Bryan Williams
Pharmacologic Treatment of Hypertension
Successful lifestyle interventions can delay the development of hypertension (see Chapter 35), but the majority of patients with confirmed hypertension require lifelong drug treatment, usually with more than one drug. This has resulted in a multibillion-dollar industry, in which numerous pharmacologic agents have been introduced (Table 36-1). In turn, this creates complexity for clinicians in trying to decide which drugs would be the most effective option for specific patient groups. The following sections review who should receive pharmacologic treatment, what target blood pressures to attain, and how to decide on what pharmacologic agent to use.
Table 36-1
The development of therapeutic strategies for hypertension.
| Development of Therapeutic Strategies for Hypertension | |
| Year | Nondrug Therapy |
| 1920s | Strict low-sodium diet |
| 1929 | Lumbar sympathectomy |
| 1944 | Kempner rice diet |
| Year | Drug Therapy |
| 1930s | Veratrum alkaloids |
| 1940s | Thiocyanates |
| 1948 | Reserpine, phenoxybenzamine |
| 1950 | Ganglion blockers |
| 1951 | Monoamine oxidase inhibitors |
| 1958 | Thiazide diuretics (chlorothiazide) |
| 1960s | Central α2-receptor agonists, nondihydropyridine calcium channel blockers, and β-blockers |
| 1970s | Angiotensin-converting enzyme (ACE) inhibitors, α1-receptor blockers |
| 1980s | Dihydropyridine calcium channel blockers |
| 1990s | Angiotensin receptor blockers (ARBs) |
| 2000s | Renin inhibitors, angiotensin receptor neprilysin inhibitor (ARNI) |
Defining Who Should Receive Pharmacologic Treatment
Blood pressure (BP) is distributed normally within populations, and thus “hypertension” is an arbitrarily defined, moving target with diagnostic thresholds subject to change as new evidence from clinical trials emerges. From a practical perspective, hypertension is best defined as that level of blood pressure at which treatment to lower blood pressure results in significant clinical benefit. This statement highlights the conundrum in defining hypertension because the risk associated with BP is a continuum, and the BP level at which treatment results in “significant clinical benefit” for any individual will depend on the absolute cardiovascular (CV) risk.1–3 This varies because some people will be more vulnerable than others to end-organ damage at a given level of pressure. Defining that vulnerability case by case remains impractical, and thus differential BP targets and thresholds have emerged that group patients into categories defining their threshold BP for therapeutic intervention and optimal BP goals. In addition, specific drug classes have been given “compelling indications” and “compelling contraindications” for specific groups of patients. This has been useful in tailoring therapy from a wide range of drug classes but has sometimes been misinterpreted as indicating that the specific drug is more important than the achieved BP, which is not the case. The primary objective of therapy must always be to lower BP as effectively as possible.4–6
Blood Pressure Thresholds for Intervention (Office Blood Pressure)
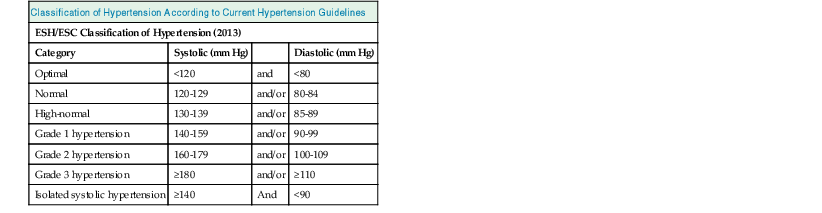
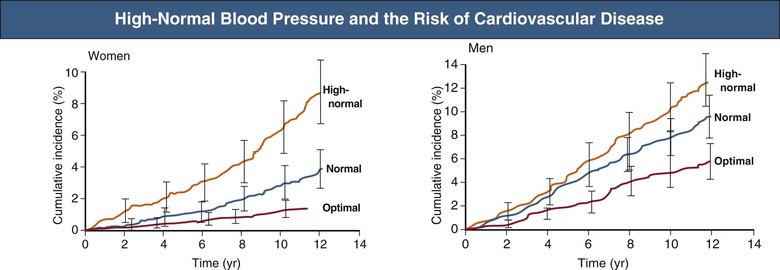
There is substantial evidence that treating a seated “office” BP above a systolic pressure of 160 mm Hg and/or a diastolic pressure above 100 mm Hg reduces cerebrovascular accidents (strokes), myocardial infarction (MI), heart failure, and mortality.4–10 There is also evidence that treating pressures above 140/90 mm Hg, especially in high-risk patients, is beneficial. Consequently, most recent guidelines define hypertension as an office BP of 140/90 mm Hg or higher.7,8 The exception is the recent United States guideline (JNC VIII), which has adopted a treatment threshold of 140/90 mm Hg for adults aged younger than 60 years but recommends a more relaxed threshold for the diagnosis of hypertension (i.e., 150/90 mm Hg in those aged 60 years and older).9 Various grades of hypertension have also been specified (Table 36-2). Previous guidelines from the United States (JNC VII) included a category of prehypertension to highlight those with borderline hypertension.10 This was designed to encourage lifestyle change because the risk of progression from prehypertension to overt hypertension is very high. Furthermore, data from the Framingham heart study have shown that people with a “high normal” BP experience a doubling in risk of CV complications (Fig. 36-1).11 Thus, prehypertension is not benign, and these people are almost certain to develop more severe hypertension without successful lifestyle intervention or drug therapy.
Clinical Dilemma of End-Organ Damage and “Normal” Blood Pressure
There is debate about treatment for people with prehypertension who already have evidence of end-organ damage, such as left ventricular hypertrophy (LVH), or microalbuminuria. This could be an example of the insensitivity of the defined thresholds for diagnosis of hypertension. Clearly, such a patient who has developed hypertensive LVH or microalbuminuria has a BP that is causing damage, but considered below the usual threshold for intervention. Thus, clinical understanding of the disease process is critical to enable the optimal use of guidelines for treatment decisions. There remains considerable uncertainty in the evidence base, and clinical judgment should not, and indeed cannot, be replaced by guidelines.
Blood Pressure Thresholds for Intervention (Ambulatory and Home Blood Pressure Monitoring)
Diagnostic thresholds for hypertension vary according to the method of measurement. Ambulatory blood pressure monitoring (ABPM) and home BP monitoring are increasingly advocated and used. When used to classify hypertension, the diagnostic thresholds are lower. The recent National Institute for Health and Clinical Excellence (NICE) guideline8 in the United Kingdom has recommended the routine use of ABPM to confirm the diagnosis of hypertension because of high rates of white coat and masked hypertension (http://guidance.nice.org.uk/CG127). Table 36-3 summarizes the diagnostic thresholds for hypertension according to different methods of measurement (see also Chapter 33).
Table 36-3
Diagnostic thresholds for hypertension according to different methods of measurement.
| Diagnostic Thresholds for Hypertension | ||
| Place/Time of Measurement* | Blood Pressure (mm Hg) | |
| Systolic | Diastolic | |
| Office or clinic | 140 | 90 |
| 24-hour | 125-130 | 80 |
| Day | 130-135 | 85 |
| Night | 120 | 70 |
| Home | 130-135 | 85 |
* 24-hour, day, and night refer to average blood pressure (BP) measurements in those time periods recorded using ambulatory BP monitoring. Home refers to an average of at least 4 days of seated BP monitoring at home, usually twice daily (i.e., average of ~14 readings).
What are the Blood Pressure Treatment Goals?
An area of great uncertainty has been the definition of the optimal BP treatment goals. As previously discussed, the ideal BP treatment goal is likely to be patient specific, but guidelines must be generalizable to populations. Thus, guidelines should be conservative and pragmatic, should curb the zeal of specialists to advocate ever lower BP goals, and should confine their recommendations to those supported by solid evidence. Until recently, there was international consensus that two BP goals were appropriate: less than 140/90 mm Hg for those with “uncomplicated hypertension” and a lower goal of <130/80 mm Hg for those at higher risk, that is, patients with diabetes, established CV or cerebrovascular disease, or chronic kidney disease (CKD). To define such goals, ideally there should be randomized controlled trials (RCTs) with different groups of patients randomized to different BP treatment targets (i.e., “more versus less” BP control) to determine whether the more aggressive BP target is appropriate and safe. Despite the firm consensus on BP targets previously outlined, no large-scale RCTs have targeted more versus less systolic BP lowering, and only a small number have targeted more versus less diastolic BP lowering.12,13 The guidelines were ahead of the evidence (Fig. 36-2).
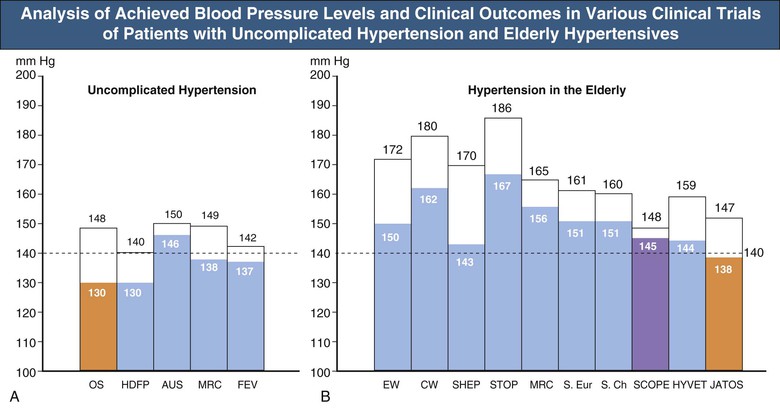
In an attempt to obtain more data with regard to systolic BP lowering, the Cardio-Sis study showed that targeting treatment to a systolic BP of less than 130 mm Hg versus less than 140 mm Hg was more effective at preventing the development of electrocardiographically defined LVH and a composite CV outcome.14 However, this is a single, relatively small study (n = 1111), and insufficient to justify a widespread application of a lower BP target of <130/80 mm Hg. An analysis of the baseline and in-treatment BP levels of patients at high CVD risk in the ONTARGET trial suggests that for people with hypertension at baseline (i.e., systolic BP ≥140 mm Hg), the risk of major CV events and of stroke in particular was reduced with progressive BP lowering.15 However, for those with a systolic BP of 130 mm Hg or less at baseline, there was much less evidence of benefit with further BP lowering and a signal of possible harm. The ACCORD trial tested the more (<120 mm Hg) versus less (<140 mm Hg) systolic BP lowering hypothesis in a high-risk population with type 2 diabetes.16 The study failed to provide conclusive evidence that the more intensive BP treatment strategy reduced a composite of major CV events, although stroke rates were significantly reduced. This study appeared underpowered to test this hypothesis definitively.
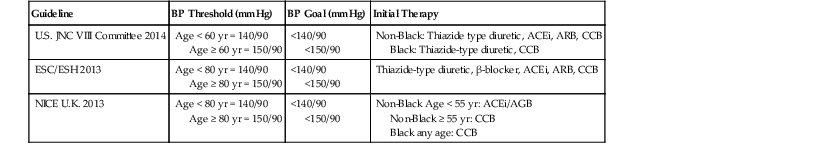
Thus, although previous guidelines have advocated the more aggressive target of less than 130/80 mm Hg for all higher-risk patients, the evidence has always been weak, and more recent studies and analyses have generated concern about a “lower is better for all” approach. As a consequence, recent guidelines have retreated from the “lower is always better” philosophy for BP goals. The European and U.K. NICE guidelines have adopted a single BP goal for most people with treated hypertension (uncomplicated or high risk) of less than 140/90 mm Hg, with a more conservative BP goal of less than 150/90 mm Hg for patients aged 80 years and older, based on the data from the HYVET study.7,8,17 The recent U.S. JNC VIII guideline has adopted a much more conservative approach, consistent with their more conservative aforementioned BP thresholds for intervention. The JNC VIII guideline has recommended a BP goal of <140/90 mm Hg, similar to other guidelines, for those aged younger than 60 years but a BP goal of less than 150/90 mm Hg for those aged 60 years and older, with the caveat being those with diabetes and/or CKD, where a BP goal of <140/90 mm Hg is recommended.9 Thus, the European and NICE BP goals for those aged 60 to 80 years are lower than those recommended for Americans in the same age group, a notable reversal of usual trends. All guidelines acknowledge that lower BP targets may be appropriate for higher risk patients, on a case-by-case basis, depending on the patient’s ability to tolerate lower BP goals, with the caveat that the evidence supporting such a strategy is limited.
Guide to Selection of Antihypertensive Agents
Key Principles from Clinical Trials
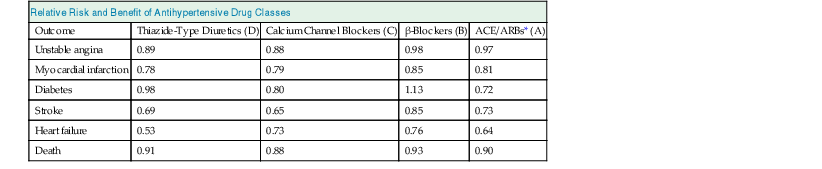
Aside from the limitations of the evidence defining optimal BP treatment targets, the pharmacologic treatment of hypertension has the most impressive evidence base in medicine to guide treatment decisions. BP lowering undoubtedly reduces morbidity and mortality, but nephrologists do not know “how low to go.” Many large RCTs have compared different classes of active treatments with placebo and different treatment strategies with each other (see references 4 to 6 for overviews). Table 36-4 summarizes a detailed systematic review and analysis conducted for the UK NICE hypertension guideline development group in 2006 (http://www.nice.org.uk/CG034guidance), which compared and ranked the effectiveness of different classes of BP-lowering medication with regard to major CV events. The differences between the various drug classes on clinical outcomes are primarily driven by differences in the quality of BP control. Analysis of these trials has provided some important guiding principles with regard to treatment strategies for hypertension, as follows:
Table 36-4
Relative risk and benefit of drugs used to treat hypertension.
Table shows effectiveness of drugs where 1.0 = no benefit/harm, <1.0 = benefit, and >1 = potential harmful effect, from a meta-analysis of major blood pressure–lowering trials conducted for the UK National Institute for Health and Clinical Excellence (NICE) Hypertension Guideline Development Group, 2006.
| Relative Risk and Benefit of Antihypertensive Drug Classes | ||||
| Outcome | Thiazide-Type Diuretics (D) | Calcium Channel Blockers (C) | β-Blockers (B) | ACE/ARBs* (A) |
| Unstable angina | 0.89 | 0.88 | 0.98 | 0.97 |
| Myocardial infarction | 0.78 | 0.79 | 0.85 | 0.81 |
| Diabetes | 0.98 | 0.80 | 1.13 | 0.72 |
| Stroke | 0.69 | 0.65 | 0.85 | 0.73 |
| Heart failure | 0.53 | 0.73 | 0.76 | 0.64 |
| Death | 0.91 | 0.88 | 0.93 | 0.90 |
* Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) were grouped as a single class for the purposes of this analysis.
(Modified from data in http://www.nice.org.uk/CG034guidance.)
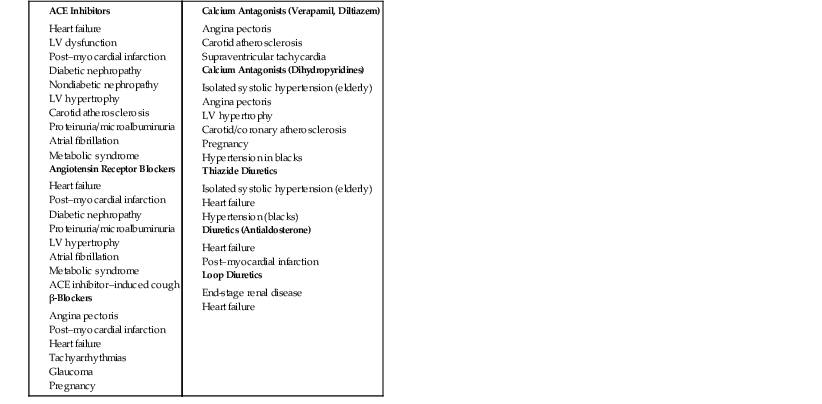
Selection of Drug Therapy
The major classes of BP-lowering therapies are summarized here. International guidelines recommend certain indications and contraindications for the use of specific classes of BP-lowering therapy in specific clinical situations (Box 36-1 and Table 36-5). These lists are not comprehensive and are subject to change as new evidence emerges. Table 36-6 outlines the more common adverse effects associated with the major classes of BP-lowering drug therapies. Figure 36-3 shows the sites of mechanism of action of the various classes of BP-lowering drugs discussed.
Table 36-5
Compelling and possible contraindications to specific classes of BP-lowering therapies.
A-V, Atrioventricular; COPD, chronic obstructive pulmonary disease.
| Contraindications to Specific Blood Pressure–Lowering Therapies | ||
| Pharmacologic Therapy | Contraindications | |
| Compelling | Possible | |
| Thiazide diuretics | Gout | |
| β-Blockers | ||
| Calcium antagonists (dihydropyridines) | ||
| Calcium antagonists (verapamil, diltiazem) | ||
| Angiotensin-converting enzyme inhibitors | ||
| Angiotensin receptor blockers | Get Clinical Tree app for offline access 
| |