Left and Extended Left Hepatectomy
Peter J. A. Lodge
Introduction
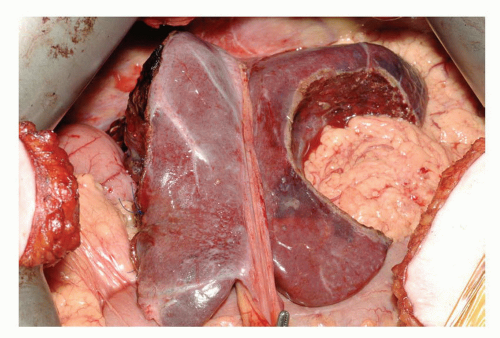
Anatomic left-sided hepatic resections can be described as left lateral sectionectomy (resection of segments 2 and 3), left hemihepatectomy (resection of segments 2, 3, and 4 ± 1) and left hepatic trisectionectomy (or extended left hepatectomy, resection of segments 2, 3, 4, 5, and 8 ± 1). En bloc resection of the caudate lobe (segment 1) may be performed in conjunction with left or extended left hepatectomy for various diagnoses (see Chapter 22).
Left lateral sectionectomy is commonly performed laparoscopically today and the laparoscopic technique is described in Chapter 31. This is one of the most minor hepatectomies and a detailed description is not necessary. It is mentioned here only for completeness.
Left hemihepatectomy is more challenging and is most usually performed by an open surgery, although more expert laparoscopic surgeons are beginning to carry it out.
Left hepatic trisectionectomy was first described in detail by Starzl as left trisegmentectomy in 1982. The procedure has recently been renamed because of an international confusion in nomenclature: Terms such as extended left hepatectomy have become ill-defined. It remains a procedure used in few highly specialised units primarily for the treatment of extensive and advanced hepatic or biliary diseases: I reported my own unit’s experience with 70 cases of left hepatic trisectionectomy in 2005 and this experience now extends to 100 cases of this difficult operation. Despite the advances in surgical and anesthetic techniques made in recent years, left hepatic trisectionectomy is still thought to be associated with higher rates of morbidity and mortality than other resections. This is mainly attributable to the aggressive nature of the (usually malignant) disease being treated, but may also be related to the extent of liver volume being resected, estimated at approximately 80% by several authors. It should be noted, however, that the volume of the liver remnant after left trisectionectomy (segments 6 and 7) is generally greater than that remaining after right trisectionectomy (segments 2 and 3). Despite this, we have demonstrated that it is possible to extend the procedure to include parts of segments 6 and 7. This procedure has enabled the resection of advanced tumors with curative intent. Despite advances in surgical technique and perioperative management, it remains the most challenging of the major anatomic hepatectomies with higher complication rates than other hepatic, and worldwide experience remains small. The
infrequency with which it is performed and the absence of surface landmarks to guide the resection both contribute to the higher morbidity. Although several authors have focused on this complicated hepatectomy, few reports have described the results of large series and long-term follow-up has rarely been considered.
infrequency with which it is performed and the absence of surface landmarks to guide the resection both contribute to the higher morbidity. Although several authors have focused on this complicated hepatectomy, few reports have described the results of large series and long-term follow-up has rarely been considered.
The comments below, therefore, relate primarily to left hemihepatectomy and left hepatic trisectionectomy.
Patient Selection
Cardiorespiratory Assessment
Before considering a surgical procedure of this scale, it is essential to be as sure as possible that the patient is fit enough to withstand the operation. It is important to take a detailed history of previous cardiovascular diseases, including myocardial infarction, angina pectoris, and hypertension. Clearly, a history of smoking or peripheral vascular disease should raise the clinical suspicion of coronary artery disease. Respiratory diseases, particularly emphysema and chronic bronchitis, are quite prevalent in the elderly population and clinical examination with chest radiology can be helpful.
Resting and exercise electrocardiography are the standard cardiologic objective assessment tests in our center. Failure to achieve an adequate heart rate for true stress testing can be a problem in the elderly population, most often due to osteoarthritis of the hips and knees. In this situation, a great deal of useful information can be gained from echocardiography, with measurement of end diastolic and systolic volumes to calculate left ventricular ejection fraction, or by radioisotope assessment with dobutamine stress. Failure to complete these investigations or a significant depression of the ST segment on the exercise ECG is a clear indication for coronary artery angiography. This procedure is carried out in 3% of major liver surgery candidates in our experience, ruling out surgery in 1% but providing reassuring information in the rest. Only a few patients in our experience have been suitable for preoperative coronary artery angioplasty, stenting or bypass grafting prior to liver surgery, but these are clearly potential treatment options to consider.
