Giant Prosthetic Ventral Hernia Repair
Gina L. Adrales
Giant hernia (Fig. 24.1 and 24.2) has been defined arbitrarily in the literature as greater than a diameter of 10 to 15 cm or an area of 170 to 200 cm2. As the survival of complex trauma and abdominal catastrophe patients has increased, the frequency and complexity of repairing the giant ventral defect have escalated. Obesity and loss of domain pose additional challenges. The relative indications and contraindications for giant synthetic prosthetic hernia repair are as follows:
Indications
Incisional or ventral hernia causing pain or obstructive symptoms
Contraindications
Ongoing wound infection is a contraindication to permanent synthetic mesh repair. Biologic mesh may be considered.
Prior significant wound infection, particularly involving methicillin-resistant Staphylococcus aureus, is a relative contraindication to permanent synthetic mesh repair.
Prohibitive operative risk in a patient without acute obstruction.
Careful evaluation of the patient is essential. Particular attention should be paid to the presence of obstructive pulmonary disease, chronic cough or constipation, prostatism, immunocompromised status, and obesity. Such factors, such as severe obesity, may alter the operative approach due to concern for abdominal compartment syndrome or may preclude a robust repair due to constant increased abdominal pressure. Thorough review of previous operative notes is helpful to discern the type and position of previous prosthetic material. Previous intraperitoneal mesh placement may be associated with increased abdominal adhesions. The surgeon should also inquire about previous wound or mesh infection.
Physical examination of the patient should include the following:
Measurement of the hernia defect(s)
Location of the defect(s) in relation to bony structures (e.g., iliac crest, pubis, xiphoid)
Chronic infection, foreign body reaction or skin breakdown, fistula
Palpable prior mesh
Presence of pannus and relation to hernia sac
Skin inspection (e.g., skin graft, eczema, psoriasis, cutaneous Candidiasis, chronic infection). Chronic skin conditions should be treated optimally, and fungal infection should be cleared prior to surgery.
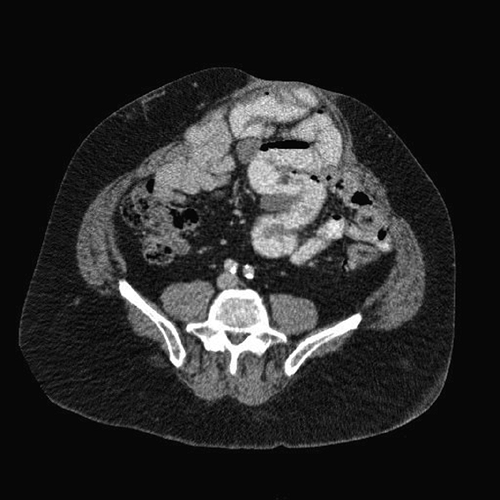
 Figure 24.3 CT scan of loss of domain. Note the large pannus. Proximity of the fascial defect to the bony pelvis also increases the complexity of this large hernia. |
Preoperative imaging is not imperative for all ventral hernias. However, such imaging can prove useful in the case of the giant ventral hernia. Preoperative CT or MRI should be obtained to determine the size of the fascial defect, presence of additional fascial defects, the proximity of the hernias to bony structures, degree of lateralization of the abdominal musculature, attenuation of the abdominal musculature, extent of bowel involvement, and loss of domain (Fig. 24.3).
Preoperative Risk Reduction
Due to the adverse effects of smoking and obesity on postoperative infection and wound complications, the patient must be counseled regarding preoperative smoking cessation and weight loss. While it may be unrealistic to require significant weight loss, a reasonable goal may often be set with the patient through comprehensive counseling regarding dietary and behavioral changes and the adverse effect of obesity on surgical outcome.
For patients who have loss of domain, preoperative treatment with progressive pneumoperitoneum or implantation of tissue expanders may be utilized to facilitate abdominal wall reconstruction and reduced risk of abdominal compartment syndrome. Botulinum injection has also been reported with success, though widespread data are lacking.
Chronic skin conditions should be treated optimally prior to surgery to reduce the risk of infection. Eradication treatment should be implemented for patients with recurrent infections with methicillin-resistant S. aureus.
Surgical Selection
Ideally, the surgical treatment of the giant hernia should result in a durable repair that also matches the goals of the patient. There is no universal algorithm to address the giant hernia. Instead, the care of these complex patients requires a tailored, individualized approach generated from the best medical evidence and modulated by both patient




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree