Single Incision Laparoscopic Surgery: Total Extraperitoneal Inguinal Hernia Repair
Brian P. Jacob
Introduction
Since the introduction of minimally invasive surgery as an alternative to traditional open surgery, numerous randomized studies have proven several advantages including better visualization, reduced postoperative pain, reduced wound and pulmonary complications, less immune suppression, speedier recovery time, and improved cosmesis. Subsequently, both physicians and industry have continued to investigate novel ways to advance minimally invasive surgery to augment patient satisfaction and outcomes. Several techniques have recently been introduced, including a resurgence of 2 mm and 3 mm instruments, natural orifice transluminal endoscopic surgery (NOTES), magnetic and robotic surgery, and single incision laparoscopic surgery (SILS), also known as laparoendoscopic single site surgery (LESS) or single port access (SPA) surgery. Of these options, SILS has seen the most rapid growth over recent years.
Despite two decades worth of laparoscopic advancements, currently only 18% of the 800,000 inguinal hernia repairs performed annually in the United States are performed laparoscopically. That being said, the slow adoption of novel techniques like NOTES and SILS into the specialty of inguinal hernia repair is not surprising. In fact, over the past 10 years, most of the advancements made for hernia repair have been focused on mesh products and fixation devices, and less so on access techniques. The reasons for this are multifactorial, but in part include overall costs and technical challenges involved in performing a laparoscopic inguinal hernia compared to that of an open repair.
SILS for inguinal hernia repair, first published in 2009 by Filipovic-Cugura’s group from Croatia, has since been supported by a handful of single center experiences. Also in early 2009, we showed the ability to perform a SILS Total Extraperitoneal Inguinal Hernia Repair (TEP) using a SPA device with routine laparoscopic instruments. In 2010, SILS TEP has continued to grow in popularity and more than 16 feasibility abstracts have been presented at international hernia conferences by groups from over 11 different
countries. Some of these studies have yet to be published. For instance, at the 2010 Asia Pacific Hernia Society meeting, Dr. Davide Lomanto’s group from Singapore presented their success following their initial experience with SILS inguinal hernia repair, while Dr. H Tran and colleagues recently presented over 100 cases from Australia at the European Hernia Society held in Istanbul, Turkey. A group from Spain, led by Dr. Salvador Morales-Conde, has also reported success with the technique at the same meeting. To date, however, there has likely been less than 500 cases performed worldwide, and within each of the presented case reports there are a number of significant variables that make it difficult to compare each of the cohorts. Therefore long-term outcomes need to continue to be assessed in institutional review board (IRB)-approved studies before the procedure can be more widely promoted.
countries. Some of these studies have yet to be published. For instance, at the 2010 Asia Pacific Hernia Society meeting, Dr. Davide Lomanto’s group from Singapore presented their success following their initial experience with SILS inguinal hernia repair, while Dr. H Tran and colleagues recently presented over 100 cases from Australia at the European Hernia Society held in Istanbul, Turkey. A group from Spain, led by Dr. Salvador Morales-Conde, has also reported success with the technique at the same meeting. To date, however, there has likely been less than 500 cases performed worldwide, and within each of the presented case reports there are a number of significant variables that make it difficult to compare each of the cohorts. Therefore long-term outcomes need to continue to be assessed in institutional review board (IRB)-approved studies before the procedure can be more widely promoted.
Table 18.1 Sample Available Single Port Access Devices | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The major technical variables that exist when performing a SILS TEP hernia repair include:
The access mechanism
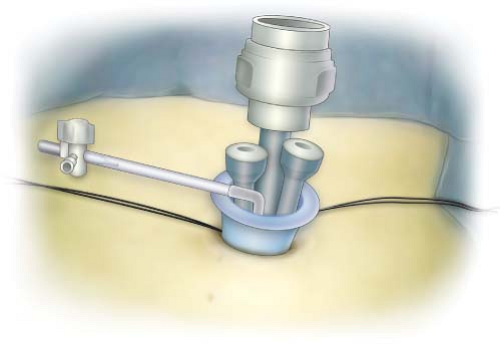
SPA device (Table 18.1)
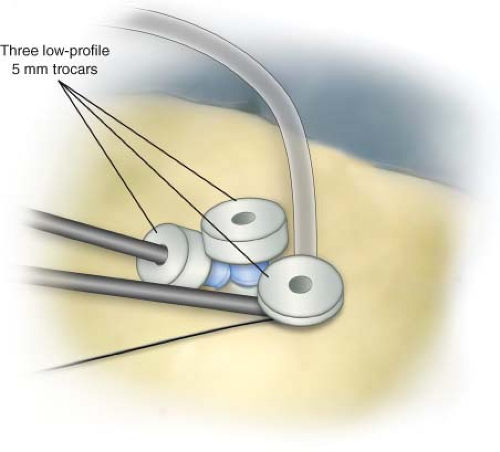
Traditional trocars inserted within a single skin incision (Figs. 18.1 and 18.2)
The instruments (standard, articulating, pre-shaped)
The camera type (flexible or standard)
Mesh and fixation device choices (surgeon specific)
When selecting a preferred technique from these variables, most surgeons adopt methods that most closely resemble their current practice with variations on the access
mechanism. The one common dominator mandatory for anyone adopting SILS TEP into their practice is that extensive experience with traditional laparoscopic inguinal hernia surgery is required. This chapter will review the common technical steps required to perform a single incision laparoscopic TEP inguinal hernia.
