical support to the pelvic viscera, as discussed later. The pelvic fasciae are not merely collagenous; they are also rich in elastic tissue and smooth muscle. This suggests that they are active in the support, and possibly the function, of the pelvic viscera. The pelvic fasciae are continuous with the retroperitoneal fasciae and have been categorized somewhat arbitrarily into outer, intermediate, and inner strata. The outer stratum, or endopelvic fascia, lines the inner surface of the pelvic muscles and is continuous with the transversalis layer of the abdomen. It is fixed to the arcuate line of the pelvis, Cooper ligament, the sacrospinous ligament, the ischial spine, and tendinous arc of the levator ani. The intermediate stratum embeds the pelvic viscera in a fatty, compressible layer that accommodates their filling and emptying. Its tissues are easily swept aside to reveal the retropubic, paravesical, rectogenital, and retrorectal potential spaces. All pelvic vessels and some pelvic nerves travel in this stratum and are subject to injury when these potential spaces are developed at surgery. The intermediate stratum coalesces around vessels and nerves supplying the pelvic organs to form named ligaments (e.g., cardinal, uterosacral, lateral, and posterior vesical) that suspend and tether these organs in the pelvis. This fascia also thickens around the pelvic urogenital organs to form their visceral fascia. These are not true ligaments but rather a meshwork of connective tissue and smooth muscle investing the visceral neurovascular pedicles (DeCaro et al, 1998). The inner stratum lies just beneath the peritoneum and is associated with the entire gastrointestinal tract. In the pelvis, it covers the rectum and dome of the bladder and forms the rectogenital septum (Denonvilliers fascia). This septum is the developmental remains of the rectogenital pouch of peritoneum that extended between the rectum and internal genitalia to the pelvic floor. The pelvic fasciae have been given a confusing array of appellations by anatomists and surgeons interested in female pelvic organ prolapse. To add to the confusion, the strength of pelvic fasciae can differ significantly between individuals and races and these differences may predispose some individuals to pelvic prolapse (Zacharin, 1985). The pelvic fasciae have three important components: (1) Anteriorly, the puboprostatic ligaments attach to the lower fifth of the pubis, lateral to the symphysis and to the junction of the prostate and external sphincter. They are called the pubourethral ligaments in the female and insert on the proximal third of the urethra (Fig. 2–11 on the Expert Consult website (From DeLancey JOL. Structural support of the urethra as it relates to stress urinary continence: the hammock hypothesis. Am J Obstet Gynecol 1994;170:1719.) (From Mostwin JL. Current concepts of female pelvic anatomy and physiology. Urol Clin North Am 1991;18:178.) The weakest point in the pelvic floor, the urogenital hiatus, is bridged by the urogenital diaphragm, a structure unique to humans (see Fig. 2–10). The fibrous perineal membrane lies at the center of, and defines, the urogenital diaphragm (see Figs. 2-4, 2-10, and 2-14). It is triangular and spans the inferior ischiopubic rami from the pubis to the ischial tuberosities. Posteriorly, it ends abruptly; the superficial and deep transverse perinei run along its free edge (Fig. 2–15). The external genitalia attach to its inferior surface; superiorly, it supports the urethral sphincter (discussed later). The perineal body represents the point of fusion between the free posterior edge of the urogenital diaphragm and the posterior apex of the urogenital hiatus. This pyramid-shaped structure forms the hub of pelvic support. Virtually every pelvic muscle (superficial and deep transverse perinei, bulbocavernosus, levator ani, rectourethralis, external anal sphincter, striated urethral sphincter) and fascia (perineal membrane, Denonvilliers, Colles, and endopelvic) insert into the perineal body. At its core are abundant elastin and richly innervated smooth muscle, which suggests that it may have a dynamic role in support. Damage to the perineal body during perineal prostatectomy risks postoperative urinary incontinence. (From Brooks JD, Chao W-M, Kerr J. Male pelvic anatomy reconstructed from the visible human data set. J Urol 1998;159:871.) Figure 2–15 Muscles of the male perineum. The transversus perinei and ischiocavernosi frame the urogenital diaphragm. (From Williams PL, Warwick R. Gray’s anatomy. 35th British ed. Philadelphia: WB Saunders; 1973. p. 530.) Major arteries of the pelvis are summarized in Table 2–1. At the bifurcation of the aorta, the middle sacral artery arises posteriorly and travels on the pelvic surface of the sacrum to supply branches to the sacral foramina and the rectum. The common iliac arteries arise at the level of the fourth lumbar vertebra, run anterior and lateral to their accompanying veins, and bifurcate into the external and internal iliac arteries at the SI joint (Fig. 2–16). The external iliac artery follows the medial border of the iliopsoas muscle along the arcuate line and leaves the pelvis beneath the inguinal ligament as the femoral artery (Fig. 2–17). Its inferior epigastric artery is given off proximal to the inguinal ligament and ascends medial to the internal inguinal ring to supply the rectus muscle and overlying skin. Because the rectus is richly collateralized from above and laterally, the inferior epigastric arteries may be ligated with impunity. A rectus myocutaneous flap based on this artery has been used to correct major pelvic and perineal tissue defects. Near its origin, the inferior epigastric artery sends a deep circumflex iliac branch laterally and a pubic branch medially. Both vessels travel on the iliopubic tract and may be injured during inguinal hernia repair. Its cremasteric branch joins the spermatic cord at the internal inguinal ring and forms a distal anastomosis with the testicular artery (Fig. 2–18). In 25% of people, an accessory obturator artery arises from the inferior epigastric artery and runs medial to the femoral vein to reach the obturator canal. This vessel must be avoided during obturator lymph node dissection. Table 2–1 Arteries of the Pelvis Figure 2–16 Right internal and external iliac arteries. The ureter and vas deferens pass medial to the vessels. (From Clemente CD. Gray’s anatomy. 30th American ed. Philadelphia: Lea & Febiger; 1985. p. 750.) Figure 2–17 Right obturator fossa, showing the iliac vessels and obturator nerve. (From Skinner DG. Pelvic lymphadenectomy. In: Glenn JF, editor. Urological surgery. 2nd ed. New York: Harper & Row; 1975. p. 591.) Figure 2–18 Collateral arterial circulation to the testis. (From Hinman F Jr. Atlas of urosurgical anatomy. Philadelphia: WB Saunders; 1993. p. 497.) The internal iliac (hypogastric) artery descends in front of the SI joint and divides into an anterior and a posterior trunk (see Fig. 2–16). The posterior trunk gives rise to three parietal branches: (1) the superior gluteal, which exits the greater sciatic foramen; (2) the ascending lumbar, which supplies the posterior abdominal wall; and (3) the lateral sacral, which passes medially to join the middle sacral branches at the sciatic foramina. The anterior trunk gives off seven parietal and visceral branches: (1) The superior vesical artery arises from the proximal portion of the obliterated umbilical artery and gives off a vesiculodeferential branch to the seminal vesicles and vas deferens. The artery of the vas deferens travels the length of the vas to meet the cremasteric and testicular arteries distally (see Fig. 2–18). Because of these anastomoses, the testicular artery may be sacrificed without compromising the viability of the testis. (2) The middle rectal artery gives small branches to the seminal vesicles and prostate and anastomoses with the inferior and superior rectal arteries in the rectal wall. (3) The inferior vesical branches supply the lower ureter, the bladder base, the prostate, and the seminal vesicles. In the female, they supply the ureter, the bladder base, and the vagina. (4) The uterine artery passes above and in front of the ureter (“water flows under the bridge”) to ascend the lateral wall of the uterus and meet the ovarian artery in the lateral portion of the fallopian tube (see Figs. 2-13 and 2-19). The ureter is vulnerable during division of the uterine pedicles. (5) The internal pudendal artery leaves the pelvic cavity through the greater sciatic foramen, passes around the sacrospinous ligament, and enters the lesser sciatic foramen to gain access to the perineum. Its perineal course is discussed later. (6) The obturator artery, variable in origin, travels through the obturator fossa medial and inferior to the obturator nerve and passes through its canal to supply the adductors of the thigh (see Fig. 2–17). (7) The inferior gluteal artery travels through the greater sciatic foramen to supply the buttock and thigh. Figure 2–19 Female internal genitalia, from behind. The ureter passes beneath the uterine artery. (From Hinman F Jr. Atlas of urosurgical anatomy. Philadelphia: WB Saunders; 1993. p. 402.) The dorsal vein of the penis passes between the inferior pubic arch and the striated urinary sphincter to reach the pelvis, where it trifurcates into a central superficial branch and two lateral plexuses (Reiner and Walsh, 1979) (Fig. 2–20). To minimize blood loss at radical retropubic prostatectomy, the dorsal vein complex is best divided distally, before its ramification. Part of this complex runs within the anterior and lateral wall of the striated sphincter; thus care must be taken not to injure the sphincter when securing hemostasis. The superficial branch pierces the visceral endopelvic fascia between the puboprostatic ligaments and drains the retropubic fat, anterior bladder, and anterior prostate (see Fig. 2–20). (From Reiner WG, Walsh PC. An anatomical approach to the surgical management of the dorsal vein and Santorini’s plexus during radical retropubic surgery. J Urol 1979;121:200.) The internal iliac vein is joined by tributaries corresponding to the branches of the internal iliac artery and ascends medial and posterior to the artery. This vein is relatively thin walled and at risk for injury during dissection of the artery or the nearby pelvic ureter. The external iliac vein travels medial and inferior to its artery and joins the internal iliac vein behind the internal iliac artery. In half the patients, one or more accessory obturator veins drain into the underside of the external iliac vein and can be easily torn during lymphadenectomy (see Fig. 2–17). The pelvic lymph nodes can be difficult to appreciate on gross examination because they are embedded in the fatty and fibrous tissue of the intermediate stratum. Three major lymph node groups are associated with the pelvic vessels (Fig. 2–21). A substantial portion of pelvic visceral lymphatic drainage passes through the internal iliac nodes and their tributaries: the presacral, obturator, and internal pudendal nodes. The external iliac nodes lie lateral, anterior, and medial to the vessels and drain the anterior abdominal wall, urachus, bladder, and, in part, internal genitalia. The external genitalia and perineum drain into the superficial and deep inguinal nodes (see later discussion). The inguinal nodes communicate directly with the internal and external iliac chains. The common iliac nodes receive efferent vessels from the external and internal iliac nodes and the pelvic ureter and drain into the lateral aortic nodes. The lumbosacral plexus and its rami are well illustrated in Chapter 1; only the pelvic courses of its nerves are reviewed here (see Figs. 2-7 and 2-12 and Table 2–2). The iliohypogastric nerve (L1) travels between, and supplies, the internal oblique and the transversus muscles and pierces the internal and external oblique muscles 3 cm above the external inguinal ring to supply sensation over the lower anterior abdomen and pubis (see Fig. 2–5). The ilioinguinal nerve (L1) passes through the internal oblique muscle to enter the inguinal canal laterally. It travels anterior to the cord and exits the external ring to provide sensation to the mons pubis and anterior scrotum or labia majora (see Figs. 2-5 and 2-7). The genitofemoral nerve (L1, L2) pierces the psoas muscle to reach its anterior surface in the retroperitoneum and then travels to the pelvis and splits into genital and femoral branches. The latter supplies sensation over the anterior thigh below the inguinal ligament. The genital branch follows the cord through the inguinal canal, supplies the cremaster muscle, and supplies sensation to the anterior scrotum. Table 2–2 Somatic Nerves of the Lower Abdomen and Pelvis For most of its pelvic course, the femoral nerve (L2, L3, L4) travels within the substance of the psoas muscle and then exits its lateral side to pass under the inguinal ligament (Fig. 2–22). It supplies sensation to the anterior thigh and motor innervation to the extensors of the knee. During a psoas hitch, sutures should be placed in the direction of the nerve (and the psoas muscle fibers) to avoid nerve damage or entrapment. Retractor blades must not rest on the psoas muscle because they can produce a femoral nerve palsy, a potentially dangerous setback after pelvic surgery. The lateral femoral cutaneous nerve (L2, L3) may be seen lateral to the psoas in the iliacus fascia. (From Burnett AL, Brendler CB. Female neuropathy following major pelvic surgery: etiology and prevention. J Urol 1994;151:163.) The lumbosacral trunk (L4, L5) passes into the true pelvis behind the psoas and unites with the ventral rami of the sacral segmental nerves to form the sacral plexus. This plexus lies on the pelvic surface of the piriformis deep to the endopelvic fascia and posterior to the internal iliac vessels (see Fig. 2–16). It leaves the pelvis through the greater sciatic foramen immediately posterior to the sacrospinous ligament (where it may be injured during sacrospinous culposuspension) and supplies motor and sensory innervation to the posterior thigh and lower leg. An exaggerated lithotomy position may stretch this nerve or place pressure on its peroneal branch at the fibular head to produce foot drop. Pelvic and perineal branches of the sacral plexus include (1) the posterior femoral cutaneous nerve (S2, S3), which, after passing through the greater sciatic foramen, gives an anterior sensory branch to the perineum and posterior scrotum (see Fig. 2–8); (2) the pudendal nerve (S2, S3, S4), which follows the internal pudendal artery to the perineum (to be discussed); (3) the nervi erigentes (S2, S3, S4) to the autonomic plexus; and (4) pelvic somatic efferent nerves from the ventral rami of S2, S3, and S4 (Fig. 2–23). The latter nerves travel on the pelvic surface of the levator ani in close association with the rectum and prostate and are separated from the pelvic autonomic plexus by the endopelvic fascia. They supply the levator ani and extend anteriorly to the striated urethral sphincter (Lawson, 1974; Zvara et al, 1994). (From Lawson JO. Pelvic anatomy. I. Pelvic floor muscles. Ann R Coll Surg Engl 1974;54:250.) The presynaptic sympathetic cell bodies that project to the pelvic autonomic plexus reside in the lateral column of gray matter in the last three thoracic and first two lumbar segments of the spinal cord. They reach the pelvic plexus by two pathways: (1) The superior hypogastric plexus is formed by sympathetic fibers from the celiac plexus and the first four lumbar splanchnic nerves (Fig. 2–24). Anterior to the bifurcation of the aorta, it divides into two hypogastric nerves that enter the pelvis medial to the internal iliac vessels, anterior to the sacrum, and deep to the endopelvic fascia. (2) The pelvic continuations of the sympathetic trunks pass deep to the common iliac vessels and medial to the sacral foramina and fuse in front of the coccyx at the ganglion impar (see Fig. 2–24). Each chain comprises four to five ganglia that send branches anterolaterally to participate in the formation of the pelvic plexus. Presynaptic parasympathetic innervation arises from the intermediolateral cell column of the sacral cord. Fibers emerge from the second, third, and fourth sacral spinal nerves as the pelvic splanchnic nerves (nervi erigentes) to join the hypogastric nerves and branches from the sacral sympathetic ganglia to form the inferior hypogastric (pelvic) plexus (see Fig. 2–24). Some pelvic parasympathetic efferent fibers travel up the hypogastric nerves to the inferior mesenteric plexus, where they provide parasympathetic innervation to the descending and sigmoid colon. The pelvic plexus is rectangular, approximately 4 to 5 cm long, and its midpoint is at the tips of the seminal vesicles (Schlegel and Walsh, 1987). It is oriented in the sagittal plane on either side of the rectum and pierced by the numerous vessels going to and from the rectum, bladder, seminal vesicles, and prostate (Fig. 2–25). Division of these vessels (the so-called lateral pedicles of the bladder and prostate) risks injury to the pelvic plexus with attendant postoperative impotence (Walsh and Donker, 1982; Walsh et al, 1983). The right and left components of the pelvic plexus communicate behind the rectum and anterior and posterior to the vesical neck. Branches of the pelvic plexus follow pelvic blood vessels to reach the pelvic viscera, although nerves to the ureter may join it directly as it passes nearby. Visceral afferent and efferent nerves travel on the vas deferens to reach the testis and epididymis (see later discussion). Figure 2–25 Lateral view showing the left pelvic autonomic nervous plexus and its relation to the pelvic viscera. (From Schlegel PN, Walsh PC. Neuroanatomical approach to radical cystoprostatectomy with preservation of sexual function. J Urol 1987;138:1403.) The most caudal portion of the pelvic plexus gives rise to the innervation of the prostate and the important cavernosal nerves (Walsh and Donker, 1982). After passing the tips of the seminal vesicles, these nerves lie within leaves of the lateral endopelvic fascia near its juncture with, but outside, Denonvilliers fascia (Lepor et al, 1985). They travel at the posterolateral border of the prostate on the surface of the rectum and are lateral to the prostatic capsular arteries and veins (see Fig. 2–25). Because the nerves are composed of multiple fibers not visible on gross inspection, these vessels serve as a surgical landmark for the course of these nerves (the neurovascular bundle of Walsh). During radical prostatectomy, the nerves are most vulnerable at the apex of the prostate, where they closely approach the prostatic capsule at the 5- and 7-o’clock positions. On reaching the membranous urethra, the nerves divide into superficial branches, which travel on the lateral surface of the striated urethral sphincter at 3- and 9-o’clock positions, and deep fibers, which penetrate the substance of this muscle and send twigs to the bulbourethral glands. As the nerves reach the hilum of the penis, they join to form one to three discrete bundles, related to the urethra at 1- and 11-o’clock positions, superficial to the cavernous veins and dorsomedial to the cavernous arteries (Fig. 2–26) (Lue et al, 1984; Breza et al, 1989). With the arteries, they pierce the corpora cavernosa to supply the erectile tissue (see later discussion). Small fibers also join the dorsal nerves of the penis as they course distally. In the female, the nerves to vestibular bodies and corpora cavernosa of the clitoris travel between the anterior vaginal wall and the bladder in association with the lateral venous plexuses. Figure 2–26 Dorsal penile arteries, veins, and nerves. (From Hinman F Jr. Atlas of urosurgical anatomy. Philadelphia: WB Saunders: 1993. p. 445.)
Bony Pelvis
Anterior Abdominal Wall
Skin and Subcutaneous Fasciae
Abdominal Musculature
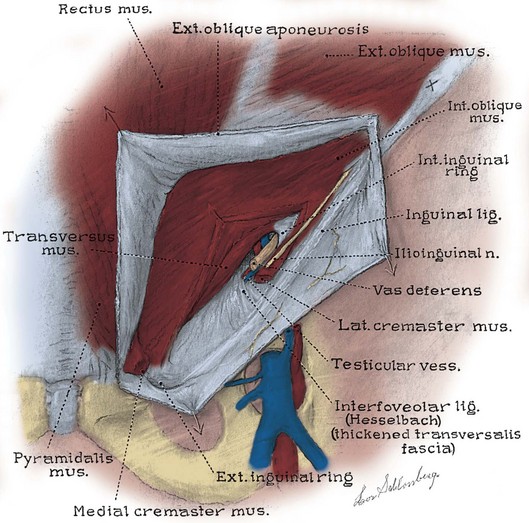
Inguinal Canal
Internal Surface of the Anterior Abdominal Wall
Soft Tissues of the Pelvis
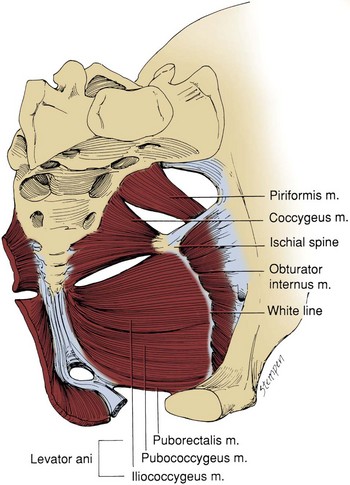
Pelvic Musculature
Pelvic Fasciae
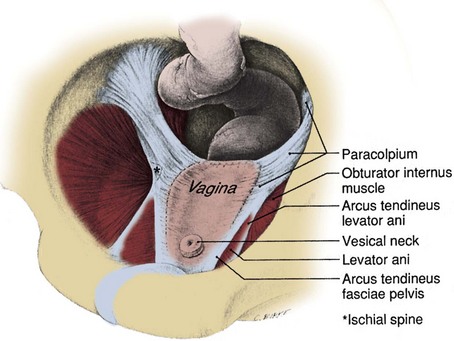
![]() ). (2) Laterally, the arcus tendineus fascia pelvis extends from the puboprostatic (pubourethral) ligament to the ischial spine (see Fig. 2–11). This fascia forms at the junction of the endopelvic and visceral fasciae. It should not be confused with the arcus tendineus levator ani, which lies above its anterior portion (Fig. 2–12). In the male, the arcus tendineus fascia pelvis is found at the base of a sulcus between the pelvic side wall and the prostate and bladder. In the female, it corresponds to the lateral attachment of the anterior bladder wall to the pelvic side wall. Paravaginal suspension procedures for stress urinary incontinence entail lateral reapproximation of the vaginal wall to this tendinous arc (Richardson et al, 1981). The lateral branches of the dorsal venous complex are directly beneath the arcus tendineus fascia pelvis; thus the endopelvic fascia should be opened lateral to this landmark. In the female, the fascia extending medially from this arch carries a variety of names (pubovesical, periurethral, urethropelvic ligament) and provides important support to the urethra and anterior vaginal wall. Damage to this fascia and its attachments has been implicated in urethrocele, cystocele, and stress urinary incontinence. (3) Posterior to the ischial spine, the fascia fans out to either side of the rectum and attaches to the pelvic side wall as the lateral and posterior vesical ligaments. In the female, these are the strong cardinal and uterosacral ligaments. They are not true ligaments; rather, they are condensations of intermediate stratum around visceral neurovascular pedicles. The peritoneum over these ligaments forms discrete folds (rectovesical in the male and rectouterine in the female) that can be appreciated at cystectomy (Fig. 2–13). Taken as a whole, the pelvic fasciae form a Y-shaped scaffolding for the pelvic viscera (see Fig. 2–12).
). (2) Laterally, the arcus tendineus fascia pelvis extends from the puboprostatic (pubourethral) ligament to the ischial spine (see Fig. 2–11). This fascia forms at the junction of the endopelvic and visceral fasciae. It should not be confused with the arcus tendineus levator ani, which lies above its anterior portion (Fig. 2–12). In the male, the arcus tendineus fascia pelvis is found at the base of a sulcus between the pelvic side wall and the prostate and bladder. In the female, it corresponds to the lateral attachment of the anterior bladder wall to the pelvic side wall. Paravaginal suspension procedures for stress urinary incontinence entail lateral reapproximation of the vaginal wall to this tendinous arc (Richardson et al, 1981). The lateral branches of the dorsal venous complex are directly beneath the arcus tendineus fascia pelvis; thus the endopelvic fascia should be opened lateral to this landmark. In the female, the fascia extending medially from this arch carries a variety of names (pubovesical, periurethral, urethropelvic ligament) and provides important support to the urethra and anterior vaginal wall. Damage to this fascia and its attachments has been implicated in urethrocele, cystocele, and stress urinary incontinence. (3) Posterior to the ischial spine, the fascia fans out to either side of the rectum and attaches to the pelvic side wall as the lateral and posterior vesical ligaments. In the female, these are the strong cardinal and uterosacral ligaments. They are not true ligaments; rather, they are condensations of intermediate stratum around visceral neurovascular pedicles. The peritoneum over these ligaments forms discrete folds (rectovesical in the male and rectouterine in the female) that can be appreciated at cystectomy (Fig. 2–13). Taken as a whole, the pelvic fasciae form a Y-shaped scaffolding for the pelvic viscera (see Fig. 2–12).
Fasciae of the Perineum and the Perineal Body
Pelvic Circulation
Arterial Supply
ARTERY NAME
ORIGIN
SUPPLIES
Middle sacral
Aorta
Sacral nerves and sacrum
External Iliac Branches
Inferior epigastric
External iliac
Rectus abdominis muscle and overlying skin and fascia
Deep circumflex iliac
Inferior epigastric
Inguinal ligament and surrounding structures laterally
Pubic
Inferior epigastric
Inguinal ligament and surrounding structures medially
Cremasteric
Inferior epigastric
Vas deferens and testis
Internal Iliac Branches
Superior gluteal
Posterior trunk
Gluteus muscles and overlying skin
Ascending lumbar
Posterior trunk
Psoas and quadratus lumborum muscles and adjacent structures
Lateral sacral
Posterior trunk
Sacral nerves and sacrum
Superior vesical
Anterior trunk
Bladder, ureter, vas deferens, and seminal vesicle
Middle rectal
Anterior trunk
Rectum, ureter, and bladder
Inferior vesical
Anterior trunk
Bladder, seminal vesicle, prostate, ureter, and the neurovascular bundle
Uterine
Anterior trunk
Uterus, bladder, and ureter
Internal pudendal
Anterior trunk
Rectum, perineum, and external genitalia
Obturator
Anterior trunk
Adductor muscles of the leg and overlying skin
Inferior gluteal
Anterior trunk
Gluteus muscles and overlying skin
Venous Supply
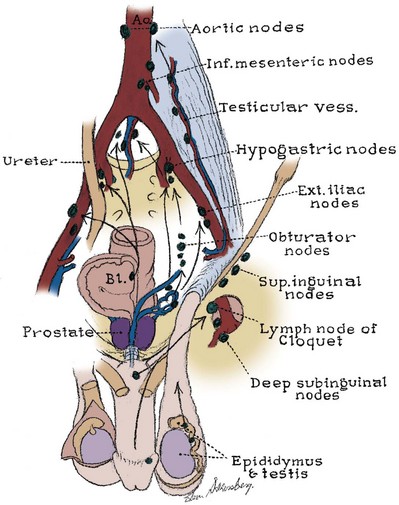
Pelvic Lymphatics
Pelvic Innervation
Lumbosacral Plexus
NERVE NAME
ORIGIN
SUPPLIES
Iliohypogastric
L1
Motor supply to internal oblique, transversus muscles, sensation over lower anterior abdominal wall
Ilioinguinal
L1
Sensation over anterior pubis (mons) and anterior scrotum or labia
Genitofemoral
L1, L2
Genital branch: motor supply to cremaster muscle sensation to anterior scrotum
Femoral branch: sensation to anterior thigh
Femoral
L2, L3, L4
Motor supply to extensors of the knee sensory to anterior thigh
Obturator
L2, L3, L4
Motor supply to adductors of the thigh, sensation to medial thigh
Lumbosacral trunk
L4, L5
Joins the sacral nerves to form the lumbosacral plexus that supplies motor and sensory innervation to the lower extremities
Posterior femoral cutaneous
S2, S3
Sensation to perineum, posterior scrotum, and posterior thigh
Pudendal
S2, S3, S4
Motor to levator ani, muscles of the urogenital diaphragm, anal and striated urethral sphincter, sensation to the perineum, scrotum, penis
Pelvic somatic efferents
S2, S3, S4
Motor supply to levator ani and striated urethral sphincter
Nervi erigentes
S2, S3, S4
Parasympathetic fibers from the sacral cord supply the pelvic viscera
Pelvic Autonomic Plexus
Anatomy of the Lower Urinary Tract and Male Genitalia