The Shouldice Hospital Repair
Robert Bendavid
Introduction
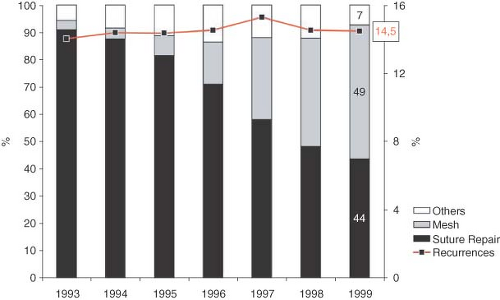
There is evidence that, despite advances in hernia surgery, the rate of hernia recurrence has remained the same, hovering at about 14% worldwide, with a range of 10% to 22% (Tables 7.1, 7.2 and Figure 7.1). By advances we mean the several varieties of prosthetic meshes, the numerous kinds of implantable, one size fits all gadgets which flood every surgical meeting, and the still controversial laparoscopic techniques. It may be that in the hands of surgeons sub-specializing in hernia surgery, the results are better but the overwhelming majority of hernias are repaired by general surgeons who, on average, do 50 cases a year only!. Statistics from the Shouldice Hospital point to the fact that 65% of the failed herniorrhaphies are due to an inadequate search for a hernia or simply due to a grossly inadequate knowledge of anatomy. Much to the regret of the surgical community, the Shouldice Hospital has not come forward, in the last 20 years, with meaningful peer reviewed publications or statistical data to support the claims which they put forth at conferences; nor have their statistics ever been presented with a seal of approval by a bona fide statistician. For those reasons, the comparative results must come from older series as well as from older reports, albeit from competent surgeons. It must also be kept in mind, in all fairness, that pure tissue repairs do not get the approval and support of an industry which is geared to produce and sell what it manufactures. We shall revisit these ethical issues.
History
The Shouldice Hospital was established in 1945 by Earle Shouldice. Its accomplishment is not in having designed a new operation. It did not. It simply carried out the steps of the Bassini operation faithfully. These steps were introduced by one of the staff surgeons, Ernie Ryan. Three differences stand out between the classic Bassini operation and what is done at the Shouldice Hospital today: The use of stainless steel wire as a suture material, as opposed to the cotton and silk which were available in Bassini’s days; a continuous suture rather than the interrupted sutures which Bassini inserted;
the exclusion of the periosteum from the first suture as was suggested by Bassini. The Shouldice Hospital, can be said to have been the heir of Bassini in having honored and respected each and every step of his legacy. The Hospital, still in existence today, performs upwards of 7,000 operations a year, which are carried out by a staff varying from 10 to 12 dedicated surgeons.
the exclusion of the periosteum from the first suture as was suggested by Bassini. The Shouldice Hospital, can be said to have been the heir of Bassini in having honored and respected each and every step of his legacy. The Hospital, still in existence today, performs upwards of 7,000 operations a year, which are carried out by a staff varying from 10 to 12 dedicated surgeons.
Table 7.1 Review of Recurrences by Countries. Courtesy Pr. V. Schumpelick | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Table 7.2 Statistical Review (1999–2004) within Bavaria. Courtesy Pf V. Schumpelick | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
Local anesthesia became, very early, a standard practice. That possibility was convincingly established by Halsted and Cushing 50 years earlier. Early mobility became the norm as soon as surgery is terminated when the patient walks to the recovery room and ambulation is encouraged when the effects of the preoperative sedation have dissipated. This trend was begun when Earle Shouldice observed that children could not be kept in bed following herniorrhaphies and that their early activity never resulted in any ill after-effect.
Anatomy
The groin is unquestionably an area of the human anatomy which has long been recognized as a difficult area of study. This is probably due to the four dimensions of an anatomy which changes as one proceeds askew from front to back and from the midline to the side. A crab might have an easier time of it! Still, some important concepts must be retained which will ease the understanding of the complexities.
Without a doubt, the most complete study of the anatomy of the groin is provided by H. Fruchaud. His book, published in 1956 by Doin Publishers in France was difficult to find and the work had not been translated into English until 2006. As a result, very few authors had previously quoted from him in a limited manner. With Astley Cooper and Jules Cloquet, the Fruchaud has been one of the cornerstones in understanding the anatomy of the groin. A review of Fruchaud’s text reminds us that the groin anatomy must always be referred to in the vertical, time honored position and tradition! Not with the patient in the supine position as in the dissection room cadaver so that the floor of the inguinal canal is the pubic ramus (with the patient in the erect position) and NOT the so-called “transversalis fascia.” The transversalis fascia is the posterior wall of the inguinal canal with the patient in the standing position as well as in the supine position in this case. Another unfortunate deformation and confusion in the teaching of the anatomy of the groin is the definition of the transversalis fascia. The problem arose with Astley Cooper when he called the transversus muscle the transversalis muscle so that its continuation inferiorly became the transversalis aponeurosis or transversalis fascia. It should instead have been called transversus aponeurosis or transversus fascia which goes on to contribute to the posterior wall of the inguinal canal.