mechanism. The one common dominator mandatory for anyone adopting SILS TEP into their practice is that extensive experience with traditional laparoscopic inguinal hernia surgery is required. This chapter will review the common technical steps required to perform a single incision laparoscopic TEP inguinal hernia.
SILS TEP inguinal hernia repair is performed under general anesthesia, with the patient in the supine position with both arms adducted and pneumatic compression stockings for deep vein thrombosis prophylaxis placed. In all cases, a urinary (Foley) catheter is placed to decompress the bladder and a single dose of intravenous antibiotics is administered. The technical steps of entering and creating the preperitoneal working space with a balloon are the same as those described by Dr. Guy Voeller in 1995 for any routine TEP hernia repair. The single skin incision is made, and can be performed transversely within or about 1 to 2 cm below the umbilicus as well as vertically within the umbilical stalk depending on the anatomy of the umbilicus. The decision of where to put the incision is up to the surgeon and can be tailored to the desired shape of the patient’s umbilicus. The subcutaneous dissection is extended to over the anterior fascia of the rectus muscle. We prefer to place two stay sutures, one on the midline and one as lateral as possible, and use the stay sutures to elevate the fascia in order to facilitate making the fascial incision. Next, the anterior fascia is divided longitudinally for approximately 2.0 to 2.5 cm, but can be made smaller if using a SPA device that permits a smaller fascia incision. Finger dissection is then used to free the plane circumferentially beneath the fascia. A plane deep to the rectus muscle is then created down to the level of the pubic bone with a dilating balloon dissector under direct laparoscopic vision.
The set-up continues by removing the balloon dissector, and inserting a single port access device (Fig. 18.2). The depicted SPA device can be substituted with any of the other devices available, although most groups report success with the devices made by Covidien™ and Olympus™. Through this SPA device, a 12 mm and two 5 mm trocars are placed. In all cases, we used a routine 45° 10 mm laparoscope and standard reusable laparoscopic instruments, just as we use in our routine laparoscopic TEP repairs.
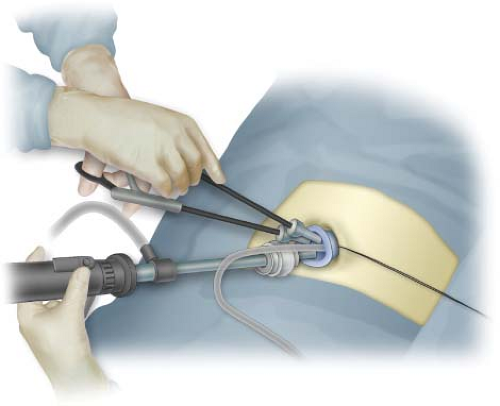
The TEP dissection and mesh insertion process proceed in a traditional laparoscopic TEP manner, and that description is beyond the scope of this chapter. Still, the peritoneum in all cases is reduced down to a level below the iliac vessels. The motions of the surgeon’s hands during the dissection may tend to be more in an upward and
downward motion from time to time (Fig. 18.3); however, the dissection should proceed without the feeling of restricted movements or instrument clashing and with complete ability to triangulate the instruments to perform a delicate and precise dissection. The use of a SPA device will prevent any air leak sometimes experienced with the insertion of multiple trocars.
downward motion from time to time (Fig. 18.3); however, the dissection should proceed without the feeling of restricted movements or instrument clashing and with complete ability to triangulate the instruments to perform a delicate and precise dissection. The use of a SPA device will prevent any air leak sometimes experienced with the insertion of multiple trocars.
In all cases of unilateral hernia, the contralateral side is also evaluated. If found, a contralateral hernia is also repaired. Once the repairs are completed and hemostasis is assured, the single port access device is removed, the fascia closed with a running 0-Vicryl suture, and the skin closed with 4-0 Monocryl sutures. 1% lidocaine is injected and a bandage applied. The Foley catheter is then removed at the end of the case.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree