Chapter 44 TRANSOBTURATOR APPROACH TO MIDURETHRAL SLING
Surgery for stress urinary incontinence has changed rapidly in the past decade. This change was preceded and to some extent catalyzed by critical appraisal of anti-incontinence surgery as an empirical therapy that, at best, provides a compensatory abnormality to restore continence. Implicit in this view is the acceptance that surgery has the potential to upset the balance of neurologic and anatomic factors that govern the bladder and its outlet. The rationale for recent innovation has been to limit the detrimental effect on this balance that can result from surgical therapy.
It is appropriate to attribute much of the recent improvement in surgical therapy of incontinence to the work of Ulf Ulmsten. Ulmsten’s original thinking and his insistence on scrutinizing the concepts that he formulated with rigorous scientific methodology are laudable, and his work represents a milestone in the evolution of surgical practice.1–3 His tension-free vaginal tape (TVT) procedure has become the “gold standard” for antiincontinence surgery. Improvement in technique will need to incorporate its innovative features.
The improvement offered by the transobturator sling (TOT) over other midurethral slings is a reduction in the incidence of penetration injuries during sling introduction. Although complications associated with the TVT procedure are uncommon, stress incontinence is an exceedingly common condition. Now, with experience with TVT totaling hundreds of thousands of women, it has become apparent that serious complications can result from the procedure and from the other retropubic sling procedures that copy it. Injury to the colon, small bowel, ureter, urethra, bladder vasculature, tube, and ovary have been associated with the procedure, as have erosions of the sling material into the vagina, bladder, and urethra.4–6 Bleeding, hematoma, abscess formation, retention, and voiding dysfunction can occur. The most feared of these complications is bowel perforation. If this occurs during blind sling introduction, its recognition is not immediate, yet it is potentially fatal, especially if diagnosis is delayed. The extent to which this particular complication is related to human error is probably irrelevant. The fact is that TVT is a blind procedure, with needle passage occurring in proximity to the bowel. Bowel perforation is to some extent related to the technique involved in retropubic midurethral sling placement, and even experienced surgeons can encounter it.
DESCRIPTION
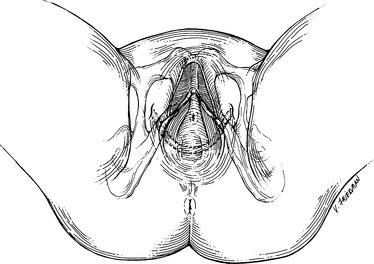
In the continuing effort to evaluate and improve surgical therapy for incontinence, the TOT approach has recently reached mainstream clinical practice.7 It is a type of midurethral sling that incorporates midurethral placement, the use of local anesthesia, and a cough stress test (Fig. 44-1). No technique is without surgical risk, but TOT seems to offer less risk than retropubic midurethral sling procedures do. TOT logically avoids the potential for bowel or large vessel injury, because it avoids blind retro-pubic needle passage.
In most respects, the TOT and retropubic TVT procedures are identical. Both use an identical hammock-like strip of polypropylene placed beneath the mid-urethra to support it from above. The main difference is in technique: with TOT placement, the introducer needle remains superficial to the urogenital diaphragm. Because the introducer needle is not allowed to pass through the retropubic space, the risk that the needle tip could cause injury to bladder, bowel, or blood vessels is lessened. The TOT sling and its instruments have been approved by the U.S. Food and Drug Administration for the treatment of stress urinary incontinence in females. This chapter discusses anatomy pertinent to TOT route, the technique itself, and the published literature supporting its use.
ANATOMY
The fact that the obturator foramen is unfamiliar to most urologists has to do with its lack of urologic surgical applications and not with any inherent danger of dissection in the area. Most urologists consider this part of the pelvis to be an end point, not a gateway, and are unfamiliar with its anatomy. The obturator foramen is not without common surgical applications, however. Access to the obturator vessels through the obturator foramen for vascular bypass, for instance, is a classic approach for relief of vascular insufficiency in the lower extremity.8 Veterinary surgeons predate urologists in the treatment of stress in-continence in female dogs via this approach.9 The advantages of TOT sling placement now makes a complete understanding of the anatomy of the obturator foramen relevant to the urologist as well.
The obturator foramen is an oval opening in the anterior ventral bony pelvis formed by the confluence of the pubic and ischial bones. The obturator membrane is a thin fibrous sheet which almost completely closes the obturator foramen. Its fibers are arranged in interlacing bundles, mainly transverse in direction; the uppermost bundle is attached to the obturator tubercles and completes the obturator canal for passage of the obturator vessels and nerve in its lateral aspect. Both obturator muscles are continuous with this membrane: the obturator internus padding the inner aspect and the obturator externus its outer surface.10
The obturator nerve arises from the ventral divisions of the second, third, and fourth lumbar nerves. It descends through the fibers of the psoas major and emerges from its medial border. It runs along the lateral wall of the pelvis above and in front of the obturator vessels to the upper lateral part of the obturator foramen. Here it enters the thigh to innervate the muscles of adduction. The obturator artery and vein that supply and drain the muscles of the medial thigh course together with the nerve through the foramen laterally. The anatomic location of the nerve and vessels in the upper outer part of the obturator foramen allows for safe passage of introduced trocars along the medial aspect of the foramen.11
The obturator foramen, its membrane, the obturator internus muscle, and its surrounding fascia lie external to the endopelvic fascial lining of the pelvis and the peritoneal cavity. Normal passage of the introducing needle during the TOT sling procedure avoids both spaces. Anatomic studies in cadavers have demonstrated that, when properly positioned, the TOT sling travels in a horizontal plane across the origin of the adductor muscles and through the inferior margin of the obturator foramen. The sling then passes through the internal obturator muscle, above the pedicle of the internal pudendal artery, through the levator ani muscle, past the tendinous arc of the pelvic fascia, and beneath the middle third of the urethra.12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree