Fig. 9.1
Operative positioning for open total gastrectomy
Peritoneal Cavity Exploration
To evaluate peritoneal seeding or distant metastasis, careful exploration of the peritoneal cavity should be performed. If there is a suspicious lesion for peritoneal seeding or other distant metastasis, intraoperative frozen biopsy is required. For suspected malignant ascites, cytologic washings may be helpful. Evaluation for resectability is also essential during peritoneal cavity exploration. Invasion of the aorta, diaphragm, pancreas, or other adjacent organs should be checked. If there is no evidence of distant metastasis and primary gastric cancer is resectable, abdominal incision can be extended for the radical operation.
To obtain an optimal operative field and avoid unexpected injury to the spleen, it is helpful to place a surgical pad behind the spleen. Sometimes, dividing the triangular ligament and flipping over the left lateral section of the liver is necessary to widely expose the gastroesophageal junction and distal esophagus. Traction in four diagonal directions and pushing the diaphragm upward with a self-retraining retractor is useful to obtain an adequate operative field for total gastrectomy (Fig. 9.2).
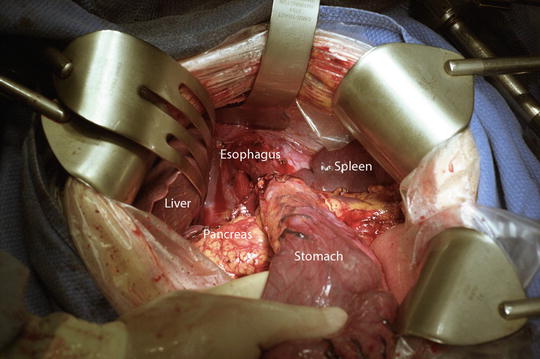
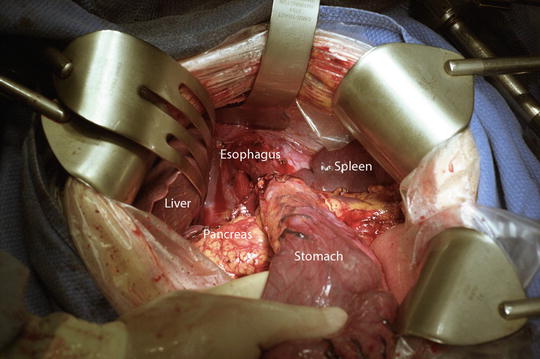
Fig. 9.2
A self-retaining retractor is used to provide optimal exposure of the operative field
Total Gastrectomy With D2 Lymph Node Dissection
Total Omentectomy
Omentectomy starts from the middle of the transverse colon and is usually performed to the left side first. To develop an adequate dissection plane for total omentectomy, it is necessary for the assistant to spread the transverse mesocolon downward with appropriate tension. During omentectomy, it is important not to injure the transverse colon or vasa recta around the colonic wall. The necessity of omental bursectomy is controversial. A randomized controlled trial to evaluate the clinical benefit of bursectomy for cT3-4a gastric cancer is ongoing in Japan.
Left Side Omentectomy With Dissection of Lymph Node Station 4sb
To complete dissection of lymph node (LN) station 4sb, it is mandatory to ligate the root of the left gastroepiploic artery (LGEA). Division of the splenocolic ligament is useful to expose the root of the LGEA and lower pole of the spleen. During dissection, it is easy to injure the inferior polar artery towards the lower pole of the spleen or pancreatic tail, which may cause partial infarction of the spleen or lead to pancreatic fistula.
Right Side Omentectomy With Dissection of Lymph Node Station 6
Right side omentectomy continues toward the hepatic flexure of the colon and the second portion of the duodenum. Wrapping and lifting up the stomach using surgical gauze by the assistant is useful to help develop the appropriate surgical field. Dissection along the middle colic vein as well as accessory right colic vein is helpful to find an avascular plane for safe approach to the area of lymph node station 6. Following the avascular plane, the dissection eventually leads to the gastrocolic trunk and superior mesenteric vein (SMV). Careful dissection is mandatory not to injure these named vessels. Using the avascular plane, omental bursectomy may be easier for right-sided omentectomy than for left-sided omentectomy. Meticulous dissection of the gastrocolic trunk and anterior surface of the pancreatic head can expose the root of the right gastroepiploic vein (RGEV). After identification of the anterior superior pancreaticoduodenal vein (ASPDV) and gastrocolic trunk, the RGEV can be ligated just distal to the ASPDV. According to the Japanese classification of gastric carcinoma guideline third edition [1], it is optional to dissect LNs around the SMV (i.e., LN number 14v) for D2 LN dissection.
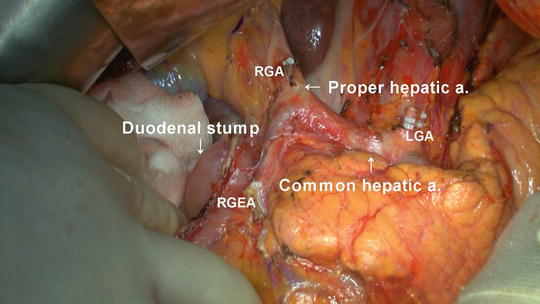
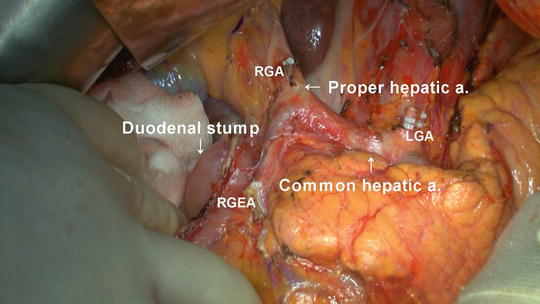
Complete dissection around the pancreatic head and gastroduodenal artery (GDA) can expose the root of the right gastroepiploic artery (RGEA). After ligation of the RGEA at its root, careful dissection and ligation of the infrapyloric artery is also required. Energy device (ultrasonic or bipolar) is helpful to dissect not only the infrapyloric artery but also the small branches to the posterior wall of the duodenum from the GDA.
Dissection of Lymph Node Stations 5 and 12
Division between LN stations 5 and 8 can effectively expose the medial side of the proper hepatic artery as well as the root of the right gastric artery (RGA). To develop a good surgical field, it is useful for the assistant to roll down the first portion of duodenum to the caudal side to make appropriate tension. During dissection of LN station 12 (i.e., hepatoduodenal ligament LNs along the proper hepatic artery in the caudal half between the confluence of the right and left hepatic ducts and the upper border of the pancreas), it is important not to injure the hepatic artery, bile duct, and portal vein.
After careful dissection of the hepatoduodenal ligament, the root of the RGA can be identified and ligated. For sufficient mobilization of the duodenum, one or two supraduodenal vessels can also be ligated.
Duodenal Transection
A linear stapler can be used for duodenal transection (Fig. 9.3). After transection, the operator should be careful to obtain hemostasis of the staple line. Attempts to obtain hemostasis with electrocautery may cause postoperative duodenal stump leakage. Reinforcement of the staple line with Lambert sutures, even though it may not always be necessary, can be useful to prevent duodenal stump leakage.
 < div class='tao-gold-member'>
< div class='tao-gold-member'>




Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








