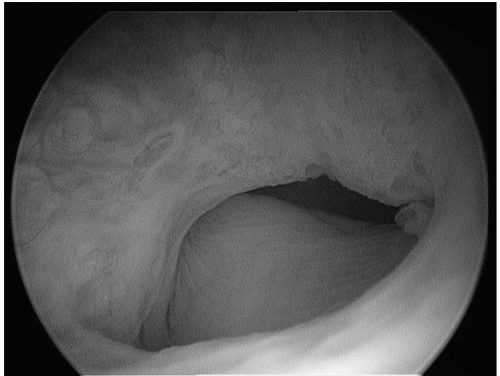
There is controversy regarding the characteristics of patients best treated with bulking agents. In 1992 the term “intrinsic sphincter deficiency” (ISD) was coined to describe patients with a damaged urethral sphincteric mechanism (
Fig. 15.1), regardless of cause (
7). While many, including the author of this chapter, believe the ideal patient for urethral bulking has both limited mobility of the bladder neck and a poorly functioning sphincteric mechanism, others consider that any patient desiring conservative treatment of stress urinary incontinence is a candidate. One of the aspects against use in young patients is that repeat injections of current agents are usually required to maintain effect, and this could mean many injections for such a patient. While some reports indicate equal effectiveness in patients with hypermobility of the bladder neck (
8,
9,
10), others have noted impaired effect in these patients (
11). Medicare guidelines for reimbursement require immobility of the bladder neck (
5). It was not specified as to how immobility was to be determined, but most physicians use a Q-tip test with a straining value of less than 30 to 40 degrees as the cut-off value for hypermobility. Hypermobility has also been determined radiologically by a standing stress test with 2 cm or greater descent of the bladder neck, but there is no indication that imaging provides any more information than the standard Q-tip test. Other techniques include ultrasound and voiding cystourethrography (
12). Medicare still requires a leak point pressure of 100 cm of water or less for reimbursement (
6). The guidelines for this measurement require at least 150 mL of bladder filling, but there is no requirement regarding maximum bladder volume, position of the patient, size of urethral catheter, or kind of effort used to increase the intra-abdominal pressure. Without study confirmation, it is the author’s opinion that the most important pretreatment indication is impaired mobility of the bladder neck. If an anti-incontinence procedure or other
pelvic floor surgery has been performed, and stress incontinence persists or occurs, there is no contraindication to using a bulking agent, and often it is effective. This may be done as early as 6 weeks after surgery.
Generally, bulking agents are not indicated for patients with urethral hypermobility, especially now where there are minimally invasive tension-free slings that have excellent cure rates (see
Chapter 14, Surgical Treatment of Stress Urinary Incontinence). There are situations in high-risk patients where a pessary has provided excellent control of pelvic organ prolapse, and there has been some temporary stabilization of bladder neck mobility. Periurethral bulking has been considered in this patient since when the prolapse is reduced by the pessary, the masking effect of the prolapse on the urethra is removed, and stress incontinence can result. This has not been studied definitively. The result of periurethral bulking after radiation therapy has not been encouraging. Contraindications include active urinary tract infection, high residual urine, severe detrusor overactivity, and reduced bladder capacity (less than 250 mL).