Routine lung function tests including vital capacity and forced expiratory volume form part of our standard assessment as well as chest radiology. Useful information is also gained from the chest CT, which is done primarily to look for lung metastases and diaphragm involvement by the hepatic tumor. The CT appearances of emphysema in particular are characteristic. In our northern UK population, because of the high incidence of emphysema and chronic obstructive airways disease, we occasionally consider blood gas sampling preoperatively.
Hepatic Reserve Assessment (see Chapter 18)
Preoperative blood tests necessary before proceeding to major resection include full blood count, urea and electrolytes, liver function tests, clotting screen and tumor marker studies. Prothrombin time, bilirubin and albumin give a fairly accurate indication of global hepatic function, but in some cases, a liver biopsy of the residual tumor-free liver will also be necessary if there is a doubt about hepatic reserve, in particular, when considering resection for hepatocellular carcinoma. This is particularly important in the group of patients with a previous history of excess alcohol consumption or if there is serologic evidence of hepatitis B or C. It is also useful when dealing with cholangiocarcinoma, as there may be underlying sclerosing cholangitis.
It is inevitable that a degree of temporary hepatic failure will be induced in some patients undergoing very major resection. More work needs to be done in this interesting area. If the tumor-free segments are affected by biliary obstruction, it is our current practice to attempt biliary decompression by endoscopic or percutaneous techniques a few days in advance of surgery as this may speed up the postoperative recovery and
reduce risks for morbidity and mortality in major liver surgery. In most cases of major left hepatectomy, the volume of the right liver remnant, even if only segments 6 and 7, is generally adequate, and preoperative portal vein embolization is usually unnecessary. We have not used portal vein embolization routinely.
reduce risks for morbidity and mortality in major liver surgery. In most cases of major left hepatectomy, the volume of the right liver remnant, even if only segments 6 and 7, is generally adequate, and preoperative portal vein embolization is usually unnecessary. We have not used portal vein embolization routinely.
Radiology Assessment
Although MRI is the imaging method of choice for the liver in our center, other groups routinely use CT arterioportography with similar results. Three dimensional CT and MRI imaging technology continue to improve and may be of value in planning the surgical approach. It is our current practice to use CT scanning of chest, abdomen and pelvis to exclude extrahepatic disease for all tumor types, but FDG-PET scanning is also used in selected cases, particularly biliary tract cancers. Screening for primary site recurrence (e.g., colonoscopy) is also clearly important. An isotope bone scan may be useful in patients with advanced disease.
 PREOPERATIVE PREPARATION
PREOPERATIVE PREPARATIONRoutine blood tests in our unit include full blood count, urea and electrolytes, liver function tests, coagulation screen, C-reactive protein (CRP), blood group and save, and tumor marker studies (primarily carcinoembryonic antigen [CEA], CA19-9, and alpha feto protein) immediately before surgery as a baseline. A low molecular weight heparin may be administered on the night before surgery to reduce the risk of deep vein thrombosis and pulmonary embolism for patients admitted preoperatively and at the end of surgery admitted on the day of surgery. Broad spectrum antibiotics are given at the time of anesthetic induction.
Anesthesia
It is our routine to place a central venous line and a urinary catheter for careful monitoring. A warm air flow device covers the patient as well as a standard warming blanket underneath. We use an air-oxygen-desfurane-based anesthesia which has been shown to minimise the derangement of postoperative liver function, with infusions of n-acetyl cysteine and antioxidants to confer hepatic protection. We use an accepted methodology for low central venous pressure anesthesia and we use an epidural catheter for central venous pressure manipulation as well as postoperative analgesia, although vasodilators are sometimes necessary in addition. Inotropic/vasoconstrictor support, primarily with norepinephrine or phenylephrine, is often necessary for the elderly patients to support blood pressure during surgery.
 OPERATIVE TECHNIQUE
OPERATIVE TECHNIQUELeft Lateral Sectionectomy
A strictly anatomical approach is unnecessary. Left lateral sectionectomy is considered for tumors obliterating much of hepatic segments 2 and 3 or compromising the portal triad structures for these segments. A lesser resection should usually be planned for more peripheral tumors and parenchyma-sparing techniques offer the patient a potential lifeline for re-resection if a further liver tumor occurs in the future. A resection of segment 2 or 3 individually (see Chapter 24) or wedge excisions for smaller peripheral tumors can be performed. This can often be combined with a right liver resection (Fig. 20.1). The use of ultrasonic dissection (CUSA, Valleylab, Inc., Boulder, CO) or alternative appropriate parenchymal-dissection techniques negates the need for vascular control in most cases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree