, André Smout1 and Jan Tack2
(1)
Gastroenterology and Hepatology, Academic Medical Centre, Amsterdam, The Netherlands
(2)
Gastroenterology and Hepatology, UZ Leuven, Leuven, Belgium
4.1 Anatomy of the Esophagus
The esophageal lining consists of multiple layers of squamous epithelium. The transition from esophageal to gastric mucosa is called the z-line, because of the z-shaped appearance that one can find during endoscopy (Fig. 4.1).
Fig. 4.1
Schematic display of the anatomy of the esophagus (Published with kind permission of © Rogier Trompert Medical Art 2015)
The muscular layers of the pharynx continuously pass into the muscles of the upper esophageal sphincter (UES); all are striated muscle fibers. The UES consists of bundles of the cricopharyngeal muscle, which proximally pass into bundles of the pharyngeal constrictor muscles and distally pass into bundles of the circular esophageal muscles. The UES is controlled by the same nerves as the pharyngeal muscles and stands under voluntary control.
The muscular wall of the esophagus consists of two layers, an inner circular muscle layer and an outer longitudinal muscle layer. The nervous network of the myenteric plexus is found between the two muscle layers. The proximal one third of the esophageal muscles is striated, the middle third is a transition from striated to smooth muscle, and the distal third consists entirely of smooth muscle.
The lower esophageal sphincter (LES) also consists of smooth muscle and can be regarded as a local specialization of the circular muscle layer. The LES is normally found at the level where the esophagus leaves the thorax and enters the abdomen through the diaphragmatic hiatus. The LES and the muscular fibers of the diaphragm together form a functional entity that serves as a protection against gastroesophageal reflux.
4.2 Swallowing and Esophageal Peristalsis
The first step of digestion takes place in the mouth. By chewing, food is grinded and mixed with saliva. Saliva serves as a lubricant and contains amylase, an enzyme that digests starch. The muscles of the mouth and tongue push the food to the throat so it can be swallowed. In resting state, the esophagus is empty and the lumen is collapsed. The UES and LES exert a tonic pressure and seal off the esophagus. The onset of a swallow is voluntary, but the rest of the sequence that follows is reflexogenic. Swallowing is a well-organized movement of the mouth, tongue, throat, esophagus, and sphincters and results in transport of a bolus from the mouth to stomach. The swallow reflex inhibits respiration temporarily so that food does not enter the airways during swallowing. The swallow reflex starts when pressure sensors in the pharynx are stimulated. This activates an afferent nerve to the swallow center in brainstem. From there, motor neurons of the cranial nerves are activated that control the muscles of pharynx and upper esophagus (glossopharyngeal, vagal, and hypoglossal nerves) and the motor neurons of the vagus nerve that control the middle and distal esophagus.
A swallow can be divided into three phases, which are the oral phase, the pharyngeal phase, and the esophageal phase. In the oral phase the swallow is still under voluntary control. This phase starts when the tongue pushes part of the food in the mouth against the palate and moves it toward the back of the mouth. When the bolus reaches the pharynx, the pressure sensors will be activated and the swallow reflex will start.
The pharyngeal phase is entirely reflexogenic and consists of the following steps:
1.
The soft palate moves upward caused by the bolus below and closes off the nasopharynx.
2.
The vocal cords close and the larynx moves upward against the epiglottis. This prevents the bolus from entering into the airways and facilitates opening of the UES.
3.
The UES relaxes and the pharyngeal constrictors contract so the bolus is moved in distal direction.
4.
A peristaltic wave starts above the pharynx and moves in distal direction. This will push the bolus through the relaxed UES.
The bolus has entered the esophagus and the esophageal swallow phase has been initiated. After the bolus has passed the UES, the sphincter will close. The peristaltic wave initiated by the swallow (primary peristalsis) moves further in distal direction with a propagating velocity of 3–5 cm/s. The peristaltic wave will have traversed the esophagus in about 10 s. Peristalsis ensures that passage of food is also possible in supine position; gravity thus only plays a minor role.
If the esophagus is dilated in the absence of a swallowing, for example, during inflation of air during endoscopy, peristalsis will be triggered. This is called secondary peristalsis. The peristaltic wave will then start at the position where the distention took place.
The volume and viscosity of the bolus influence the amplitude and velocity of propagation of the peristaltic wave via input of sensory nerves to the enteric nervous system and central nervous system.
During swallowing the LES relaxes so the bolus can pass the sphincter and reach the stomach. After relaxation the sphincter contracts and returns to the tonic pressure of approximately 20 mmHg.
A swallowed liquid bolus usually passes the esophagus in one swallow, for a solid bolus temporarily hold-up halfway in the esophagus is not uncommon and only after several swallows the bolus is cleared from the esophagus.
4.3 Belches
With every swallow, some air is introduced into the esophagus. This air is transported to the stomach, together with the swallowed bolus. Gas can also be formed in the stomach, for example, after drinking carbon dioxide-containing beverages. In upright position the gas will move to the proximal stomach. Stretching of the fundus by the gas will activate stretch sensors in the gastric wall, and through afferent fibers of the vagal nerve, a reflex is initiated that results in relaxation of the LES so that the air can escape the stomach. The relaxation of the LES is in this case not triggered by a swallow and is called transient LES relaxation (TLESR). This reflex prevents overdistention of the stomach. When the air reaches the esophagus, it can either trigger secondary peristalsis and being pushed back to the stomach or, when the air reaches the proximal esophagus, it can induce reflexogenic relaxation of the UES and the air can escape. The vibrations of the pharyngeal structures caused by the air passage cause the typical sound associated with belching.
4.4 Motility Disorders of the Esophagus
Disorders of motility of the esophagus can lead to ineffective transport of food from the mouth to the stomach. This can cause difficulty in swallowing, the feeling of impaired esophageal bolus transit and retrosternal pain. When there is a sensation of difficulty in propulsion of food from the mouth or throat to the esophagus, it is called oropharyngeal dysphagia. When there is a sensation of the food not further passing down through the esophagus, it is called esophageal dysphagia. Pain can be caused by a bolus that gets stuck and stretches the esophageal wall or because spastic contractions are induced. This symptom is also known as odynophagia. Of course, dysphagia can also be caused by narrowing of the esophagus, such as occurs with a tumor or peptic stricture after long-standing reflux disease. In case of esophageal motility disorders, there is often esophageal dysphagia for both solid and liquid foods, while in case of obstructive disorders, there is often dysphagia for solids only.
Esophageal motility disorders are classified into primary and secondary motility disorders. Secondary motility disorders are caused by another disease, for example, scleroderma that affects the esophageal muscles.
In case of esophageal dysphagia, the first step is to exclude an organic cause using endoscopy. Biopsies are always taken to exclude the presence of allergic or eosinophilic esophagitis, even when the esophagus has a normal endoscopic appearance. When endoscopy did not reveal any abnormalities and biopsies are normal, further testing for motility disorders will be performed. Usually, the next step is esophageal manometry (Fig. 4.2). A barium esophagogram is made when there is a suspicion for a stricture (Fig. 4.3).

Fig. 4.2
Esophageal manometry in a subject with normal esophageal motility. Both conventional line tracings (a) are shown as well as colorplot tracings (b) as used in high-resolution manometry

Fig. 4.3
Barium esophagogram in a patient with mid-esophageal narrowing of lumen caused by eosinophilic esophagitis
4.5 Primary Esophageal Motility Disorders
4.5.1 Oropharyngeal Dysphagia
Dyskinesia of the UES is defined as a condition with poorly coordinated movements of the hypopharynx and UES. This results in symptoms of swallowing difficulty or aspiration. The sphincter may relax too late, too early, or not enough. Cricopharyngeal hypertrophy may also cause swallowing difficulties and aspiration. In this condition the resting pressure of the UES is increased and a Zenker’s diverticulum is formed just above the sphincter.
Because the first phase of swallowing is controlled by the central nervous system through the cranial nerves, disorders of the central nervous system and cranial nerves such as tumors, neurodegenerative disorders, and stroke also result in swallowing disorders. For example, swallowing disorders are highly frequent in Parkinson’s disease, sometimes making oral feeding impossible.
4.5.2 Esophageal Dysphagia
4.5.2.1 Achalasia
Achalasia is a disorder characterized by incomplete or absent relaxation of LES, in combination with absent esophageal peristalsis.
The severe abnormalities in esophageal motility are caused by destruction of the myenteric plexus. The cause for this is unknown but there are several hypotheses. It has been suggested that achalasia is partly genetic, an autoimmune disease, or caused by a virus. Achalasia can also be secondary to Chagas’ disease; in that case the ganglia are destroyed by the parasite Trypanosoma cruzi, which lives only in South America.
Achalasia can have its first presentation in patients of all ages, equally frequent in men and women. It may take long before a diagnosis is made, because the disease is rare and unknown and because the disease often starts slowly. The final diagnosis is made with esophageal manometry.
The symptoms in achalasia are caused by the inability of the esophagus to empty. This results in problems with food passage; swallowed foods may stick in the esophagus for hours before they are regurgitated again. Retrosternal pain can be caused by stretch on the walls of the esophagus, due to stasis of food, but probably also by spastic contractions. Weight loss is also common. Long-standing achalasia can result in dilatation of the esophageal body (Fig. 4.4).
Fig. 4.4
Barium swallow radiograph in a patient with achalasia. The esophageal lumen is distended, while at the level of the transition from the esophagus to the stomach, there is hardly any contrast visible (bird’s beak)
High-resolution manometry has revealed that there are several achalasia subtypes (Fig. 4.5). We distinguish classic achalasia (type I), achalasia with simultaneous increases in esophageal luminal pressure called pan-esophageal pressurization (type II), and achalasia with spastic contractions (type III). The achalasia subtypes differ in presentation, findings on manometry and barium esophagograms, and response to treatment.
Fig. 4.5
High-resolution manometry of achalasia subtypes. Type I achalasia (a) shows limited pan-esophageal pressurization after swallows; in the type II achalasia (b) there is pronounced pan-esophageal pressurization visible. Type III achalasia (c) is characterized by spastic contractions
The treatment of achalasia is focused on reduction of LES pressure, and this can be done in several ways. Medication such as nitrates and calcium channel blockers are insufficiently effective for long-term achalasia treatment. Botulinum toxin (Botox) can be injected endoscopically at the level of the LES. This is an effective and relatively safe treatment option that is mostly performed under mild sedation. Disadvantage is that the effect wears out after 3–6 months and frequent retreatment will be required.
Pneumodilation is another treatment option. A 3- to 4-cm wide balloon is placed endoscopically or under fluoroscopic control at the level of the LES. By filling the balloon with air (pneumodilation), the sphincter is dilated. The effect of pneumodilation persists longer than that of Botox injections, but sometimes repeated dilations are required. There is also a risk of perforation of the esophagus (about 2 %). With repeat dilations when indicated, long-term symptom control can be achieved in 70–90 % of patients.
Surgical treatment consists of a laparoscopic cleavage of the LES, myotomy according Heller. Usually this procedure is combined with a fundoplication according to Dor to reduce any reflux after the myotomy. Reflux symptoms may occur after all successful treatments for achalasia, as the sphincter pressure will be reduced and there is no peristalsis in the esophagus to clear refluxed gastric contents. Heller myotomy is very effective and 80–90 % of the patients treated will not need future re-treatments. However, the treatment is more invasive than endoscopic treatments and complications such as esophageal mucosal perforations do occur.
Recently, it has also become possible to perform a myotomy using an endoscopic approach. In a so-called per-oral endoscopic myotomy (POEM) procedure, the LES is cut endoscopically. The procedure is promising but it is new and long-term results are not available yet.
Esophagogastric junction outflow obstruction is a disorder characterized by poor relaxation of the LES in combination with sufficient evidence of esophageal peristalsis. Typical symptoms are chest pain and dysphagia and the disorder may be an early stage of achalasia. Not all patients with manometric signs of esophagogastric junction outflow obstruction need treatment; symptoms may disappear spontaneously.
4.5.2.2 Distal Esophageal Spasm
Spastic contractions of esophageal muscles can cause retrosternal pain and dysphagia. Sometimes these pains come in attacks and may mimic cardiac pain. Not infrequently patients have been admitted to a coronary care unit several times before they are referred to the gastroenterologist for analysis of their noncardiac chest pain. Distal esophageal spasms are diagnosed with esophageal manometry (Fig. 4.6). Premature rapid propagating contractions are seen in the esophagus. Sometimes spastic contractions are also seen during endoscopy and on radiographic images (Fig. 4.7).
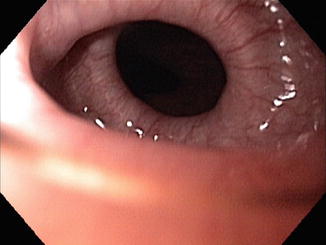
Fig. 4.6
High-resolution manometry picture of spastic contraction in distal esophagus
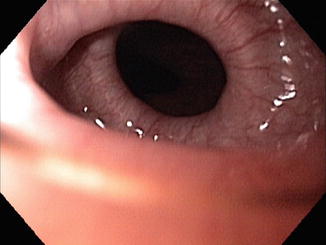
Fig. 4.7
Endoscopic picture of spastic contractions in the esophagus
Attacks of spasms are frequently triggered by emotions or by eating food. Gastroesophageal reflux can also trigger spasms. Sometimes patients have symptom very infrequently, which can make it difficult to make a diagnosis as the spastic contractions may not be visible on manometry in asymptomatic periods.
For management of spasms, it is of utmost importance to explain about the cause of the pain. Once the patients understand that the pain is caused by a benign disorder, this will substantially reduce anxiety during an attack. Medications that induce smooth muscle relaxation, such as nitroglycerine and calcium channel blockers, are moderately effective, although side effects such as headaches and hypotension may complicate effective dosing. In case of severe symptoms and insufficient effect of medication, endoscopic injections with botulinum toxin or even myotomy may be considered. Of course, when there is suspicion that reflux plays a role, this will need to be treated as well. Generally, the vast majority of patients with spasms use acid suppressants.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