The true transversalis fascia is in fact the endoabdominal fascia which is continuous with the endopelvic fascia and the rest of the abdominal cavity. It is a very thin layer, marked by a profuse cellularity which differentiates it from the aponeurotic, sparse cellularity of the extensions infero-laterally of the transversus abdominis and internal oblique muscles. These last two fascial layers form the true posterior wall of the inguinal canal.
Another feature of Fruchaud’s inguinal description is the elimination of the inguinal ligament. There is no such ligament! It is simply a continuation, a reflection of the external oblique aponeurosis. What Fruchaud refers to as the inguinal ligament is in fact, the iliopubic tract (the ligament of Thomson), a structure seen at the lower edge on the deep surface of the divided posterior wall of the inguinal canal. It is not always a solid structure, especially at its lateral end. That is why the reflection of the external oblique aponeurosis must be included in the Bassini and the Shouldice inguinal hernia repair. Since usage has forced us to call “Transversalis Fascia” the posterior aspect of the inguinal canal, we will continue to do so to avoid confusion. It follows therefore that the lower extension of the transversalis fascia joins the inner aspect of the recurved and lower portion of the external oblique aponeurosis to continue inferiorly over the pubic ramus.
Obesity
Obesity is always a drawback in all surgery. Whereas the evidence is overwhelming on obesity being a factor in incisional hernia recurrences, the same cannot be said for inguinal hernias. Overweight makes surgery longer, will require more local anesthesia, and may limit ambulation after surgery. It will be a factor in postoperative infections. Otherwise, a moderate adiposity should not be an objection to inguinal hernia repair. It has been a custom at the Shouldice Hospital to promote weight loss and while the intent is noble, it is not always successful. Certainly not in the class that would be labeled obese. In larger centers, bariatric surgeons become part of the team.
Sedation
Preoperative sedation consists of Diazepam (10 to 25 mg, orally) 90 minutes prior to surgery and Meperidine (25 to 100 mg) 45 minutes before making the incision. These drugs can be varied to suit the needs and condition of the patient and the experience of the surgical and anesthetic teams. Intravenous sedation is not uncommon and can be an additional option.
Local Anesthesia
The Shouldice Hospital has had extensive experience with procaine hydrochloride (novocain) and continues to use it to this day. It is a safe, effective, and a cost-effective drug. The concentration is 1% to a maximum volume of 200 cc. Here again, the choice of anesthetic agent may vary with local customs and uses. Novocain has never been associated with malignant hyperthermia. It may induce tremulousness but this is properly controlled by the preoperative sedatives be they benzodiazepines or barbiturates. Properly carried out, in terms of quantity and timing of the medications, there is no doubt that adequate sedation and anesthesia can be effective and satisfying. The advantage of the method is that it makes surgery possible and safe for the majority if not all patients regardless of age and health status. Local anesthesia also imparts the benign nature that herniorrhaphies are in terms of surgery and safety, as many patients have a morbid and unreal fear of general anesthesia. Apprehension of cardiac complications are a justified risk particularly in the above 50 age group. These apprehensions were mapped out and at the risk of sounding trite through repetition, one must insist on that repetition. It has been established from the records of the Shouldice Hospital that the cardiac status of a patient population is as seen in Table 7.3.
Table 7.3 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The Incision
Most textbooks describe the inguinal incision 2 to 3 cm “above” a line joining the pubic crest to the anterior superior iliac spine. Experience has shown that the incision should be instead, along that line, not above. Also, it should be from the pubic crest laterally to a distance of 10 cm. This incision brings the inguinal area into full view without undue discomfort from the traction of retractors. This retraction is a source of marked discomfort under local anesthesia since it affects areas not covered by your local anesthesia.
Local Anesthesia
The infiltration of the skin is carried out by raising a wheal 3 to 4 cm wide at the site of the proposed incision. A volume of 60 to 90 cc of 1% procaine hydrochloride will be generous and sufficient (Fig. 7.2). After the initial incision is made, when the external oblique aponeurosis is identified, another 20 cc of anesthetic agent is injected deep to this aponeurosis allowing it to bathe the sub-aponeurotic space. Later, when this aponeurosis has been incised, all the nerves in the groin will be easily identified and infiltrated individually with 1 to 2 cc of the anesthetic agent. One must remember their tremendous variation and distribution. The genital branch of the genitofemoral nerve which issues from the deep inguinal ring appears on the lateral aspect of the cremasteric muscle and often within the substance of that muscle.
The Dissection
The external oblique aponeurosis is incised from the superficial inguinal ring laterally, along the direction of its fibers, to a level of 2 to 3 cm lateral to the deep inguinal ring (Fig. 7.3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree