Fig. 27.1
Operative positioning for TAMIS. (a) The patient is placed in high lithotomy position for posterior lesions. (b) The patient is placed in prone-jackknife position on a split-leg table for anterior lesions
For lateral lesions, the patient is positioned either in prone-jackknife or lithotomy and turned in either direction such that the lesion is as close to the 6 o’clock position as possible. If the lesion cannot be placed directly at the midline, it is preferentially oriented toward the surgeon’s dominant hand to facilitate suture repair. The patient must be firmly secured to the table, which we accomplish with towels and circumferential tape at the level of the chest.
Port Placement and Exposure
The anal sphincter is manually dilated with 2–3 fingers. We no longer perform intersphincteric injections of any kind. The transanal access channel/port is heavily lubricated and inserted into the anal canal with the lip of the port placed proximal to the sphincters and levator. If the lip of the port does not completely traverse the levators, visualization will invariably be obstructed by internal hemorrhoidal tissue. Insertion of the port can be facilitated by internally folding and grasping the port with a ring clamp. After initial insertion, gentle pressure can be applied with the introducer supplied by the manufacturer to push the lip of the port past the levators. There is no need to suture the port to the skin, given that it is fairly stable if placed in the appropriate position (Fig. 27.2).
Fig. 27.2
Diagram illustrating proper seating of the transanal port in the anal canal. The body of the port is approximately 4 cm wide and is properly inserted at 5.5 cm
A lightly moistened sponge is inserted into the rectum, to be pushed into the proximal lumen during insufflation. This helps prevent insufflation of the proximal colon and may also limit periodic collapse of the pneumorectum during the case. The instrument sleeves are then placed into the gel cap and the gel cap is then fixed to the transanal port.
Identification of Excision Margins of at Least 1 cm
We routinely mark 1-cm margins using a hook cautery device. As the dissection proceeds, tissue distortion and retraction are encountered and these cautery marks are invaluable in preventing disorientation and assuring adequate margins of excision (Fig. 27.3).
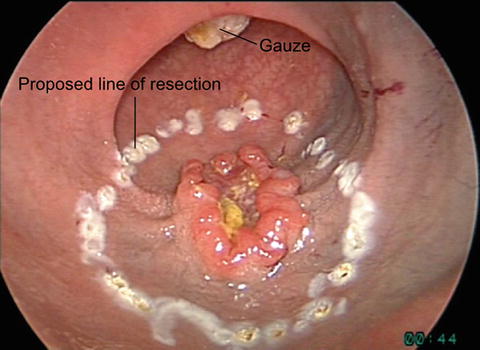
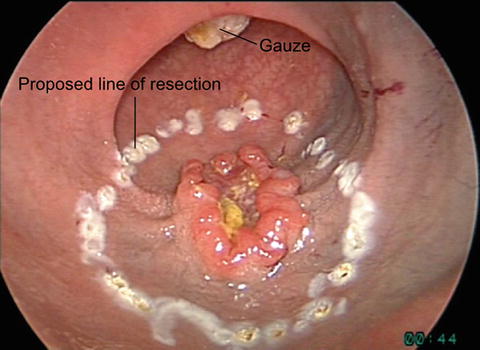
Fig. 27.3
Marking 1-cm margin of excision of rectal lesion marked with hook cautery
Full-Thickness Incision of the Rectal Wall
A full-thickness incision is made into the perirectal tissue beginning 1 cm distal to the lesion. This is usually accomplished by lifting the rectal wall with a grasper and incising the rectum with a hook cautery device. Distal incision allows complete visualization of the tissue planes during the course of the dissection (Fig. 27.4).
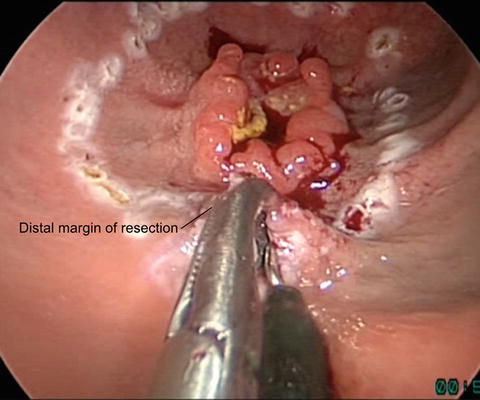
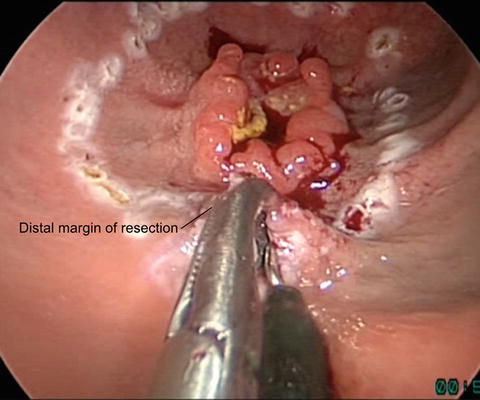
Fig. 27.4
Excision of rectal lesion begins with full-thickness incision of the rectal wall at the distal margin
Posteriorly, the perirectal tissue is usually easily recognized by the presence of perirectal fat. While there is often some fat anteriorly as well, the correct plane generally consists of loose, relatively avascular areolar tissue between the rectal wall and the urogenital structures. This initial step should be performed with extreme caution for anterior and lateral excisions to avoid injury to major vascular and urogenital structures.
We do not perform partial-thickness excisions given that this alternative is not oncologically appropriate in the setting of a suspected cancer, and because (in our experience) benign adenomas are almost always appropriately treated with endoscopic mucosal resection by our gastroenterology colleagues.
Circumferential Dissection
The perirectal tissue is dissected first by bluntly spreading the tissue in the appropriate plane and by taking the perirectal tissue sharply with cautery. The overlying rectal wall is then taken progressively with cautery or ultrasonic shears. Dissection in this manner is especially important as the peritoneal reflection is approached and minimizes the risk of injury to perirectal structures (Fig. 27.5). The dissection is carried circumferentially in this manner on both sides. The proximal extent of the dissection is approached in the deep plane first, with the overlying rectal wall and mucosa taken with energy immediately thereafter.
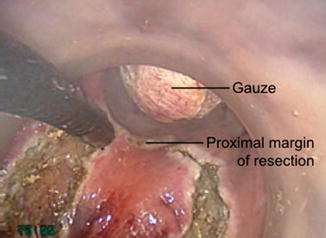
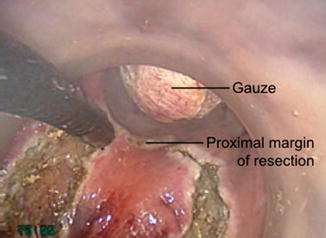
Fig. 27.5
Intraoperative photo demonstrates circumferential dissection of the lesion with 1-cm margin. A Ray-tec sponge has been inserted in the proximal rectum to limit insufflations of the colon and preserve the pneumorectum
Once free, the specimen is securely grasped to maintain orientation, and removed after unclamping the gelcap of the transanal port. The specimen is then placed on a Telfa dressing and oriented for pathologic examination. The surgeon routinely accompanies the specimen to the pathology room to assure orientation. Gross examination is routinely performed. Frozen section analysis is performed selectively if margin involvement is suspected.
Suture Repair
The pneumorectum often causes the excision defect to appear impressively large in size. This effect can be reduced by decreasing insufflation pressure in order to facilitate repair, though we generally find this unnecessary. We repair the defect using a multifilament absorbable suture with a LapraTy (Ethicon) on one end to avoid tying in a confined space (Fig. 27.6). Locking monofilament absorbable suture is now commercially available and is also a good option.
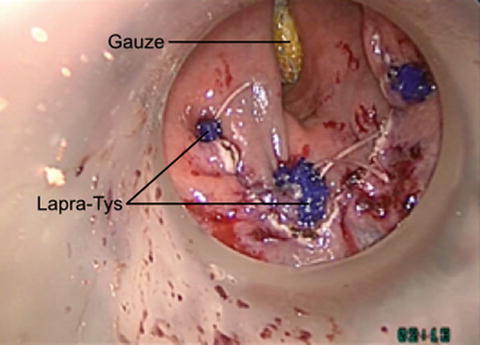
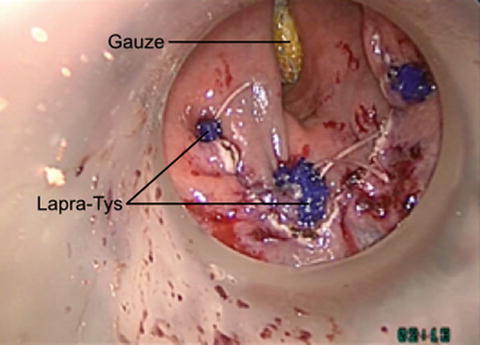
Fig. 27.6
Intraoperative photo demonstrates suture repair of the resulting rectal defect with running multifilament suture. LapraTys (Ethicon) have been placed to secure the sutures in place of knot-tying
The repair proceeds in a running fashion with large full-thickness bites from the side of the surgeon’s dominant hand towards the nondominant side. Depending on the size of the defect, 2 or 3 separate running sutures may be use to traverse the entire defect. This limits the amount of redundant suture that is in the lumen at any given time. Once the last bite is taken, a LapraTy (Ethicon) is placed and the suture divided to complete the repair. The gauze and transanal port are then gently removed.
Postoperative Care
The patient is admitted overnight for observation and diet is advanced as tolerated. Analgesics are usually unnecessary. In the absence of significant pain, fever, bleeding, or urinary retention the patient is discharged home on postoperative day #1. If fevers are noted, pelvic and abdominal sepsis should be ruled out. In the presence of a benign abdominal exam, empiric antibiotics may be used and the patient may be observed until resolution.
If fevers persist, imaging studies such as abdominal plain-films and/or CT scan of the abdomen and pelvis with rectal contrast should be considered. Free abdominal air should immediately raise concern for unrecognized peritoneal entry and should prompt laparoscopy and/or laparotomy in the setting of persistent abdominal pain and/or fevers.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








