Fig. 20.1
Conversion rate of laparoscopic colorectal surgery by type of previous operation. Figure represents data from Franko et al. [11]; 820 patients were evaluated. * represents conversion rates that were significantly different from patients without prior surgery by Pearson’s chi-squared test. With permission from Franko J, O’Connell BG, Mehall JR, Harper SG, Nejman JH, Zebley DM, et al. The influence of prior abdominal operations on conversion and complication rates in laparoscopic colorectal surgery. JSLS: Journal of the Society of Laparoendoscopic Surgeons 2006;10(2):169-75 © Society of Laparoendoscopic Surgeons 2006 [11]
When considering specific metrics, the rate of enterotomy varies between studies, with Binenbaum et al. [12] reporting a rate of nearly 0.6 %. A systematic review by van der Voort and colleagues [13] found a smaller incidence of intestinal injury during laparoscopy (0.13 %); however, nearly 70 % of intestinal injuries were associated with adhesions or prior abdominal surgery. In laparoscopic cases dedicated exclusively to lysis of adhesions, enterotomy rates have been reported between 3 % and 17 % [14]. Although a rare complication in most studies, accidental enterotomy can have disastrous consequences, with mortality rates of greater than 3.5 % in these cases [13]. Mortality rates increase to between 20 % and 50 % if the enterotomy is not recognized at the time of surgery [15, 16].
Adhesions are thought to occur almost universally after transperitoneal surgery. The density of adhesions and the clinical ramifications appear to worsen with the number of previous surgeries [17] and other inflammatory processes, such as bowel injury, intra-abdominal abscess, locally advanced cancer, or IBD. While the potential for dense adhesive disease in reoperative patients poses an additional challenge for the minimally invasive surgeon, it increases the degree of difficulty rather than creating a unique set of problems. We feel that laparoscopic surgery can be performed safely and efficiently when adequately trained surgeons follow basic steps (Table 20.1) and maintain a low threshold for conversion to an open approach in especially complex cases.
Table 20.1
Steps in the reoperative minimally invasive colorectal case
1. Abdominal entry |
• Initial transperitoneal entry |
• Insufflation and inspection |
• Safe placement of ports for Step 2 |
2. Anterior abdominal wall clearance |
• Adhesiolysis of abdominal wall |
• Optimal placement of ports for Step 3 |
3. Dissection and isolation |
• Adhesiolysis, mobilization, and isolation of structures for Step 4 |
4. Resection and reconstruction |
When thinking about the reoperative laparoscopic case, it helps to break the procedure down into steps. These smaller components help to concentrate the surgeon on immediate goals, and each step is focused on setting the surgeon up for success in the following step. Gaining safe entry into the abdominal cavity is the first step. The goal of this step is the safe placement of adequate ports to continue adhesiolysis of the anterior abdominal wall. The first step involves initial port placement, insufflation, visual examination, and finally the safe placement of additional ports. The second step is a focused adhesiolysis. The goal of the second step is not a complete takedown of all intra-abdominal adhesions. Rather, this is an abdominal wall adhesiolysis for optimal placement of ports in order to continue the dissection and isolation of the structures of interest. Once ideal port placement has been achieved, the surgeon can begin the third step—dissecting out the structures needed to complete the case. Mobilization and isolation of these structures is key in setting up the resection and reconstruction, the final step of the procedure. Having a clear understanding of the anatomy prior to commencing a difficult dissection is critical as this will help frame the procedure and increase one’s understanding of the anatomy as the dissection progresses.
In this chapter, we will examine the challenges involved in minimally invasive colorectal surgery for reoperative patients and focus on preoperative, operative, and postoperative strategies to minimize complications and achieve optimal outcomes despite the added difficulty posed by these cases.
General Considerations
As with any surgery, appropriate patient selection is the key to achieving optimal outcomes. While most of the considerations for laparoscopic surgery in the reoperative patient are identical to those for any patient undergoing laparoscopic surgery, the reoperative patient may require additional attention centered around the potential for adhesions. In patients with a significant amount of expected adhesions, two differences between them and typical patients should be considered. First, the risk of injury during entry into the abdominal cavity may be increased compared to typical patients. This additional level of risk may alter the risk-benefit ratio of a given case and tip the scales in favor of nonoperative management (when appropriate) or open surgery.
In addition, laparoscopic adhesiolysis may be a significant portion or even the majority of a complex reoperation. Studies of open surgery have indicated that abdominal entry and time for adhesiolysis in reoperative surgery can extend the range of operative times by 20 min to several hours [18]. Although data examining operative time for abdominal entry and adhesiolysis in laparoscopic reoperation is lacking, the potential for extended times in laparoscopy is likely even greater than in open surgery. The additional time involved for this aspect of the case should be considered, and cases should be scheduled for extended blocks to avoid time constraints in the operating room (OR). Patients potentially unable to tolerate the increased fluid shifts and stress of prolonged anesthesia due to added length of surgery should be considered for an open procedure or nonoperative management.
While the emergent status of an operation is generally a contraindication for laparoscopic surgery, urgent operations are often performed laparoscopically. Even in cases considered to have a low likelihood of laparoscopic completion, practitioners feeling comfortable with laparoscopic entry find little disadvantage to starting an operation with a diagnostic laparoscopy. With a low threshold for conversion to an open procedure in the urgent setting, diagnostic laparoscopy adds little time to the procedure and may provide important visualization for diagnosis or surgical planning. In some cases, a procedure may be completed with the minimally invasive technique, sparing the patient the larger incision and associated complications. The reader is referred to Dr. Haas’ excellent review of the use of a laparoscopic approach for colorectal disease in the emergent setting in Chap. 27.
Preoperative Evaluation
Preoperative evaluation in the reoperative patient differs from the evaluation of other patients preparing for surgery due to the focus on the past surgical history. While considerations of the patient’s disease and indicated procedure are important, the patient’s surgery may be dominated by aspects related to his previous surgeries. The patient’s surgical history should be thoroughly reviewed, with attention paid to the number and types of previous operations and resultant anatomy. Furthermore, especially in Crohn’s patients, consideration should be given to determining the length of residual bowel to avoid a short bowel syndrome. Abdominal complications such as mesh placement, intra-abdominal abscesses, fistulas, bowel injuries, and other inflammatory processes that may lead to increased abdominal adhesions should be directly questioned.
A visual inspection of the abdomen may reveal scars from previous surgeries that the patient forgot or considered unimportant (Fig. 20.2). They can also be more significant and should cause reconsideration regarding whether or not you should undertake a minimally invasive approach (Fig. 20.3). These scars may also provide a road map of locations to avoid during entry, as adhesions to previous incisions or trocar sites will increase the risk of bowel injury. If possible, previous operative notes should be reviewed to help identify potential areas of dense adhesive disease to be avoided during laparoscopic entry. Areas of potential adhesion may also determine port placement, as lysis of adhesions may be the most difficult portion of the case, requiring the addition of dedicated ports.



Fig. 20.2
Abdomen demonstrating subtle previous scars throughout

Fig. 20.3
“Hostile” abdomen suggesting that a minimally invasive approach may be contraindicated. Courtesy of Brad Davis, MD, with permission
Indicated imaging, such as a barium enema to establish anastomotic patency or colonic anatomy for stoma reversal, should be performed in accordance with usual practice for any surgery. A computed tomography (CT) scan may be of additional aid in determining the potential site of adhesion in obstructive disease, and areas of the abdomen with especially dilated loops may be avoided during laparoscopic entry. In general, however, dilated loops of the bowel are not static, and minimal reliance can be placed on preoperative imaging in this regard.
Although not regularly practiced at our institution, several reports in the literature have indicated the utility of preoperative ultrasonic or cine-MRI evaluation of abdominal wall adhesions to minimize injury during laparoscopic entry into the abdominal cavity (Fig. 20.4) [19–21]. These techniques use spontaneous and induced visceral slide to detect loops of bowel or other organs adhered to the anterior abdominal wall. While these techniques have shown excellent correlation to intraoperative findings, they have not been tested for improvement in clinical outcomes and their widespread application in the non-research setting is unclear. Finally, determining both the date and results of a previous colonoscopy can be useful to avoid missing pathology or making intraoperative decisions such as the need for an en bloc resection, diversion, or intraoperative endoscopy.
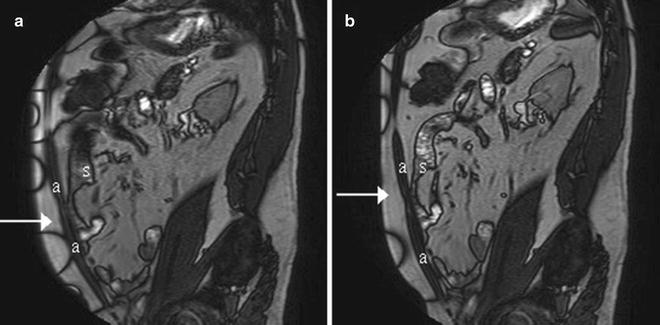
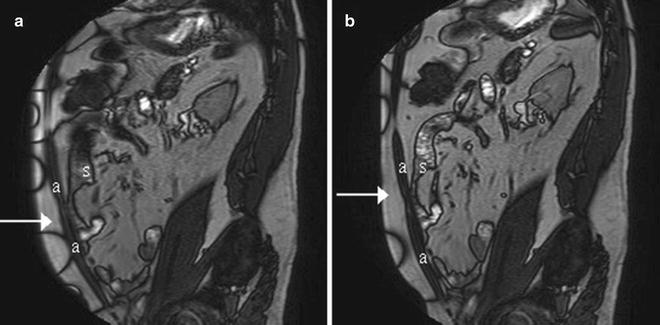
Fig. 20.4
Midsagittal MRI showing adhesion (arrow) between abdominal wall (a) and small bowel(s) during inspiration (a) and expiration (b). With permission from Zinther NB, Zeuten A, Marinovskij E, Haislund M, Friis-Andersen H. Detection of abdominal wall adhesions using visceral slide. Surg Endosc. 2010;24(12):3161-6 © Springer in 2010 [21]
Timing of Surgery
While the timing of certain operations is out of the surgeon’s control (i.e., perforation, complete obstruction, sepsis), most cases can be performed electively and provide an early opportunity to optimize the chances of success after previous operation. As with any surgery, patient nutrition and cardiopulmonary status should be optimized before undergoing a complex procedure. In the case of previous operation in the distant past, timing may make little difference to the surgery performed. However, in cases of a recent operation, the difficulty of adhesiolysis can be dramatically altered by the appropriate timing of surgery.
Adhesions form within 5–8 days of surgery [22, 23]. These initial adhesions are more vascular and diffuse, making adhesiolysis significantly more difficult and dangerous. The ability to delay surgery by 3 months beyond the previous operation (such as an ileostomy closure) will allow time for these adhesions to become better defined, with less density and vascularity [24, 25]. This delay may decrease complications, blood loss, and operative time.
For cases where delay is not possible, the surgery should be undertaken with extreme caution. In conjunction with anesthesia, a brief risk assessment can still be easily performed. In addition, consideration for the potential need for diversion is crucial, and patients should be appropriately marked in the preoperative holding area. Extended operative times and increased blood loss should be expected and planned for accordingly. Managing expectations for the patient, family, and surgical team is important, as these cases are often complicated. Blunt dissection may be less appropriate in this setting, as vascular adhesions will bleed more often, obscuring the operative field and causing increased blood loss. While laparoscopy still holds the potential for fewer postoperative complications, the risk-benefit ratio may be dramatically different in these patients and should be considered carefully.
Gaining Access
The first step in any minimally invasive abdominal procedure is entry into the abdominal cavity, and safe performance of this step is critical in reoperative colorectal surgery. In a review of the reasons for enterotomy during laparoscopic surgery, nearly 42 % of injuries were caused by Veress needle or trocar placement, making entry into the abdominal cavity the most treacherous period of laparoscopic surgery [13]. While the incidence of these injuries is low (0.18 %), more than half of these injuries occur in patients with a previous operation [26], demonstrating the importance of caution during abdominal entry and the need for careful choice of entry technique. Large meta-analyses of laparoscopic entry have shown no difference in major complication rates between open and closed techniques [27]. The Hasson technique, which allows direct visualization as the abdominal cavity is entered, has generally provided the safest results, particularly when used away from previous surgical sites [28, 29].
The Veress needle technique is often preferred by surgeons due to speed and prevention of gas leakage at the trocar site. For reoperations in patients without a previously violated left upper quadrant (LUQ), Veress needle entry into this area may be a reasonable alternative and has demonstrated comparable outcomes in reoperative surgery with an intestinal injury rate of 0.4 % [30]. Veress needle entry into the LUQ has become our preferred method of abdominal entry, as most prior surgeries are performed in the lower quadrants or right upper quadrant (Fig. 20.5) [11]; however, prior LUQ surgeries, such as splenectomy or gastric resection, must first be excluded. Optical trocars (Fig. 20.6; Video 20.1) have been suggested as another possible alternative, allowing visualization with rapid abdominal access even in reoperative cases [31]; however, reports have indicated that optical trocars cannot prevent injury during abdominal entry [15, 32].
Fig. 20.5
Rates of previous surgery type in reoperative laparoscopic colorectal surgery. Figure represents data from Franko et al. [11]; 347 patients undergoing laparoscopic colorectal surgery were identified with prior operations. With permission from Franko J, O’Connell BG, Mehall JR, Harper SG, Nejman JH, Zebley DM, et al. The influence of prior abdominal operations on conversion and complication rates in laparoscopic colorectal surgery. JSLS : Journal of the Society of Laparoendoscopic Surgeons 2006;10(2):169-75 © Society of Laparoendoscopic Surgeons 2006 [11]
Fig. 20.6
Abdominal entry techniques. (a) Trocar through upper midline abdominal entry point using Hasson technique. (b) Veress needle in left upper quadrant. (c) Optical trocar in left upper quadrant. Clear trocar tip allows light to pass from camera lens for visualization
The “peek-port” technique [33] has been promoted as a rapid and less costly method for evaluating the potential for laparoscopic completion of a reoperative case. In this method, a small midline incision is made and used to evaluate the intra-abdominal cavity for the appropriateness of laparoscopy. In patients with a previous midline incision, an off-midline incision should be used for entry to avoid adhesions. If the patient is considered an appropriate candidate, then a hand-assist port is placed and the laparoscopic equipment is opened for a hand-assisted, laparoscopic case. If the abdomen is considered unfavorable for laparoscopy, then the midline incision is lengthened to continue the case as a laparotomy. Results from a single-institution series using this technique demonstrated 32 % rate of immediate conversion to laparotomy and a 5 % rate of late conversion after attempted laparoscopy. In cases where the peek-port technique was not used, the conversion rate to laparotomy was 2 %, potentially due to patient selection [33].
Identifying Important Anatomy
Due to dense adhesions and distorted anatomy from previous resection, finding critical landmarks to guide surgery and avoid serious injury can be difficult in reoperative cases. Attempting to perform an extensive lysis of adhesions in an unfamiliar operative field can be a dangerous and unnerving experience; therefore, the use of aids or alternate techniques may provide assistance in orienting the surgeon and decreasing the risk of injury.
Ureters
Although identifying and preserving the ureters is always a concern during colorectal surgery, special consideration needs to be given to this topic for reoperative cases with a laparoscopic approach. Although studies have not demonstrated increased rates of ureteral injury during reoperative colorectal surgery [11], adhesive disease, distorted anatomy, and increased dissection make the safety of the ureters a special concern during these cases. In general, the ureters tend to be more medially located than normal, especially in the pelvis, following prior surgery. However, this may not always be the case, and it is important to have several options to find them if you cannot do it via standard medial and lateral approaches. One method is to start at the splenic flexure (assuming this is relatively undisturbed anatomy) and locate the ureter as it courses from the kidney along the retroperitoneum and track it caudally into the pelvis.
Another method for identification is ureteral stenting, which has a well-established history in colorectal surgery. Although studies have not demonstrated decreased rates of ureteral injuries during typical or complex surgery [34, 35], many surgeons advocate the utility of intraoperative injury recognition with stenting. With the advent of laparoscopic colorectal surgery, the tactile feedback provided by ureteral stents was replaced with lighted stents that could be visualized during surgery (Video 20.2). While no significant improvements in outcomes have been detected, rates of ureteral visualization greater than 80 % have demonstrated the potential utility of this technique [36]. Prophylactic bilateral stenting of the ureters before complex reoperative colorectal cases that involve pelvic dissection may improve ureter identification and recognition of intraoperative injuries. We strongly advocate the routine placement of lighted stents in purely laparoscopic cases due to the loss of tactile feedback.
Bladder
Bladder catheters should be placed in all complex colorectal cases involving the pelvis to decompress the bladder, improve exposure, and decrease the chance of a bladder injury. The catheter can also allow for monitoring of urine output and an assessment of intraoperative fluid status, an important consideration in reoperative cases that may be prolonged due to extensive adhesiolysis. Finally, the catheter balloon can provide a landmark in the lower pelvis for the location of the bladder to help orient the surgeon and safeguard against bladder injury.
Major Blood Vessels
Colorectal surgery is often performed in close proximity to several large vessels in the pelvis; however, the most commonly injured are the epigastric vessels during trocar placement in the anterior abdominal wall. Avoidance of these vessels can be managed in several ways. Initial entry in a midline position may allow for intra-abdominal examination for vessel identification. Transillumination of the anterior abdominal wall using the laparoscopic light source can help to identify the location of the epigastric vessels. In the case of dense adhesions or an obese patient, the surgeon can avoid the epigastric artery by remaining close to the midline or well lateral to the midclavicular line for port placement. Inserting the working trocars lateral to the rectus muscle will also minimize the risk of injuring these vessels. Finally, the visual inspection of the port sites both at the time of placement and removal will insure that any injury will be promptly recognized and treated.
Although damage to other major vessels such as the iliac arteries is rare, these injuries can be catastrophic. Extreme care must be exercised during a redo pelvic dissection, as normal anatomic landmarks may be missing or difficult to identify. The surgeon must be cognizant of energy sources used in dissection because the optics for these cases may be altered, leading to missed identification of normally seen pulsating structures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








