2 Preoperative Evaluation of Patients with Urinary Incontinence and Selection of Appropriate Surgical Procedures for Stress Incontinence
2-1. Discussion of Normal Lower Urinary Tract Function
2-3. Case Study of a Patient with Mixed Urinary Incontinence
2-4. Examination of a Patient with Significant Anterior Vaginal Wall Prolapse
2-5. Case Study of a Patient with Symptomatic Prolapse and Incontinence
2-6. Demonstration of “Eyeball” Filling Study in a Patient with Incontinence and Prolapse
2-7. Q-tip Test in a Patient with Minimal Urethral Mobility
Preoperative Evaluation
The evaluation of a patient with urinary incontinence (UI) is focused on characterizing the incontinence, identifying any concomitant or contributory factors, and determining the patient’s treatment goals and preferences to direct initial treatment decision making and counseling. Essential elements in the initial assessment include a focused medical history and physical examination and basic clinical testing. Additional elements may be necessary if UI is poorly characterized or additional findings suggest a more complicated situation (Video 2-1 ![]() ).
).
History
Evaluation of patients with UI begins with a thorough history and review of the medical record. Elements of the history should be directed toward determining the type of UI (stress urinary incontinence [SUI], urge urinary incontinence [UUI], or mixed incontinence [MUI]) and assessing the duration, frequency, and severity of incontinence episodes; impact of symptoms on lifestyle; and patient expectations of treatment. In addition, the patient should be questioned regarding the presence of other lower urinary tract symptoms and concomitant bowel and pelvic conditions, which may be contributory. Prior treatments for UI, if any, should be reviewed in detail (Videos 2-2 and 2-3 ![]() ). Finally, obstetric, surgical, bowel, and medication histories should be reviewed with the patient to identify any complicating factors or comorbidity that may have an impact on treatment options. Symptoms of other pelvic floor disorders, such as pelvic organ prolapse (POP), defecatory dysfunction, pelvic pain, and sexual dysfunction, should also be sought.
). Finally, obstetric, surgical, bowel, and medication histories should be reviewed with the patient to identify any complicating factors or comorbidity that may have an impact on treatment options. Symptoms of other pelvic floor disorders, such as pelvic organ prolapse (POP), defecatory dysfunction, pelvic pain, and sexual dysfunction, should also be sought.
Questionnaires and Symptom Measurement Tools
Several tools are available for further assessment and quantification of symptoms, severity, and health-related quality of life (QOL) issues. A simple frequency volume chart or bladder diary is generally recommended to document the frequency and volumes of voiding, incontinence episodes, and use of incontinence pads. Patient-reported symptom and QOL questionnaires may be used to assess the patient’s perspective regarding symptoms and effects on QOL. Although many questionnaires are available, the use of high-quality, robustly validated tools is recommended by most professional societies. Commonly used instruments are presented in the Appendix, including Urogenital Distress Inventory-6 (UDI-6), Incontinence Impact Questionnaire-7 (IIQ-7), International Consultation on Incontinence Modular Questionnaire–Short Form (ICIQ-SF), Incontinence Quality of Life Instrument (I-QOL), and American Urological Association Symptom Index (Abrams et al., 2010).
Physical Examination
As part of the initial assessment, a thorough physical examination should be performed with special attention paid to the lower abdomen and pelvis. Components of overall health status include assessment of mental status, obesity (body mass index), and physical dexterity and mobility. Abdominal examination should assess for masses, bladder distention, and relevant surgical scars. Genitourinary examination should include an overall assessment of genital anatomy and neurologic function. The presence of urine leakage from the urethral meatus should be confirmed, if possible, in patients describing SUI symptoms; extraurethral leakage (fistula formation) should always be considered in patients who have had previous surgery or radiation. The vagina should be inspected to assess estrogen status, for concomitant POP, and, if relevant, for the presence of any foreign body or material (Videos 2-4 and 2-5 ![]() ).
).
Cough Test
Provocative testing for SUI can confirm the presence of the sign of SUI and is usually done with a cough or provocative stress test. The cough stress test can be performed with the bladder empty or filled and with the patient supine or standing. For the test, the patient is asked to cough vigorously several times while the examiner observes for urine loss from the meatus. Any leakage of urine with provocation is considered a positive test. Ideally, the bladder is filled up to 300 mL or to a sense of fullness; however, the test can also be performed with an empty bladder. In the supine empty stress test, the patient voids immediately before examination in the lithotomy position and coughs or strains (Valsalva maneuver) while the examiner inspects the urethral meatus. In either the full or the empty test, if leakage does not occur in the supine lithotomy position, the patient repeats the maneuvers in the standing position. Some studies have correlated a positive empty supine stress test with objective urodynamics testing indicative of intrinsic sphincter deficiency (Videos 2-3 and 2-6 ![]() ).
).
Hypermobility
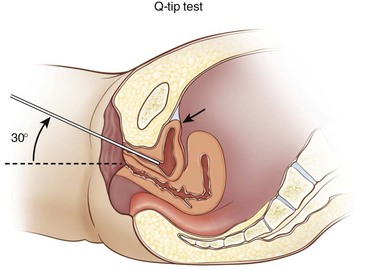
The cotton-tipped swab (Q-tip) test was designed to quantify the degree of hypermobility by measuring the angle of deflection from horizontal of the swab inserted into the urethra during cough or Valsalva maneuver. To perform the test, a swab is inserted per the urethra to the level of the urethrovesical junction, and the angle of the swab compared with horizontal is assessed. Next, the patient coughs or strains, and the change in the angle of the swab is noted. An excursion of 30 degrees or more is a positive test for hypermobility. Although this test is not a diagnostic test, it is an objective measure for quantifying bladder neck mobility during excursion (Video 2-7 ![]() and Figure 2-1).
and Figure 2-1).
Clinical Testing
Pad Testing
1. Test is started without the subject voiding.
2. A preweighed collecting device is put on when the 1-hour test period begins.
3. The subject drinks 500 mL of sodium-free liquid within a short period (maximum 15 minutes), and then sits or rests.
4. At 30 minutes, the subject walks, including stair climbing equivalent to one flight up and down.
5. During the remaining 30 minutes, the subject performs the following activities:
6. At the end of the 1-hour test, the collecting device is removed and weighed.
7. If the test is regarded as representative, the subject voids, and the volume is recorded.
8. Otherwise the test is repeated preferably without voiding.