Central Pancreatectomy
Cristina R. Ferrone
Carlos Fernández-del Castillo
Andrew L. Warshaw
 INDICATIONS/CONTRAINDICATIONS
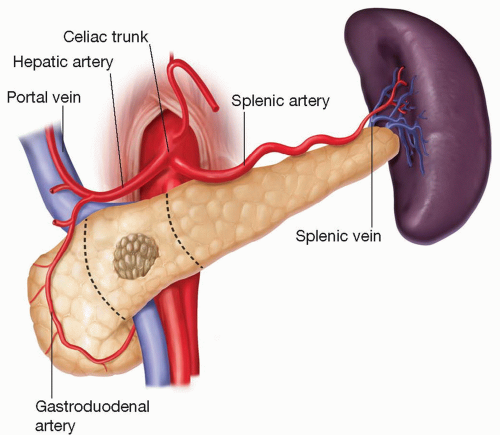
INDICATIONS/CONTRAINDICATIONSCentral pancreatectomy provides patients and surgeons an alternative to an extended pancreatic resection or enucleation of lesions located in the neck or body of the pancreas (Fig. 6.1). Central pancreatectomy was first described by Guillemin and Bessot in 1957 and was first performed for a neoplasm by Dagradi and Serio in 1984. The procedure was popularized in North America by Warshaw et al. after publishing their experience of 12 middle pancreatectomies for 7 cystic lesions, 4 neuroendocrine tumors and 1 intraductal papillary mucinous tumor. Segmental resection has been adopted by many for benign or borderline lesions, focal chronic pancreatitis, and trauma. If a central pancreatectomy is not performed, lesions located in the mid portion of the pancreas would require an aggressive surgical resection, such as an extended pancreaticoduodenectomy or extended distal pancreatectomy. The main advantage of central pancreatectomy compared to an extended resection is the ability to conserve more pancreatic parenchyma, thereby preserving exocrine and endocrine function. The long-term incidence of new onset diabetes mellitus ranges from 50% to 57% of patients undergoing distal pancreatectomy in comparison with 11% for patients undergoing central pancreatectomy. Exocrine insufficiency requiring enzymes occurs in 27% of patients undergoing distal pancreatectomy as opposed to 10% of patients undergoing central pancreatectomy. An additional advantage is the preservation of normal upper gastrointestinal and biliary anatomy. Central pancreatectomy also assures preservation of the spleen. Splenic preservation not only decreases operative duration, morbidity and length of stay, but also reduces the risk of post splenectomy sepsis, malignancy, and reactive thrombocytosis which can result in a myocardial infarction. While enucleation of a pancreatic lesion also preserves pancreatic parenchyma and upper gastrointestinal anatomy, it can result in disruption or compromise of the pancreatic duct. We do not recommend a central pancreatectomy for patients with ductal adenocarcinoma due to potentially inadequate elimination of the relevant lymphatic drainage. Adequate lymph node dissection is essential for accurate staging of patients with malignant lesions and may influence their long-term survival.
Important points to evaluate when considering a central pancreatectomy are as follows.
1. The lesion should be benign or borderline (pathologic frozen section at the time of surgery is essential to assure that the margins are free of tumor).
2. The lesion should be located in the neck or proximal body of the pancreas.
3. Enucleation is an undesirable option if the main pancreatic duct is close and likely to be disrupted.
4. The distal pancreatic stump should be at least 6 cm in length to make its conservation worthwhile.
 PREOPERATIVE PLANNING
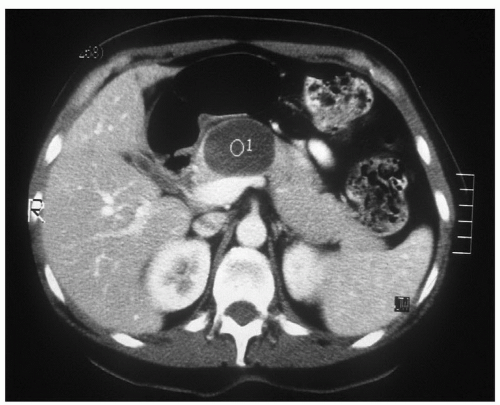
PREOPERATIVE PLANNINGAbdominopelvic contrast-enhanced computed tomography (CECT) or magnetic resonance cholangiopancreatography (MRCP) should be performed for preoperative evaluation. These imaging studies are essential to determine the anatomic relationship of the neoplasm to the pancreatic duct, portal vein, superior mesenteric vein, superior mesenteric artery, common hepatic artery, and splenic vessels. Understanding the relationship of the lesion to these landmarks is essential to determine if a central pancreatectomy is the appropriate operation and to performing a safe operation.
For patients in whom the precise diagnosis of the pancreatic neoplasm is unclear, an endoscopic ultrasound with fine-needle aspiration may be desirable. The fine-needle aspirate will provide tissue to make a histologic diagnosis, while the endoscopic ultrasound assists in outlining anatomic landmarks.
 SURGICAL TECHNIQUE
SURGICAL TECHNIQUEThe pancreatic lesion needs to be deemed resectable. Therefore, the lesion needs to be evaluated relative to pertinent anatomical landmarks as noted above. Central pancreatectomy is only recommended for benign or borderline lesions; therefore vascular involvement or adjacent organ invasion should be absent. For a central pancreatectomy to be worth this added effort and risk of complications, the distal pancreas should
measure at least 6 cm in length to ensure adequate length for an anastomosis and to add significant endocrine and exocrine capacity over what would be lost with a distal resection.
measure at least 6 cm in length to ensure adequate length for an anastomosis and to add significant endocrine and exocrine capacity over what would be lost with a distal resection.
Positioning
The patient is placed in the supine position with both arms out. All patients should have adequate intravenous access, a Foley catheter, deep venous thrombosis prophylaxis and receive appropriate antibiotic prophylaxis, depending on the individual’s allergies.
Technique
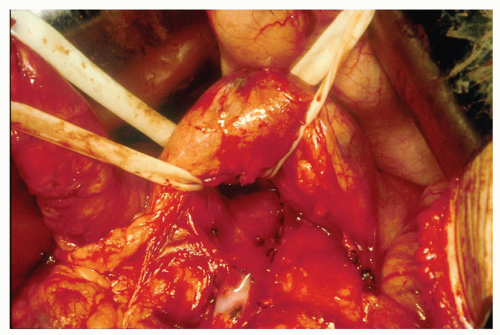
An upper midline incision is made from the xiphoid to the umbilicus. The abdomen is inspected to rule out metastatic disease or any other pathologies. The gastrocolic omentum is divided outside the gastroepiploic vessels, and the lesser sac is entered. The stomach is retracted cephalad and the transverse colon and omentum caudad. Adhesions in the lesser sac are lysed. The neck, body, and tail of the pancreas will then be visible (Fig. 6.2). The peritoneum along the superior and inferior borders of the pancreas is incised, and the pancreatic neck is mobilized. The relationship of the lesion to the portal vein, superior mesenteric artery and vein, and the common hepatic artery must be clarified (Fig. 6.3). Attention must be given not to avulse branches between the
splenic artery or vein and the pancreas; careful ligation of some of these branches may be required for adequate mobilization of this pancreatic segment. Usually the splenic vessels can be preserved. If this is not possible, we either suture ligate or staple the splenic vessels and rely on the short gastric vessels for splenic perfusion.
splenic artery or vein and the pancreas; careful ligation of some of these branches may be required for adequate mobilization of this pancreatic segment. Usually the splenic vessels can be preserved. If this is not possible, we either suture ligate or staple the splenic vessels and rely on the short gastric vessels for splenic perfusion.
 Get Clinical Tree app for offline access 
|