9 Surgical Management of Voiding Dysfunction and Retention After Stress Incontinence Surgery
Introduction
Transient voiding dysfunction and retention can occur frequently and to a certain degree are expected to occur after certain types of anti-incontinence surgery. It is common for a patient to have retention for days to weeks after a biologic pubovaginal sling or certain suspension procedures. Patients with synthetic sling procedures done in isolation should void immediately postoperatively or shortly thereafter in most cases. Table 9-1 presents reported rates of obstruction after various sling and suspension procedures. When a surgical intervention for iatrogenic voiding dysfunction is believed to be necessary, controversy exists regarding the timing and techniques for these procedures. Preoperative cystourethroscopy should always be performed because the surgeon needs to ensure there is no sling material or sutures within the urethra or the bladder. Also, depending on the clinical situation, urodynamics studies may be helpful in documenting iatrogenic outlet obstruction as the cause for the patient’s symptoms.
Table 9–1 Reported rates of obstruction from various sling procedures
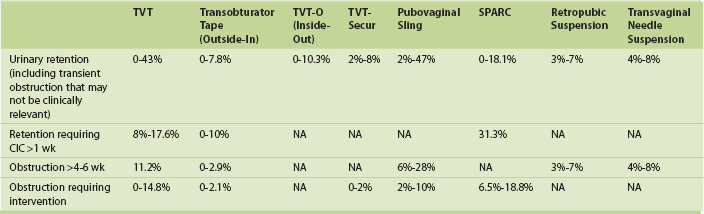
CIC, Clean intermittent catheterization; NA, not available.
From Nitti VW, ed. Vaginal Surgery for the Urologist. Philadelphia: Saunders; 2012.
Technique for Synthetic Sling Loosening in the Acute Setting (7 to 14 Days)
1. The patient is positioned in the lithotomy position, and the vagina is prepared in a sterile fashion.
2. The anterior vaginal wall is infiltrated with local anesthetic.
3. The surgeon cuts the suture used to close the vaginal wall and opens the prior incision.
4. The surgeon identifies the sling and hooks it with a right-angled clamp or other small clamp.
5. The surgeon spreads the clamp or applies downward traction to loosen the tape 1 to 2 cm.
6. The incision is closed with running absorbable suture (Video 9-1 ![]() ).
).






