Fig. 9.1
Patient positioning and OR setup. The operating surgeon stands between patient’s legs. The surgeon stands on patient’s right side for left colon procedure and then moves to left side for right colon procedure
Hand-Access Device Placement
A 7–8 cm minilaparotomy is made. We exclusively use muscle-splitting Pfannenstiel incision for UC cases, though we prefer a lower midline incision for Crohn’s patients to keep the lateral abdomen free of incisions for possible future ostomy [1, 2]. Too small of a wound may complicate free and deep insertion of the device, therefore, interfering with the HALS procedure. After confirming the adequacy of wound size by inserting surgeon’s hand into the abdomen, a hand-access device is assembled to the wound. Our favorite device is GelPort laparoscopic system (Applied Medical, Rancho Santa Margarita, CA), which provides stable wound retraction during open procedure and enables unlimited hand exchanges into every abdominal quadrant without significant gas leakage during laparoscopic procedure [5, 6].
Surgical Ports and Energy Devices
Two standard trocars are used: one in the periumbilical region for laparoscopy and the other in the left mid-abdomen for the energy device, respectively (Fig. 9.2). We currently prefer bipolar vessel-sealing device (LigaSure™, Covidien, Mansfield, MA) for colonic mobilization, takedown of the omentum, and mesenteric division. We do not find that the LigaSure™ device gets too hot, even after repeated activations, and thus enables safe use of surgeon’s hand simultaneously [6]. We do not use monopolar electrocautery or ultrasonically driven scalpel since these devices may make hand assist difficult with an inability to take large vessels (monopolar) and increased heat production. We also do not routinely use any laparoscopic clips. However, device and instrumentation selection is up to the individual surgeon, and preferences differ pending experience and comfort level.
Fig. 9.2
The sites for hand-access device, laparoscope, and energy device
The “Palm-Down” and “Palm-Up” Techniques
HALS requires logical and systemic use of surgeon’s hand. A random use of hand may interfere with the procedure, rather than assist the procedure. The authors have systematized and categorized the use of hand into two simple techniques: “palm-down” and “palm-up” techniques.
Most of HALS procedures can be performed using “palm-down” technique (Video 9.1). This technique facilitates free and delicate use of the 2nd/3rd fingers. This is best suited for extending an avascular plane under continuous traction, e.g., colonic mobilization (Fig. 9.3a). A blunt dissection using 2nd finger is possible, as needed.
Fig. 9.3
Schematic representations of (a) “palm-down” and (b) “palm-up” techniques
In “palm-up” position, on the contrary, the surgeon can more positively use his/her 1st finger (Video 9.2). This technique is effective for palpation and for dividing structures containing vessels. In mesenteric division, for example, a fine palpation and rapid division is possible by pinching the mesentery with 1st and 2nd fingers (Fig. 9.3b). Additionally, a wider displacement/retraction is possible with intentional use of dorsal surface of the hand. This is extremely useful in dividing the mesentery while keeping small-bowel loops out from the operative field.
Technical Aspects Step-by-Step
Our technical principles of TAC are similar either in open, straight laparoscopic or HALS approach, which involve entire colonic mobilization followed by the mesenteric division, both in an inferior-to-superior fashion initially, followed by counterclockwise approach. Since the high ligation of major colonic arteries is often unnecessary (except in the rare situation of multiple synchronous cancers), the authors exclusively use a “lateral-to-medial” approach for colonic mobilization. A “medial-to-lateral” approach can still be used; however, it is not as straightforward as in usual cancer cases due to inflamed mesentery and fragile peri-colonic tissue. The key is to maximally utilize the minilaparotomy to facilitate “open” procedures, i.e., procedures achievable under direct vision, such as small-bowel exploration, partial colonic mobilization, and anastomosis.
Step 1. Partial Colonic Mobilization Under Direct Vision (Fig. 9.4)
Fig. 9.4
Step 1 (partial colonic mobilization under direct vision)
The procedure begins under direct vision with the hand-access device left uncapped (opened). First, the small bowel is identified and exteriorized to evaluate any “extracolonic” pathologies. This step is extremely important in Crohn’s patients, since additional strictureplasty and/or small-bowel resection can be immediately performed under direct vision when a significant lesion is identified during the exploration. This exploration is also important in UC patients to exclude any possibility of “Crohn’s disease mimicking UC.”
While the hand-access device is kept uncapped, the descending colon and its junction to the sigmoid colon is exposed and partially mobilized (Fig. 9.5). The left ureter can be identified as it crosses over the iliac bifurcation in thin patients (Video 9.3). The dissection can be extended towards the splenic flexure as long as the exposure is adequate and constant. The ileocecal mobilization is then performed on the right side as well (Fig. 9.4). The key is to use long retracting devices for effective displacement of the small-bowel loops.
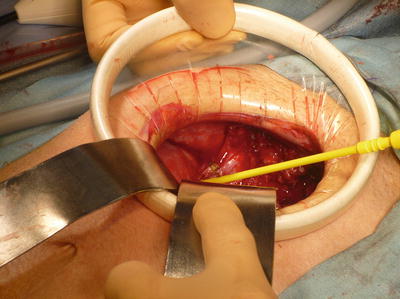
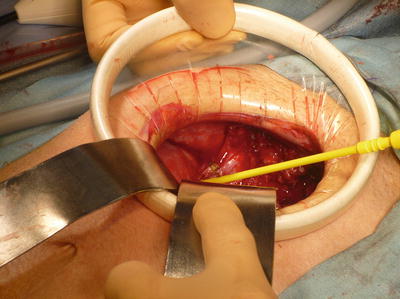
Fig. 9.5




Mobilizing the sigmoid-descending colon junction under direct vision
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








