Roux-en-Y Lateral Pancreaticojejunostomy for Chronic Pancreatitis
Charles J. Yeo
Eugene P. Kennedy
Keith D. Lillemoe
 INDICATIONS/CONTRAINDICATIONS
INDICATIONS/CONTRAINDICATIONSChronic pancreatitis is a single term applied to a complex spectrum of disease. The essence of this disease process is the progressive destruction of the pancreatic parenchyma and its replacement with fibrotic tissue, which over time, leads to both exocrine and endocrine insufficiency.
The most common etiology of chronic pancreatitis is chronic excessive ethanol consumption, followed by other toxic or metabolic causes such as hypercalcemia, hyperlipidemia, certain medications, and perhaps tobacco. Other well-described etiologic factors for chronic pancreatitis include hereditary pancreatitis, cystic fibrosis, autoimmune disease, prior severe acute pancreatitis with necrosis, and pancreatic ductal obstruction from developmental abnormalities (pancreas divisum), sphincter of Oddi dysfunction, or obstruction from trauma or neoplasm. Patients not fitting one of these diagnostic categories are classified as idiopathic, a group that ranks second to ethanol consumption when etiologies are tallied.
The hallmark symptom is chronic, often disabling pain. The pain is classically located in the epigastric region and presents as a dull ache that radiates to the back. The exact nature of the pain and the timing of its occurrence in relationship to other aspects of the disease can vary greatly between patients. Some patients experience intermittent pain that can last days and be disabling. Fatty foods are often cited as a trigger, but the pain can frequently arise without any obvious trigger. Between episodes, these patients can be symptom free but the severity, duration, and frequency of episodes often increases over time. Other patients experience a more chronic, daily form of pain with intermittent exacerbations. The onset of episodes of chronic pain can vary greatly between patients, with certain patients experiencing pain early in the course of chronic pancreatitis while, less commonly, other patients can exhibit endocrine and exocrine insufficiency and dramatic radiographic evidence of chronic pancreatitis without any significant pain episodes.
The pain associated with chronic pancreatitis is typically the most disabling feature of the disease and the symptom that drives patients to seek frequent medical attention.
Since the pain typically increases over time, patients may become addicted to narcotic pain medications and often require episodic inpatient care. The pain and the side effects of pain medications dramatically impair quality of life and often result in disability and loss of employment. Ultimately, failure of medical approaches to pain management leads patients to surgical intervention for their conditions.
In addition to chronic pain, patients with chronic pancreatitis often present with a combination of other symptoms related to the exocrine and endocrine insufficiency that results from destruction of the gland. Steatorrhea, malabsorption, fat soluble vitamin deficiencies, malnutrition, and weight loss are all common. Diabetes may result from impaired islet cell function. Associated medical problems from long-term ethanol abuse as well as side effects from narcotic pain medications are also common.
The diagnosis of chronic pancreatitis is made via a combination of patient history, the constellation of symptoms, and radiographic findings. Evaluation typically is prompted by a complaint of chronic abdominal pain. Patient history may reveal ethanol use, prior episodes of acute pancreatitis, suspected drug abuse, or a family history or known genetic predisposition. Laboratory evaluation is often not helpful, as patients with chronic pancreatitis can have severe exacerbations with normal serum amylase and lipase levels.
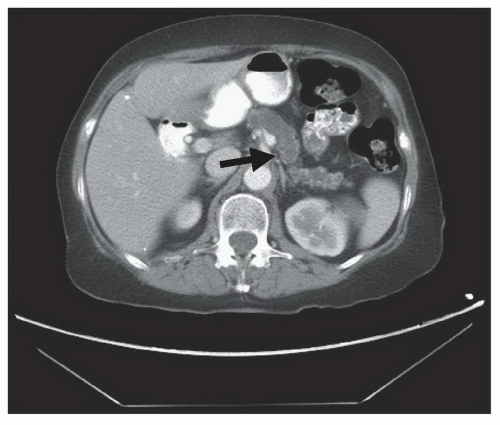
Imaging is a key element in diagnosis. Classically, patients with chronic pancreatitis have dilatation of the pancreatic duct which can be detected on imaging. A “chain of lakes” is often seen from segmental strictures due to the inflammatory process. Calcifications in the pancreatic parenchyma are essentially pathognomonic. The initial imaging study of choice to evaluate the possible diagnosis of chronic pancreatitis is a high quality, multi-detector, contrast enhanced computed tomography (CT) scan (Fig. 11.1). CT is quite accurate for detecting dilatation of the pancreatic duct as well as parenchymal calcifications. With proper contrast enhancement, it also gives an excellent assessment of the pancreatic parenchyma and surrounding vasculature.
When greater resolution of the pancreatic duct is necessary, magnetic resonance cholangiopancreatography (MRCP) provides excellent imaging of the pancreatic duct. Utilizing T2-weighted images, the detailed structure of the pancreatic duct can be seen with high resolution. In our practice, we strongly prefer MRCP over endoscopic retrograde cholangiopancreatography (ERCP), as ERCP, as an invasive procedure, is associated with significant risk of complications, including exacerbation of the pancreatitis. Endoscopic ultrasound (EUS), although not required for most cases, can help evaluate the parenchyma of the pancreas in fine detail, particularly when trying to discern an inflammatory stricture or mass from a subtle neoplasm. In addition, EUS offers the additional advantage of providing a tissue diagnosis via fine needle aspiration when a diagnosis is uncertain from imaging alone.
The treatment of chronic pancreatitis is truly multi-modal and requires cooperation between specialties. Once a diagnosis is made, every effort should be made to identify the etiology of the pancreatitis. If the chronic pancreatitis is due to ethanol abuse, then aggressive steps should be made to assist the patient in ethanol cessation. Simply stopping the consumption of ethanol can lead to improvements in symptoms and decrease the rate of progression of the disease. Similar efforts should be applied toward smoking cessation for patients who abuse tobacco. Metabolic abnormalities that trigger pancreatitis should be treated and any possibly related drugs stopped or changed.
Once triggering factors are removed, treatment focuses on symptom relief. Pain is managed with analgesics and often requires significant doses of narcotics. Collaboration with a chronic pain specialist and careful monitoring of narcotic prescriptions and dosing can help differentiate appropriate management from signs of abuse. Exocrine and endocrine insufficiency is managed with pancreatic enzyme replacement and insulin therapy, respectively. Nutritional support is also initiated when appropriate.
The most common indication to intervene surgically in chronic pancreatitis is unremitting pain that significant interferes with quality of life and cannot be adequately addressed medically. Evidence exists that surgical interventions for chronic pancreatitis can slow the progression of the disease and delay the loss of pancreatic function. However, this in and of itself is not an adequate indication for surgical intervention. Traditionally, it was taught that chronic pancreatitis would “burn itself out” and if surgical intervention was delayed long enough, symptoms would improve. This theory has not held up to scientific scrutiny however, and patients randomized between medical and surgical interventions had significantly less pain over the ensuing 10 years of follow-up if they had undergone surgery. In addition, a recent randomized study comparing endoscopic and surgical interventions for chronic pancreatitis was stopped early due to clear superiority at interim analysis in the surgical arm.
Surgical interventions for chronic pancreatitis can be divided into two broad groups: drainage operations and resectional operations. In 1960, Partington and Rochelle described the side-to-side longitudinal pancreaticojejunostomy that is currently referred to as the Puestow procedure. This procedure remains the standard approach to pancreatic ductal decompression. It is best applied to patients with parenchymal disease and pancreatic ductal dilatation diffusely involving the pancreatic head, neck, body, and tail of the gland. It requires a significant degree of pancreatic ductal dilatation to be technically feasible with a ductal diameter of at least 5 mm.
Segmental pancreatic resection is best applied when parenchymal disease and pancreatic ductal abnormality are primarily confined to one portion of the gland. The same resectional approaches used for neoplasms (pancreaticoduodenectomy, distal pancreatectomy) are utilized as well as total pancreatectomy with islet cell auto-transplant at some centers. When properly applied, these approaches yield acceptable results. Finally, there are also two additional approaches developed more recently that combine aspects of both resectional and drainage approaches. First, the duodenum-preserving pancreatic head resection or Beger procedure addresses the problem of an inflammatory mass in the head of the pancreas. Second, the local resection of the pancreatic head with longitudinal pancreaticojejunostomy or Frey procedure seeks to address the problem that occurs in patients with significant disease in the pancreatic head as well as a “chain of lakes” along the pancreatic duct throughout the body and tail. All of these approaches will be addressed in other chapters of this atlas.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNINGPreoperative planning for a Roux-en-Y longitudinal pancreaticojejunostomy begins with appropriate patient selection. As mentioned, it is best applied to patients with parenchymal disease and ductal dilatation diffusely involving the pancreatic head, neck, body, and tail of the gland. The degree and distribution of ductal dilatation noted on preoperative imaging is key to patient selection. Although there have been reports of
success with lateral pancreaticojejunostomy in patients with small duct disease, this procedure is usually for those patients with a pancreatic duct that measured at least 5 mm in diameter.
success with lateral pancreaticojejunostomy in patients with small duct disease, this procedure is usually for those patients with a pancreatic duct that measured at least 5 mm in diameter.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree