(1)
Department of Surgery Division of Gastrointestinal Surgery, University Hospital Center Zagreb, Zagreb, Croatia
(2)
School of Medicine University of Zagreb, Zagreb, Croatia
Abstract
Despite an increase in the number of effective broad-spectrum antibiotics, pelvic inflammatory disease (PID) and the complications arising from the disease continue to reach epidemic proportions into the 1990s. Acute salpingitis and PID account for more than 350,000 hospital admissions and 150,000 surgical procedures per year [1]. In addition, some report that nearly one-third of patients hospitalized for PID develop some degree of pelvic abscess [2]. Other sequels such as ectopic pregnancy, salpingitis isthmica nodosa, tubal infertility, chronic pelvic pain syndromes, and pelvic adhesions are other consequences of PID. Tubo-ovarian abscess (TOA) is the most serious manifestation of salpingitis because the intra-abdominal rupture of a TOA is potentially life-threatening, with mortality rates as high as 8.6 % [3]. Pelvic inflammatory disease and subsequent TOA may result whenever bacteria gain access to the upper female genital tract. Under normal circumstances, the Fallopian tubes and related pelvic structures are sterile. However, access of bacteria into the upper genital tract either via sexually transmitted diseases or through instrumentation of the uterus may inoculate the uterus with bacteria from the vagina, causing infection. It has been suggested that passive transport and vectors such as spermatozoa and Trichomonas assist in establishing the ascending infection from the polymicrobial vagina and cervix [4]. Once present in the upper genital tract in sufficient numbers and virulence, these bacteria initiate an inflammatory reaction (endometritis-salpingitis-peritonitis) that results in the signs and symptoms of PID. The rate of a TOA developing from typical PID is in the range of 1–4 % [5].
19.1 Considerations in General Female Population
19.1.1 Tubo-ovarian Abscess
Despite an increase in the number of effective broad-spectrum antibiotics, pelvic inflammatory disease (PID) and the complications arising from the disease continue to reach epidemic proportions into the 1990s. Acute salpingitis and PID account for more than 350,000 hospital admissions and 150,000 surgical procedures per year [1]. In addition, some report that nearly one-third of patients hospitalized for PID develop some degree of pelvic abscess [2]. Other sequels such as ectopic pregnancy, salpingitis isthmica nodosa, tubal infertility, chronic pelvic pain syndromes, and pelvic adhesions are other consequences of PID. Tubo-ovarian abscess (TOA) is the most serious manifestation of salpingitis because the intra-abdominal rupture of a TOA is potentially life-threatening, with mortality rates as high as 8.6 % [3]. Pelvic inflammatory disease and subsequent TOA may result whenever bacteria gain access to the upper female genital tract. Under normal circumstances, the Fallopian tubes and related pelvic structures are sterile. However, access of bacteria into the upper genital tract either via sexually transmitted diseases or through instrumentation of the uterus may inoculate the uterus with bacteria from the vagina, causing infection. It has been suggested that passive transport and vectors such as spermatozoa and Trichomonas assist in establishing the ascending infection from the polymicrobial vagina and cervix [4]. Once present in the upper genital tract in sufficient numbers and virulence, these bacteria initiate an inflammatory reaction (endometritis-salpingitis-peritonitis) that results in the signs and symptoms of PID. The rate of a TOA developing from typical PID is in the range of 1–4 % [5].
TOA is usually a polymicrobial infection, whereas general pelvic infections may often be monomicrobial. Tubo-ovarian abscesses are usually a mixture of anaerobic, facultative anaerobic, and aerobic organisms, with the purest isolated generally being anaerobes. The most frequent isolates from TOAs include a variety of Enterobacteriaceae, such as Escherichia coli (37 %), Bacteroides fragilis (22 %), other Bacteroides species (26 %), Peptostreptococcus (18 %), and Peptococcus (11 %) [3, 6].
The sexually transmitted organisms such as Neisseria gonorrhoeae and Chlamydia are usually not present in the abscess but may be recovered from the cervix in one-third of cases. The emergence and recognition of Prevotella bivia (formerly Bacteroides bivius) and Prevotella disiens as major pathogens in upper female genital tract infection, combined with data suggesting that increased concentration of anaerobic organisms in the vagina is a risk factor for PID, point toward an anaerobic-predominant mixed infection as a cause of PID and TOA. These anaerobic bacteria such as Bacteroides species and Peptostreptococcus species are commonly found in high concentrations in the vagina of women with bacterial vaginosis [4].
Standardized diagnostic criteria for TOA do not exist. The clinical diagnosis of TOA has the same diagnostic difficulties of PID. Women presenting with PID and a pelvic mass may have a TOA, or it could be a hydrosalpinx, tubo-ovarian complex, or other complex adnexal mass. Patients with TOAs typically present with a history of pelvic or abdominal pain and fever. A history of PID may be present in only 50 % of patients. The majority of patients also have a leukocytosis [2]. A significant proportion of women with TOA is afebrile (20–30 %) and has normal WBC counts [2]. Other laboratory studies that may help in the diagnosis are an elevated erythrocyte sedimentation rate (ESR) and elevated C-reactive protein (CRP), which was found to be more sensitive than elevated WBC or ESR. Pelvic examination usually reveals extreme pelvic tenderness (cervical motion tenderness), and a mass may be present. If rupture has occurred, typical signs and symptoms of peritonitis are present and may lead to shock and death if not treated immediately. Ultrasonography is very helpful in the diagnosis of TOAs and in following TOAs that are managed conservatively. Ultrasonography has proven to be very reliable in the diagnosis of TOA [6]. The expected typical appearance of a TOA on ultrasonography is a complex or cystic adnexal mass with multiple internal echoes and septations. The “gold standard” for diagnosis has always been laparoscopy; however, as ultrasound technology continues to improve, laparoscopy may be reserved for patients in whom the diagnosis is questionable.
Indications for surgical intervention in the treatment of TOA include:
Questionable diagnosis, when another surgical emergency may exist
Rupture of abscess
Failure of medical therapy with or without a drainage procedure
The first two are indications for immediate surgical intervention. Intraperitoneal rupture of a TOA represents a true surgical emergency. Delayed interventions may increase the risk of septic shock and even death. There is general agreement that acute rupture of a TOA requires immediate surgery, but the extent of the surgery required to achieve a cure is controversial [6, 7]. Traditionally, aggressive surgical extirpation, usually consisting of total abdominal hysterectomy with bilateral salpingo-oophorectomy (TAH-BSO) and drainage of all pockets of infection, was the treatment of choice in TOAs. This radical approach was used largely because of the inadequacies of antibiotics of that time. This procedure dropped the mortality rate from 100 to 12 % [8] and is probably the procedure of choice in a patient who has completed childbearing or in those who are postmenopausal. However, most women who present with a TOA are in the peak of their reproductive years, and fertility is a major issue. Conservative therapy of an unruptured TOA consists of appropriate intravenous antibiotic therapy, close monitoring of the patient, and possible drainage of the abscess via posterior colpotomy [9, 10], CT- or ultrasound-guided percutaneous drainage, or drainage via laparoscopy. The posterior colpotomy approach has largely been abandoned because of a high rate of complications, including peritoneal sepsis and death. Success rates of CT-guided percutaneous drainage have been in the range of 77–94 %, and this technique may play more of a major role in the future [11]. Early drainage of abscess and irrigation via laparoscopy in addition to antibiotics achieved a success rate of 95 % by Reich and McGlynn’s series of 21 patients [12]. These latter approaches have shown initially promising results but still need to be studied prospectively in a controlled randomized fashion. It does appear that drainage of a TOA in combination with antibiotic therapy is much more successful than conservative management. It has been shown that 50 % of patients treated with antibiotics alone eventually require surgical treatment for the disease [2, 13]. Others report a success rate of 70 % when TOAs are treated with antibiotics alone [4].
Approximately 19 % of patients treated with conservative surgical therapy require reoperation at a later date [2, 13, 14]. In cases of grossly apparent bilateral disease, a somewhat conservative approach of bilateral partial adnexectomy without hysterectomy may be performed. Patients without adnexa are still able to conceive via in vitro fertilization and donor eggs. One must always use clinical judgment, however, and in patients with severe pelvic disease, TAH-BSO may be necessary despite the patient’s reproductive status. In patients who have completed childbearing, TAH-BSO is standard therapy. It should also be noted that when a TOA is present in a postmenopausal woman, associated underlying malignancies are found in 25–50 % of cases, and conservative surgical therapy has no role [15]. Antibiotic therapy should include a broad-spectrum cephalosporin such as cefoxitin or cefotetan. Anaerobic coverage with clindamycin or metronidazole should also be added, as these have been shown to have the best ability to penetrate an abscess [6].
19.1.2 Ovarian Abscess
Ovarian abscess is a primary infection of the parenchyma of the ovary, an entity distinctly different from tubo-ovarian abscess. Tubo-ovarian abscess, by contrast, involves the ovary by secondary spread from the infected Fallopian tube [16]. Ascending infection is the most important mode of infection in nonpregnant women. Cases of ovarian abscess have also been reported due to non-gynecologic conditions such as ruptured appendicitis or diverticulitis or secondary to infection at distant sites as in tonsillitis, typhoid, parotitis, and tuberculosis. Association of ovarian abscess with intrauterine device (IUD) has been noted, and some of them may be secondary to Actinomyces spp. It may also occur due to secondary infection in a dermoid cyst, serous cystadenoma, or simple ovarian cyst. Ovarian abscess is also a known complication of transvaginal oocyte retrieval or transcervical embryo transfer, occurring in approximately 0.2–2.2 % [17]. Aitken is attributed to give the earliest description of primary ovarian abscess in 1869 [18, 19] and then Coe in 1891 [20]. Black presented the first major series of 42 cases in 1936. Wetchler and Dunn have reported 120 cases in literature till 1985 [16].
19.2 Incidence
19.2.1 Tubo-ovarian Abscess
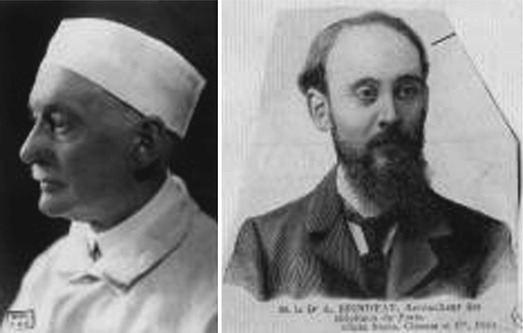
Pelvic inflammatory disease in the form of pelvic and peritoneal abscess complicating pregnancy is rare. Blanchard et al. found that acute salpingo-oophoritis during pregnancy occurs more commonly in first trimester [21]. Sherer et al. have reported a recurrent pelvic abscess in pregnancy and in their review noted that the pelvic infection and pelvic abscess are less common in the second and third trimesters than in cases diagnosed in the first trimester [22]. By 1977, only 12 cases of tubo-ovarian abscess occurring late in pregnancy had been described in the literature [23]. Auguste Brindeau (Fig. 19.1) in 1917 is thought to have described the first such case [23]. In addition to 12 personal cases of salpingo-oophoritis during pregnancy, he has collected 81 more cases, of these 44 were operated on. There are several newer cases in late pregnancy [24, 25]. On the other hand, pelvic infection readily occurs in the puerperium if there is infection of the birth canal during or following parturition.
Up to 2003, there were only 26 reported cases of tubo-ovarian or pelvic abscess during pregnancy published [27]. The incidence of PID after oocyte retrieval is 0.12 % [28]. Pelvic infection after transvaginal oocyte retrieval for IVF-ET is <1 % [17, 29–31]. In less than half of these cases, a pelvic abscess develops.
19.2.2 Ovarian Abscess
19.2.3 Intramyometrial Abscess
This entity is not described as part of PID, but it is mentioned here due to the same possible etiological factor. It is the rarest entity. Only one report with two cases was found [34].
19.3 Etiopathogenesis
19.3.1 Tubo-ovarian Abscess
During pregnancy, pelvic infection occurs quite independent of the gravid state or the infection may exist before the pregnancy. The etiologies may include non-gynecologic conditions such as ruptured diverticulitis or appendicitis; tubo-ovarian abscess of unknown origin has also been reported [35]. Friedman and Bobrow have proposed four mechanisms for infection of the ovaries or tubo-ovarian abscess during pregnancy [36]:
Hematogenous spread as in pelvic tuberculosis
Lymphatic spread especially from vagina and cervix
Infection of a previously existing ovarian cyst
Flare-up of old infection
Similar mechanisms are described by Merzer [37]:
Infection at the time of fertilization
Infection soon after fertilization before the uterine cavity has become closed by conception (12 weeks)
Vascular or lymphatic spread (from a septic focus in the vagina or cervix)
Flare-up of preexisting infection
Instrumentation sufficient to overcome natural barriers
Ascending infection associated with threatened abortion and intrauterine bleeding
Pelvic inflammatory disease, previous laparotomy, structural genital anomalies, and IVF-ET are known risk factors for pelvic abscess during pregnancy [27].
Why some tubo-ovarian abscesses are unilateral may be explained by a “flare-up” of an already preexisting but latent salpingitis [24]. This possibility would seem to necessitate either a low-grade infection of the tube in the first instance leaving sufficient patency to permit the passage of a fertilized ovum. After nidation, the infection may then become acute probably because of the congestion produced by the gestation or unilateral salpingitis, the other tube being patent and functioning [38].
19.3.1.1 In Vitro Fertilization-Embryo Transfer
Pelvic abscess formation is a rare complication of oocyte retrieval, which usually results in failure of the procedure. It is reported to occur in 0.2–0.5 % of transvaginal oocyte retrievals [17, 39]. Inoculation of vaginal bacteria and anaerobe opportunists is suggested to be the cause of PID following oocyte retrieval [30]. Microorganisms of the vagina are suggested to be the etiological pathogens in pelvic abscesses when transvaginal oocyte retrieval is used [30]. El-Shawarby et al. in 2004 described three different pathways for such infections. Direct inoculation of vaginal microorganisms may occur by puncture through the non-sterile vagina. The risk of pelvic infections after oocyte retrievals seems also related to the history of pelvic inflammatory disease. Reinfection may occur through puncture of chronically infected ovaries [40]. Although least likely, infection may occur through direct puncture of the bowel with an inflammatory or infectious spillage [41]. However, no pelvic infection has been reported with laparoscopic or abdominal oocyte retrievals in the 1990s [30].
The most well-established and well-accepted technique to decrease the risk of pelvic infection is using the fewest possible vaginal punctures [39, 42]. Serour et al. emphasized the importance of the fact that most patients in their study had a maximum of only two vaginal punctures [42]. Vaginal preparation has been made by different methods including the use of saline or povidone-iodine. In reports by Meldrum [43] and Evers et al. [44], no cases of PID in small group of patients were diagnosed. The former study used intravenous cefazolin and vaginal irrigation with povidone-iodine and the latter using only 10 % povidone-iodine. Larger series report rare cases of serious infections using sterile saline (0.5 %) [45] and Earle’s balanced salt solution (0.4 %) [39].
19.3.1.2 In Vitro Fertilization-Embryo Transfer and Endometriosis
IVF-ET is now a recognized treatment for refractory endometriosis-associated infertility. On the other hand, endometriosis is proposed to be a risk factor for pelvic inflammation and abscess development following transvaginal oocyte retrievals [46, 47]. The presence of old blood in endometrioma is suggested to provide a culture medium for bacteria to grow slowly after transvaginal inoculation which may explain the role of endometriosis in predisposing the patients with PID [46]. Among its risk factors, incidental aspiration of an ovarian endometrioma during the process of oocyte retrieval is believed to be a common cause for developing the pelvic infection [46, 48, 49]. In one study 80 % (8/10) of PID following oocyte retrieval had underlying endometriosis [28].
There have been some case reports on the coexistence of endometriosis [46, 48] or its history [47] in patients with PID following assisted reproductive technology treatment. Younis et al. [46] presented three cases of severe pelvic abscess following oocyte retrievals for IVF-ET in whom stage IV endometriosis or ovarian endometrioma was previously diagnosed as the sole reason for infertility. In contrast, Ashkenazi et al. [17] failed to show a higher incidence of endometriosis among their patients: two cases of endometriosis in 28 PID patients among 4,771 ovum pickups. It has been suggested that both the pseudocapsule of endometrioma and its inside old blood may prevent antibiotic prophylaxis from overcoming the transvaginal bacterial inoculation [46]. In other cases of endometriosis, small pools of old blood may act as culture media for the inoculated bacteria. Deposit of TOA is an uncommon complication in pregnant women, leading to serious complications such as surgery, ICU admission, and preterm delivery; only one subject developed a TOA during pregnancy following IVF-ET in this report.
The presence of endometrioma is a risk factor for the development of a TOA or an ovarian abscess [50]. Whether operative treatment of recurrent ovarian endometriosis improves the prognosis of IVF is still open to debate [51]. Previous reports have indicated that aspiration of endometriotic cysts before ovulation induction for in vitro fertilization resulted in a better clinical outcome [52]. However, studies have also indicated that pretreatment for endometrioma before IVF could potentially reduce the number of retrieved oocytes [53]. In order to prevent infection in patients with endometrioma for oocyte retrieval, previous reports have suggested the aspiration of endometrioma before oocyte retrieval [53]. However, Tsai et al. found these endometriotic cysts re-expanded quickly after aspiration and it was difficult to harvest some oocytes without puncturing through these chocolate cysts. In addition, the chocolate content of the follicular fluid is sometimes found incidentally after the aspiration [54]. Since endometrioma was considered a risk factor for the development of a TOA or an ovarian abscess [50], infection-preventing measures should be applied not only prior to but also immediately before oocyte retrievals.
19.3.1.3 Pelvic Inflammatory Disease
19.3.1.4 Postpartum
The postpartum period appears to be the least likely time to develop a TOA because ascending infection, which is the major pathophysiology in developing PID in most women, rarely occurs during this phase.
19.3.1.5 Tubal Sterilization
Particularly in women who have had tubal sterilization, the incidence of TOA is minimal because the procedure blocks communication between the genital tract and the pelvic cavity [55]. Theoretically, this blockage should prevent an ascending transmission of any organisms, if present, from the genital tract proximal to the site of tubal sterilization into the peritoneal cavity. This view is supported by clinical evidence that a complete or even partial occlusion of tubes appears to lessen the severity of infection when it occurs [55]. Three possible explanations of TOA after previous occluded tubes (TOAPOT) have been proposed [55]. The most likely cause is the persistent tract or reconnection between the two tubal segments. Secondly, factors related to the operative procedure are possible. Lastly, systemic factors such as a hematogenous or lymphatic bacterial spread with a compromised immunological status of the patient are possible. Time intervals from tubal occlusion to TOAPOT had been reported to range from as early as 36 h to up to 12 years [55].
19.3.2 Ovarian Abscess
The etiology of ovarian abscess in pregnancy is uncertain and in all probability is different from that in nonpregnant state. Ascending infection is the most important mode of infection in nonpregnant women. Barriers to ascending infection in pregnancy include cervical mucus plug, intact fetal membranes, and the decidua covering the openings of the Fallopian tubes. Friedman and Bobrow [36] have proposed four mechanisms for infection of ovaries during pregnancy (see section Tubo-ovarian Abscess). Data that confirm these facts are that ovarian abscess readily occurs in the puerperium if there is infection of the birth canal during or following parturition. Also it is likely that the ovary becomes infected quite independently of the gravid state or that the infection exists before the pregnancy.
19.3.3 Intramyometrial Abscess
The etiology in one published report of two cases is failed instrumental delivery in the second stage of labor [34].
19.4 Microbiology
Up to 2003, in only several cases, bacterial etiology of pelvic infections is available after transvaginal punctures such as E. coli [56] and a subclinical infection with C. trachomatis [57] and rare isolate in general population Atopobium vaginae [58], S. aureus, and mixed anaerobic bacteria [47]. Anaerobic opportunists of the vagina are found to be etiological agents in pelvic abscesses after transvaginal oocyte retrieval. Escherichia coli, Bacteroides fragilis, Enterococcus, and Peptococcus are commonly found microorganisms [30, 31]. There are also case reports with other microorganisms such as Fusobacterium necrophorum during puerperium [59]. In a case by Navada and Bhat, at laparotomy there was no clear-cut evidence of spread of infection from adjacent organs, but the preexisting salpingitis or previously ruptured tubo-ovarian abscess could not be ruled out. Thus, the proposed mechanism in the case by Navada and Bhat could be flared up of old infection [60]. Intraoperative finding of adhesion between the loops of intestine, the uterus, and the tubo-ovarian tissue indicates the chronic nature of the disease. Hence, she might have contracted the pelvic infection before pregnancy following the first Cesarean section.
Patients who suffer from ovarian abscesses almost always have a history of salpingitis, endometriosis, pelvic adhesion, hydrosalpinx, or pelvic surgery [30, 46].
19.4.1 Ovarian Abscess
An ovarian abscess is defined as a primary infection of the ovary without the involvement of the Fallopian tube, whereas a tubo-ovarian abscess involves both the Fallopian tube and the ovary. Since 1869, only 125 cases of primary ovarian abscesses have been reported in the related English literature. Wetchler and Dunn reviewed 120 cases up to 1985, [16] and Stubblefield in 1991 added five cases [61]. The possible factors for the cause of ovarian abscess are disruption of the ovarian capsule, giving bacteria access to the ovarian stroma, and hematogenous and lymphatic spread [16]. Nevertheless, the most common mechanism is considered to be alteration of the ovarian capsule at the time of ovulation or by penetration during surgery or surgical procedures. The interval between capsule disruption and clinical presentation may vary, depending on the bacterial inoculum dose, type of bacterium, its virulence and whether the infection occurred secondary to a direct contamination at surgery, or spread through devitalized tissue [62]. The aforementioned complication has been reported to occur after vaginal hysterectomy, ovarian cystectomy, Cesarean section, during pregnancy, and with the use of an intrauterine device [16, 63].
Furthermore, transvaginal or percutaneous needle aspiration of an endometrioma has been considered in the causation of this rare phenomenon [48, 64]. Ultrasonically guided vaginal oocyte collection is a relatively atraumatic method with rare complications. This technique has now become the method of choice in most IVF-ET programs, because it results in excellent oocyte yields, with increased speed and excellent follicle, as well as major pelvic vessel visualization, thereby decreasing the probability of vessel puncture [65]. Nevertheless, despite the advantages, there are some inherent risks, such as injury to blood vessels and hemoperitoneum, trauma to pelvic organs, infection or exacerbation of pelvic inflammatory disease, rupture of endometriotic cystic masses, urinary tract infections, and hyperstimulation [31, 66–68]. Reports on the formation of an ovarian abscess after ovum retrieval for IVF are scant [48]. Moreover, the case reported by Padilla in 1993 occurred during ovum retrieval while an endometriotic cyst was punctured [48], thus making the case by Dicker et al. of ovarian abscess to occur after follicle aspiration without any subtle pelvic pathology [31].
19.5 Clinical Presentation
19.5.1 Tubo-ovarian Abscess
Pregnancy is said to protect against pelvic infections. Clinicians are therefore unlikely to suspect a pelvic abscess as a cause of an acute abdomen in pregnancy. The first signs of the disease are sometimes mild and not specific [46]. Recurrent symptoms of abdominal pain in the postoperative period and interpregnancy period suggest the chronic nature of the disease. However, the courses of antibiotics and the low virulence of the organisms resulted in chronic pelvic infection. The infection might have flared up recently and presented in the third trimester of pregnancy with some acute symptoms like abdominal pain with giddiness and vomiting to suggest peritonitis. Patients with PID during pregnancy may present with wide range of clinical symptoms, and the findings may be altered significantly by the size of the gravid uterus [22]. With no classical clinical features of acute peritoneal or pelvic infection, it was not suspected preoperatively and was detected only during Cesarean section [69]. Jafari et al. in the English literature review of 19 cases found that in only one case, the diagnosis was made preoperatively [23].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree