Sphincteroplasty of Biliary and Pancreatic Ducts
Thomas J. Howard
 INDICATIONS/CONTRAINDICATIONS
INDICATIONS/CONTRAINDICATIONSTransduodenal sphincteroplasty (TS) for abnormalities of the biliary and pancreatic duct sphincters is an operation that has generated a great deal of study and interest by both gastrointestinal endoscopists and surgeons. The reason for this attraction is that if true, these syndromes validate a fundamental pathophysiologic concept related to restrictions of flow in a secretory organ. For the pancreas, this involves either a developmental malformation resulting in an inadequately sized sphincter (pancreas divisum), or an acquired sphincter stenosis due to passage of gallstones and/or inflammation [sphincter of Oddi dysfunction (SOD)] both leading to pancreatic-type pain or recurrent episodes of acute pancreatitis. For the liver, the acquired sphincter stenosis, presumably again from passage of gallstones and debris, results in biliary-type pain and liver function test elevations. In both of these situations, the secretory organ somehow ascertains this flow restriction and responds with inflammation (pancreatitis, hepatitis) and symptoms experienced in the organism as pain. Sphincter enlargement of the pancreatic or biliary orifice, or both, either through endoscopic sphincterotomy (ES) or transduodenal sphincteroplasty (TS) should alleviate this flow restriction and its attendant organ response leading to pain relief. Despite this appealing theory, the level of scientific evidence to support either TS or ES for abnormalities of the biliopancreatic sphincters remains meager at best (Level C, Level II-3), certainly not sufficient to establish a causal relationship between stenosis and symptoms. Unfortunately, both medical and surgical data on this topic consist almost exclusively of small case series containing fundamental methodologic flaws including referral bias, lack of blinding, absence of a control group, and short clinical follow-up. As there are no animal models of spontaneously occurring sphincter dysfunction to investigate, all data is derived from humans, which to date, has been carried out without a proper placebo-controlled population. Despite these limitations, there still exists a substantial body of literature reporting decreasing pain scores, reduction in episodes of acute pancreatitis, and reduction in recurrent hospitalizations, in approximately three-quarters of selected patients treated by either
ES or TS, a level of success that cannot be easily be ignored. Perhaps the key word in the above sentence is “selected” as it is clear that there are substantial overlap between symptoms of patients with hypertensive pancreatic or biliary sphincters and those with chronic pancreatitis, alcohol or narcotic addiction, or visceral hypersensitivity syndromes.
ES or TS, a level of success that cannot be easily be ignored. Perhaps the key word in the above sentence is “selected” as it is clear that there are substantial overlap between symptoms of patients with hypertensive pancreatic or biliary sphincters and those with chronic pancreatitis, alcohol or narcotic addiction, or visceral hypersensitivity syndromes.
Historically, early operative series of TS reported encouraging results in effective symptom control with low associated morbidity and mortality rates. Advances in endoscopic imaging and instrumentation promoted the development of ES, a minimally invasive technique that has supplanted operative TS in the majority of patients with pancreatic or biliary sphincter abnormalities. The ability to manometrically measure biliary and pancreatic duct sphincter pressures endoscopically has brought about the convergence of both diagnosis and treatment within one procedure such that most patients with SOD or pancreas divisum are now treated by ES at the time of their initial diagnosis. This synchronous diagnostic-therapeutic endeavor, while efficient, discourages collaboration and randomization possibly contributing to the slow progress in this field. As another consequence of this efficiency, only a small percentage of patients are now considered candidates for operative TS: Those who have failed one or more prior ESs or those with anatomic abnormalities limiting the endoscopic access to their major or minor papilla (post-bariatric or gastric surgery). From a surgeon’s perspective, this results in the paradox that while the total number of patients having TS has declined, the complexity level of each operation (reoperative field, prior gastric surgery, strictured ES) has increased. In this situation, both experience and sound clinical judgment are paramount in achieving optimal therapeutic outcomes. As a byproduct of this endoscopic selection bias and declining referral patterns, the surgical literature over the last decade has focused on improving the indications and patient selection criteria for TS in an effort to maximize long-term benefits. For the purpose of our discussion in this chapter, there are currently three solid indications for TS:
Impacted gallstone unable to be extracted by endoscopic methods
Sphincter of Oddi dysfunction
Pancreas divisum with dominant dorsal duct anatomy
Impacted Gallstone Unable to be Extracted by Endoscopic Methods
As touched on in the introduction, improved functionality of endoscopic retrograde cholangiopancreatography (ERCP) coupled with extracoporeal shock wave lithotripsy (ESWL) for stone fragmentation, has made an impacted gallstone at the ampulla of Vater a rare indication for TS.
Sphincter of Oddi Dysfunction
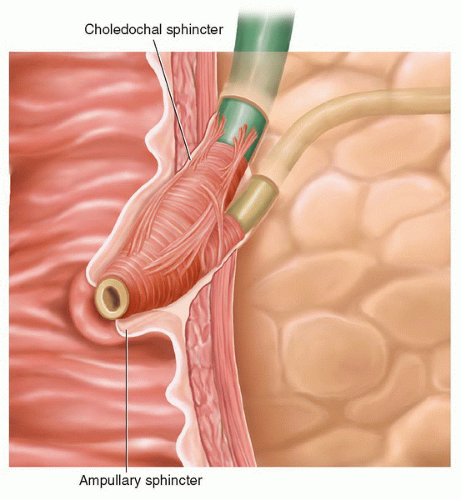
SOD is defined as a benign, noncalculus obstructive disorder occurring at the level of the sphincter of Oddi which, depending on the dominant manifestation, can produce either biliary or pancreas predominant symptoms although significant abnormal manometric findings in both sphincters exist (Fig. 15.1). Encompassed by this nebulous definition is a wide variety of abnormalities running the gamut from mechanical fibrotic stricturing secondary to the passage of gallstones to dysmotility conditions caused by a defective neuronal or hormonal milieu. Pancreas or biliary-type pain syndromes, cholestasis, and recurrent episodes of acute pancreas without another etiology are all contained under this large umbrella of clinical manifestations which are believed to be due to a hypertensive sphincter segment which fails to relax normally under the influence of CCK, other gastrointestinal hormones, and cholinergic neural factors during a meal. This physiologic obstruction acts as a deterrent to the flow of bile and pancreatic juice into the intestine during a meal. A large number of indirect clinical tests have been evaluated (radionucleotide, ultrasonography, magnetic resonance imaging, morphine-neostigmine) in an effort to quantify this “functional obstruction” and identify patients
with this disease. Endoscopic sphincter of Oddi manometry (ESOM), which directly measures sphincter pressures in real time, remains the only objective measure to accurately predict beneficial outcomes from either ES or TS. Manometric studies of normal human subjects reveal a basal sphincter pressure of approximately 10 mm Hg over which are superimposed episodic contractions with a frequency of 2 to 6/minute and an amplitude of 50 to 140 mm Hg above duodenal pressure. The complexity of these recordings makes the interpretation of pathophysiologic derangements challenging due to multiple potential abnormalities including elevated basal sphincter pressure, lack of superimposed contractions, or absence of sphincter relaxation. Given our present level of understanding, the most objective information on which to base a decision for operation in patients with SOD is finding an elevated basal sphincter pressure greater than 40 mm Hg. Large clinical experience from the endoscopy groups in both Wisconsin and Indiana have facilitated the grouping of patients with either predominate biliary-type pain or pancreatic-type pain and their associated clinical and manometric findings into a classification system useful for predicting their response to ES (Table 15.1).
with this disease. Endoscopic sphincter of Oddi manometry (ESOM), which directly measures sphincter pressures in real time, remains the only objective measure to accurately predict beneficial outcomes from either ES or TS. Manometric studies of normal human subjects reveal a basal sphincter pressure of approximately 10 mm Hg over which are superimposed episodic contractions with a frequency of 2 to 6/minute and an amplitude of 50 to 140 mm Hg above duodenal pressure. The complexity of these recordings makes the interpretation of pathophysiologic derangements challenging due to multiple potential abnormalities including elevated basal sphincter pressure, lack of superimposed contractions, or absence of sphincter relaxation. Given our present level of understanding, the most objective information on which to base a decision for operation in patients with SOD is finding an elevated basal sphincter pressure greater than 40 mm Hg. Large clinical experience from the endoscopy groups in both Wisconsin and Indiana have facilitated the grouping of patients with either predominate biliary-type pain or pancreatic-type pain and their associated clinical and manometric findings into a classification system useful for predicting their response to ES (Table 15.1).
TABLE 15.1 Modified Milwaukee Classification System with Criteria for Both Biliary and Pancreatic Sphincter of Oddi Dysfunction | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Pancreas Divisum
Pancreas divisum is an embryologic abnormality where the dorsal and ventral duct segments during their complex counter-clockwise rotation around the GI tract fail to fuse during embryogenesis. In this situation, the dorsal pancreatic duct which drains a large portion of pancreatic parenchyma (anterior head, body, and tail segments) drains into the duodenum through the minor pancreatic duct sphincter (duct of Santorini) (Fig. 15.2). This particular developmental abnormality is common based on autopsy studies, and is estimated to occur in approximately 8% of the general population. Interestingly, only a subset of patients with this developmental abnormality will have either episodes of recurrent pancreatitis or abdominal pain syndromes felt to be related to this altered anatomy. Similar to SOD, the pathophysiologic basis for these symptoms is presumed to be a relative outflow restriction/obstruction caused by pancreatic secretions traveling through a congenitally narrow minor pancreatic sphincter rather than the more patulous major pancreatic sphincter (duct of Wirsung). This relative outflow tract obstruction causes pancreatic ductal hypertension, which, in susceptible patients, produces acute recurrent pancreatitis (ARP) and pancreatic pain syndromes. Despite this appealing hypothesis, direct supporting evidence for this theory remains vague and indirect, implying that other as yet identified factors (i.e., genetic, environmental, or psychological) may play a crucial role in the ultimate clinical expression of this disease. Because of this variability in disease expression, accurate identification of patients who will benefit from TS remains a clinical challenge, bordering more on art than science.
ERCP is the reference standard for the diagnosis of pancreas divisum and other dorsal duct variants although recent improvements in image acquisition and resolution has allowed several noninvasive techniques such as: Endoscopic ultrasound (EUS), magnetic resonance cholangiopancreatography (MRCP) with secretin stimulation, and multi-detector row CT (MDCT) with post-processing reformations to approximate the accuracy of ERCP in making this diagnosis. In patients with PD, the ventral pancreatic duct is typically from 1 to 4 cm in length and is formed by finely tapered normal ducts servicing the anatomic distribution of the posterior pancreatic head and uncinate process (remnant ventral pancreatic bud). This ductal morphology appears normal up to the point of prompt duct termination, always found on the right side of the midline. When this anatomic relationship is recognized during ERCP, it is essential that cannulation of the minor papilla be pursued to demonstrate the presence of dominant dorsal duct anatomy and exclude the possible secondary causes of ductal obstruction such as tumor (pseudo divisum) or chronic pancreatitis (false pancreas divisum). EUS is a useful tool not only to identify this anatomy but also to evaluate the pancreatic parenchyma for small focal parenchymal abnormalities that could explain the ductal changes seen. It seems prudent in the contemporary evaluations of these patients to include both ductography (ERCP, EUS, MRCP) and a method of parenchymal evaluation (EUS, MRCP, CT) to fully characterize the disease process and discern whether or not operative intervention is appropriate.
In a patient with PD and recurrent pancreatitis or pancreatic pain syndromes, identification of a dominant dorsal duct system is a necessary but not sufficient finding to establish their candidacy for accessory papilla therapy. As previously mentioned, while 8% of the general population has PD, it is only in those patients with outflow tract obstruction due to accessory papillary stenosis where endoscopic or surgical sphincteroplasty has a high likelihood of success. The dorsal pancreatic duct in most patients with PD has a normal, nondilated appearance, making the demonstration of outflow tract obstruction demanding. Of those tests which have been studies, simple endoscopic assessment of accessory papilla size, degree of difficulty encountered during endoscopic cannulation (indirect assessment of patency), as well as direct manometric measurements of sphincter pressures have all proven unreliable in predicting the response of patients to sphincterotomy. Direct evidence of outflow obstruction, identified by duct imaging techniques utilizing either EUS or MRCP, both before and after an intravenous bolus of secretin to stimulate pancreatic secretions, has been advanced as a provocative test to identify patients with PD who will benefit from dorsal duct therapy. Stenosis of the minor papilla causing outflow obstruction is defined utilizing secretin-stimulated




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree