16
Premature or Rapid Ejaculation: A Neurobiological Approach to Management
Case History
Mr. A.B. is a 42-year-old very successful self-employed businessman who owns three companies. He spent most of his earlier life building his career and had just recently married a 20-year-old secretary in his company. He never had sexual intercourse before he got married. Of late, he has been very depressed, as he is concerned that he cannot please his new wife in the bedroom. He consulted the sexual dysfunction clinic, because he did not get very far with his primary care physician. He insisted that he did not have erectile dysfunction but that he “comes too quick” and that his previous physician had prescribed Viagra, to no avail. He admits to being anxious and depressed, and concerned that his young wife will leave him for a younger man. On examination, the patient appeared anxious and was somewhat shy about this complaint. His vitals included a blood pressure of 146/88mm Hg and heart rate of 90/min. Cardiovascular, respiratory, and abdominal examination was unremarkable. Genitalia examination revealed bilaterally descended testes, phallus length of 4 inches at rest, and no deformities. Prostate examination revealed a normal-size prostate but it was slightly tender. He was assessed for depression using the criteria of the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV). The patient reported sleep difficulties, lack of interest in life, guilt feelings, lack of energy, concentration problems, and a loss of appetite. He was not suicidal. Urinalysis showed some leukocytes, and seminal analysis also revealed some leukocytes as well. Testosterone levels were in the normal range.
Debates About Definitions and Root Causes
Although there is no universal definition of premature ejaculation (PE), this condition remains a real problem in men. PE has also been referred to as rapid ejaculation (RE). This condition is generally underdiagnosed as it depends in part on patients’ self-reporting. Most studies have indicated that men are less forthcoming in reporting sexually related symptoms because of embarrassment. The DSM definition of PE or RE is: “The persistent or recurrent ejaculation with minimal sexual stimulation that occurs sooner than desired, either before or shortly after penetration, and that causes distress to either one or both parties.”
The problem with the definition is that it is subjective. Moreover, there are no large-scale studies to determine normal latency time before ejaculation, and there are no data to determine if the aging process affects this. One author has suggested that the average ejaculatory latency is 3 minutes, and that 30% of women reach orgasm with vaginal intercourse regardless of their partner’s ejaculatory control.1
Central control of ejaculation is from the hypothalamus and the limbic system. In experiments in rats, destruction of the paraventricular nuclei of the hypothalamus has led to significant decreases in seminal emission during ejaculation.2 On the other hand, peripheral control of ejaculation has four components: seminal emission, closure of bladder neck, ejaculation, and orgasm. The condition has gradually been moving from being a strictly psychological phenomenon to one with an associated neurobiological basis in some cases. This is based on findings that men with PE sometimes have different nerve conduction/latencies times.3 Intuitively, one may suspect that PE may be associated with hypertestosteronemia, but studies in men with PE have determined that hormonal differences such as testosterone levels have not been significantly different.4 Suffice it to say that the neuroregulation of sexuality by neurotransmitters has not been well characterized. This is partly because most of the experiments supporting these theories have been based on rat models and are difficult to translate to humans. Overall, dopamine and serotonin appear to be the major transmitters involved in sexuality. In general, dopamine enhances sexual functioning and promotes ejaculation. On the other hand, serotonin tends to decrease sexual functioning by inhibiting ejaculation. Based on these models, several therapeutic models have been suggested and are discussed in this chapter.
| Premature or rapid ejaculation |
| Primary |
| Secondary |
| Delayed or absent ejaculation |
| Anejaculation |
| Retrograde ejaculation |
| Failure of emission |
| Aspermia |
PE, like erectile dysfunction, is becoming more recognized in mainstream medical circles, but it will probably take a breakthrough medication such as Viagra before medical professionals will truly recognize the condition. Table 16–1 summarizes the different ejaculatory disorders that exist in men.
Epidemiological Characteristics
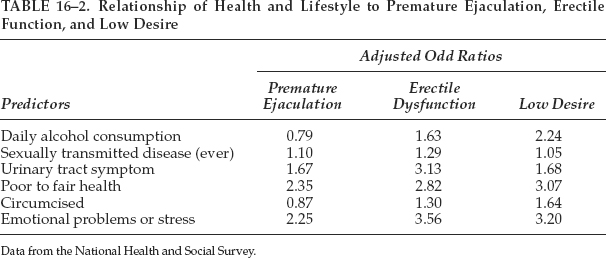
In general, there have been wide variances in the prevalence of this condition, partly because it is a subjective condition, albeit real. The National Health and Social Life Survey estimated that ∼30% of American men suffered from PE. There were slight but no significant differences in reporting rates between the younger (<40 years, 31%) and older (≥40 years, 29.5%) men, which suggests that aging does not seem to influence this condition substantially. The study also suggested that PE might be more common among blacks (34%) as compared with whites (29%). Table 16–2 shows the relationship of health and lifestyle to premature ejaculation, erectile function, and low desire.5
Classification of Premature Ejaculation
Primary Premature Ejaculation
In primary PE, the condition existed because the patient has been sexually active. Primary PE tends to be associated with psychological and psychiatric problems. Psychological problems include relationship distress, psychological distress, guilt, and psychosexual skill deficits. Psychiatric conditions include generalized anxiety state and depression.
Secondary Premature Ejaculation
This usually occurs after a period of normal and satisfactory ejaculation. Medical conditions can lead to secondary PE, but there is often underlying psychological and psychiatric issues as well. For example, a patient suffering from angina may have anxiety about his performance. He may worry that excessive sexual activity may kill him and as such would want to complete the act as soon as possible. As such, his anxiety may lead to a premature ejaculation, which in turn has medical roots, in this case his angina.
In the literature, it has been reported that prostatitis has been associated with PE.6 An Italian study evaluated segmented urine specimens by bacteriological localization studies before and after prostatic massage and expressed prostatic secretion specimens from 46 patients with PE and 30 controls. The incidence of PE in the subjects with chronic prostatitis was evaluated and they found prostatic inflammation in 56.5% and chronic bacterial prostatitis in 47.8% of the subjects with PE, respectively. When compared with the controls, these novel findings were statistically significant (p < .05). The authors suggested that because the prostate gland is responsible in the mechanism of ejaculation that a role for chronic prostate inflammation should be considered in the pathogenesis of some cases of PE. The authors suggested that because chronic prostatitis has been found with a high frequency in men with PE that a careful examination of the prostate be undertaken before any pharmacological or psychosexual therapy for PE.
Data from the National Health and Social Survey.
Pharmacological Treatment of Premature Ejaculation
At present there are no drugs approved by the Food and Drug Administration (FDA) to treat PE. However, clinical trials have evaluated several topical preparations and oral antidepressants. More research is needed in this area, and it is hoped that newer therapies that are well tested will be available in the future.
Topical Treatment of Premature Ejaculation
Lidocaine-Prilocaine Cream 5%
A Turkish group evaluated the efficacy of lidocaine-prilocaine, which could be obtained in the United States via compounding pharmacists.7 In that study, the authors evaluated the efficacy and optimum usage of lidocaine-prilocaine cream 5% in preventing PE. A total of 40 patients were examined in the study group and randomized into four groups of 10 patients. Patients in group 1 applied lidocaine-prilocaine cream 5% for 20 minutes before sexual contact, the patients in group 2 applied it for 30 minutes, and the patients in group 3 applied the cream for 45 minutes, with all patients covering the penis with a condom. Patients in the fourth group applied a base cream as placebo. In group 1, the preejaculation period increased to 6.71 ± 2.54 minutes without any adverse effects. In group 2, although the preejaculation period increased in four patients up to 8.70 ± 1.70 minutes, six patients in this group and all patients in group 3 had erection loss because of numbness. In the placebo group, there was no change in their preejaculation period. The conclusion of that study was that lidocaine-prilocaine cream 5% is effective in PE and that 20 minutes of application before sexual contact is the optimum period. A further study suggested that fluoxetine plus the topical anesthetic was more effective than fluoxetine alone in treating PE.8
SS Cream
This cream is a combination of nine natural products including bufosteroids and plant extracts and was developed in Asia. A Korean group investigated the clinical efficacy of SS cream in a double-blind, randomized, placebo-controlled, phase III clinical study. One hundred and six patients (mean age 38.7 ± 0.61 years) completed the study. A stopwatch measured the ejaculatory latency. Also, the sexual satisfaction ratio of both partner and patient were recorded twice in the screening period and once after each treatment (one placebo treatment of 0.20 g and five SS-cream treatments of 0.20 g for a total of six treatments). Patients were instructed to apply the cream on the glans penis 1 hour before sexual intercourse in a double-blind randomized fashion.
Clinical efficacy was compared with the prolongation of ejaculatory latency and improvement of the sexual satisfaction ratio before and after each treatment. In the screening period, the mean ejaculatory latency was assessed at 1.37 ± 0.12 minutes, and neither the patients nor their partners were satisfied with their sex lives. After treatment, the mean ejaculatory latency was prolonged to 2.45 ± 0.29 minutes in the placebo group and 10.92 ± 0.95 minutes in the SS-cream group. The clinical efficacy of placebo and SS cream as judged by an ejaculatory latency time prolonged more than 2 minutes was 15.09% and 79.81%, respectively. The improvement of sexual satisfaction to a grade higher than effective was 19.81% and 82.19%, respectively, for placebo and SS cream. Of 530 trials of SS cream, 98 (18.49%) resulted in a sense of mild local burning and mild pain. No adverse effect on sexual function or on the partner and no systemic side effects were observed. It was interesting to note that even placebo improved latency in this study, which suggests a strong psychological component in PE. Also, there was a dose-dependent response to SS cream.
Oral Therapy
Oral therapy consists of antidepressants, typically the selective serotonergic reuptake inhibitors (SSRIs). Tricyclic antidepressants such as clomipramine have also been studied.
Selective Serotonergic Reuptake Inhibitors
Of the SSRIs the drug most studied is paroxetine (Paxil). Altogether, there are about five or 10 clinical trials from different countries evaluating the efficacy of Paxil. Different regimens were used in these trials including paroxetine usage on a continued basis or on demand usage. There is no consensus as to which is better, although one study suggested that continued use was better than on demand use in prolonging ejaculatory latency.9 Waldinger and his colleagues10 in 1994 reported one of the earliest studies on the effects of paroxetine on PE. In that small study, 17 male outpatients with PE were randomly assigned to treatment with paroxetine (n = 8) or placebo (n = 9). After a first-week dose of 20 mg/day, the paroxetine regimen was increased to 40 mg/day for 5 weeks. Patients and their female partners were interviewed separately. Patients treated with paroxetine had significantly greater clinical improvement than the patients given placebo.
In another study performed in Israel, sildenafil (Viagra) combined with paroxetine and psychological and behavioral counseling alleviated PE in patients in whom other treatments failed.11 The intravaginal ejaculatory latency time (IVELT) was graded on a scale of to 3 (0 = longer than 5 minutes, 3 = shorter than minute). The 138 men who scored their PE as 4 or greater and IVELT as 2 or greater comprised the study group. Psychological and behavioral counseling was provided during the study. PE was graded using the same scales 3 months after the initiation of each treatment. Topical 5% lidocaine ointment comprised the initial treatment: dissatisfied patients (PE grade 4 or greater, IVELT 2 or greater), took one tablet of paroxetine 20 mg for 30 days and then one tablet 7 hours before intercourse. Sildenafil was added to the treatment of patients dissatisfied with paroxetine alone. The mean initial PE grade was 5.67 ± 0.13 and that for IVELT was 2.9 ± 0.19 for all participants (mean age 28.7 years). Thirty-eight reported improvement (PE grade 2.0 ±0.8, p<.01; IVELT 0.13 ±0.34, p<.001) after local lidocaine application. Of the 100 treated with paroxetine, 42 reported improvement (PE grade 2.5 ± 0.1, p < .01; IVELT 0.28 ± 0.46, p < .001), and 56 of the remaining 58 who were treated with a combination of paroxetine and sildenafil reported improvement (PE grade 1.78 ± 0.23, p < .001; IVELT 0.16 ± 0.37, p < .001). Two patients in the trial remained dissatisfied with all treatment modalities. This reality can be transferred to clinical practice as some patients will remain dissatisfied no matter what happens.
The efficacy of sertraline hydrochloride (Zoloft) for the treatment of premature ejaculation has also been evaluated in an Australian study.1 A total of 37 potent men, 19 to 70 years old (mean age 41), with PE were treated with 50 mg oral sertraline and placebo in a controlled, randomized, single-blind, crossover trial. All men were either married or in a stable relationship, and none of the patients received any formal psychosexual therapy. Chronic open-label treatment with sertraline was continued in 29 patients who had achieved an increase in ejaculatory latency times over pretreatment levels with active drug in the initial crossover study. In an attempt to identify which patients could maintain the improved ejaculatory control after withdrawal of the active drug, serial drug withdrawal was conducted every 4 weeks with drug initiation after a further 2 weeks if improved ejaculatory control was not maintained. The mean pretreatment ejaculatory latency time was 0.3 minute (range 0 to 1). The mean ejaculatory interval after 4 weeks of treatment was 3.2 minutes (range 1 minute to anejaculation) with sertraline and 0.5 minute (range 0 to 1) with placebo (p < .001). Intravaginal ejaculation was achieved for the first time in five patients with primary PE and two patients experienced anejaculation. One patient described minor drowsiness and anorexia, and two patients described mild, transient gastrointestinal upset. Staged drug withdrawal allowed 20 of the 29 patients (69%) on chronic open label treatment with sertraline to discontinue the drug after a mean interval of 7.3 months with a mean ejaculatory latency time of 4.1 minutes (range 1 to 12). This study concluded that sertraline also appears to be a useful agent in the pharmacological treatment of PE.
Tricyclic Antidepressants
Clomipramine (Afranil) is another antidepressant and is in the tricyclic class. It works by inhibiting the membrane pump mechanism responsible for uptake of norepinephrine and serotonin in adrenergic and serotonergic neurons.12 The inhibition of serotonin is probably how the medication aids in PE. The suggested dosage is 50 mg 2 to 12 hours before sexual activity or 50 mg per day continuously. Clomipramine has been evaluated in different clinical trials for ∼20 years. Italian investigators evaluated the effectiveness mechanism of the clomipramine treatment. Investigators measured sacral evoked response (SER) and dorsal nerve somatosensory cortical evoked potential (DN-SEP) testings in 15 patients with true premature ejaculation (TPE). They couldn’t demonstrate any significant difference between the values of either latency times or amplitudes of the evoked responses determined just before and at the end of the treatment with clomipramine in these patients. However, the sensory thresholds were 24.4 ± 4.3 V in the pretreatment term and 30.2 ± 7.3 V at the end of the treatment. This difference was found to be statistically significant (p = .0031). Their results suggest that clomipramine increases the sensory threshold for the stimuli in the genital area.
Role of Nonpharmacological/ Neurobiological Approaches
Behavioral approaches remain important despite recent advances in pharmacology. In some instances, behavioral therapy supersedes medications. The goal of behavioral therapy is to enhance the patient’s awareness of his sensory input and learn how to control it. This could be achieved by relaxation training. For example, the patient could be taught how to control and relax his pubococcygeal muscle by Kegel exercises. Cognitive and behavioral techniques could also be used and the start-stop (squeeze) method is probably the most effective. In this method, the patient squeezes the penis near the time of climax to prevent ejaculation. Combination approaches using both the neurobiological and behavioral methods are often needed to treat patients with PE.
Relapses can be common in patients with PE. They can be prevented by managing the patient’s stress and anxiety by counseling and medications for anxiety such as benzodiazepines. The patient should also practice the squeeze technique during periods of low intercourse frequency.
Discussion of the Case History
Mr. A.B. somewhat typifies the patient profile with PE/RE. These patients generally have some sort of psychological or psychiatric disorder. It is essential to determine whether the depression led to the PE or whether the PE in itself led to depression. Mr. A.B. probably had a strong psychological component because he experienced performance anxiety. He is married to a young woman and may be afraid that he cannot perform adequately. He had coincidental prostatitis, and studies often show that there is an association of prostatitis with PE, but it may not be causative of PE. In any event, he was given a course of ciprofloxacin, which cleared his prostatitis but not the PE. He returned to the clinic for counseling and was also taught the squeeze technique and to practice the start-stop techniques. In view of his depression, he was started on paroxetine (Paxil). This drug has an “off-label” indication for treatment for PE. Three months later, the patient said there was improvement in his PE, but said he might need a little help with his erections. He was then started on Levitra. This case illustrates that PE is a difficult condition to treat and that doctors sometimes confuse PE with erectile dysfunction and prescribe the wrong treatments. Usually a combined approach using both the neurobiological as well as the psychological models can lead to better outcomes. Relapse is common, and this patient will have to be monitored carefully.
Conclusion and Key Points
• PE is very common, and epidemiological studies indicate a prevalence rate of ∼30%. Despite this, very few physicians report encountering this problem, possibly because physicians often do not screen for such problems or are not comfortable in dealing with them.
• There are often overlapping psychiatric or psychological disorders in patients with PE.
• Treatments in the past have been based mainly on a psychological model, but there is increasing evidence for a neurobiological model, wherein drug treatment in combination with psychological methods may be therapeutically useful. Most of the available drugs for treatment are used on an “off-label” basis.
• Patience is required of both the provider and patient in treating this disorder, as it can frequently relapse.
REFERENCES
1. McMahon CG. Treatment of premature ejaculation with sertraline hydrochloride: a single-blind placebo controlled crossover study. J Urol 1998;159:1935–1938
2. Liu YC, Salamone JD, Sachs BD. Impaired sexual response after lesions of the paraventricular nucleus of the hypothalamus in male rats. Behav Neurosci 1997;111:1361–1367
3. Colpi GM, Fanciullacci F, Beretta G. Evoked sacral potentials in subjects with true premature ejaculation. Andrologia 1986; 18:583–586
4. Pirke KM, Kockott G, Aldenhoff J. Pituitary gonadal system function in patients with erectile impotence and premature ejaculation. Arch Sex Behav 1979;8:41–48
5. Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA 1999;281: 537–544
6. Screponi E. Prevalence of chronic prostatitis in men with premature ejaculation. Urology 2001;58:198–202
7. Atikeler MK, Gecit I, Senol FA. Optimum usage of prilocaine-lidocaine cream in premature ejaculation. Andrologia 2002; 34:356–359
8. Atan A, Basar MM, Aydoganli L. Comparison of the efficacy of fluoxetine alone vs. fluoxetine plus local lidocaine ointment in the treatment of premature ejaculation. Arch Esp Urol 2000; 53:856–858
9. McMahon CG, Touma K. Treatment of premature ejaculation with paroxetine hydrochloride as needed: 2 single-blind placebo controlled crossover studies. J Urol 1999;161:1826–1830
10. Waldinger MD, Hengeveld MW, Zwinderman AH. Paroxetine treatment of premature ejaculation: a double-blind, randomized, placebo-controlled study. Am J Psychiatry 1994;151:1377–1379
11. Chen J, Mabjeesh NJ, Matzkin H. Efficacy of sildenafil as adjuvant therapy to selective serotonin reuptake inhibitor in alleviating premature ejaculation. Urology 2003;61:197–200
12. Colpi GM, Fanciullacci F, Aydos K. Effectiveness mechanism of clomipramine by neurophysiological tests in subjects with true premature ejaculation. Andrologia 1991;23:45–47
< div class='tao-gold-member'>