Fig. 14.1
Dissection of the avascular plane between the greater omentum and the transverse mesocolon during gastrectomy. (Image courtesy of Paul F. Mansfield, MD)
Mobilize the greater curve by dividing the gastrocolic omental tissue outside of the gastroepiploic vessels to the planned point of transection of the proximal stomach. Extending the area of dissection to the left will help facilitate the exposure and dissection of the gastroepiploic vessels.
Trace the middle colic vessels down to the gastrocolic trunk to identify the right gastroepiploic vessels. Lymphatic tissue and identifiable lymph nodes often must be removed to identify the gastroepiploic vessels and can be swept toward the pylorus with the specimen or can be removed and labeled separately.
Ligate the gastroepiploic vein and artery with 2–0 or 3–0 silk, and place an additional 4–0 polyprolene suture on the proximal aspect of the artery to provide hemostatic security. Divide the right gastroepiploic vessels.
Isolate, ligate, and divide the right gastric vessels close to the proper hepatic artery.
Isolate the duodenum. Often a few additional small feeding vessels must be ligated and divided. Ligate the duodenum with a 3.5-mm thoracoabdominal (TA) stapler, and transect the duodenum with a knife. Alternatively, use a gastrointestinal anastomosis (GIA) stapler or sharp transection with handsewn closure to transect the duodenum (Fig. 14.2).
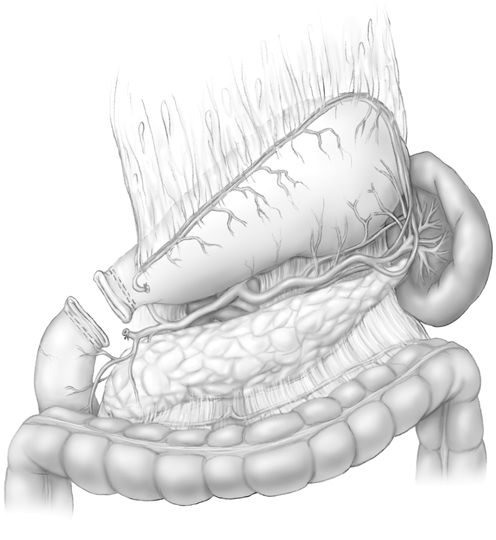
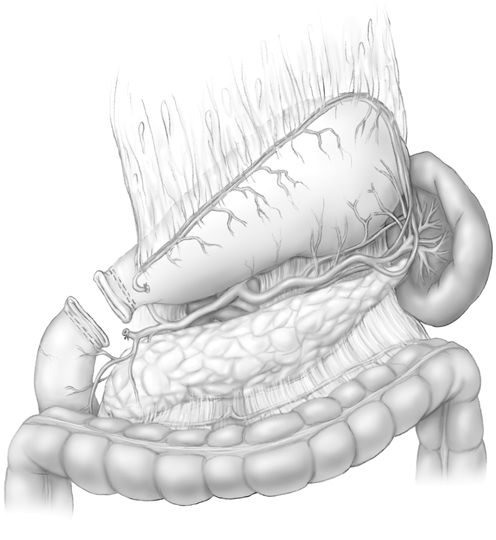
Fig. 14.2
Isolation, ligation, and transection of the duodenum during a subtotal gastrectomy. (Image courtesy of Paul F. Mansfield, MD)
Obtain a specimen from the duodenal margin, and send for immediate frozen-section analysis to document a negative surgical margin.
Transect the thin avascular portion of the lesser omentum (Fig. 14.3). Guided by preoperative imaging, take care to identify a potential accessory or replaced left hepatic artery.
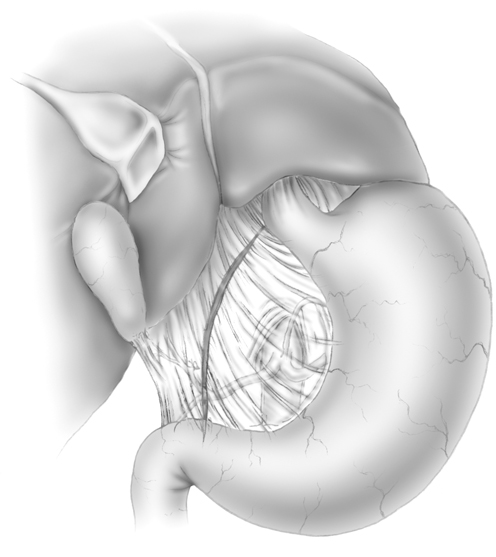
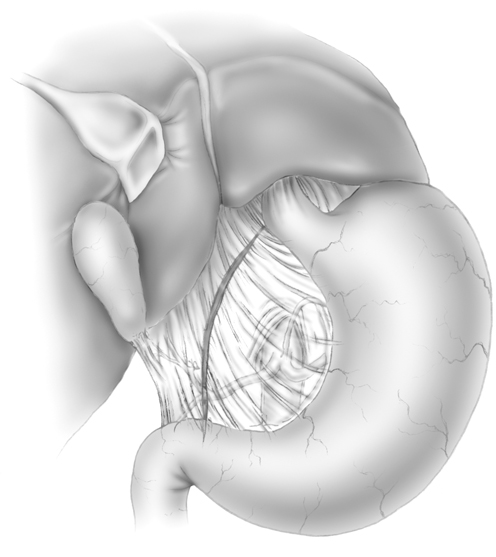
Fig. 14.3
Transection of the avascular portion of the lesser omentum during a subtotal gastrectomy . (Image courtesy of Paul F. Mansfield, MD)
Isolate, ligate, and transect the left gastric vessels. The left gastric vessel dissection can be initiated with anterior and cephalad retraction of the stomach. The left gastric vein (the coronary vein of the stomach) often is encountered surgically after the point at which it receives branches from the anterior and posterior lesser curvature but before the vein terminates in the portal vein. Ligate the left gastric vein with 3–0 silk. Variable amounts of celiac nodal tissue will be encountered prior to identification of the left gastric artery. The left gastric artery is identified most often in the middle of the celiac trunk. Ligate the left gastric artery with 2–0 or 3–0 silk, and place an additional 4–0 polypropylene suture on the proximal aspect of the left gastric artery to provide hemostatic security.
Identify a suitable area for transection of the proximal stomach. To help obtain a negative surgical margin, thoroughly review preoperative and pretreatment imaging and endoscopy results, use intraoperative palpation, and perform intraoperative endoscopy.
Transect the proximal stomach with a 4.8-mm GIA stapler. Alternatively, divide the stomach between bowel clamps, or ligate the stomach with a TA stapler and transect the specimen with a knife (Fig. 14.4).
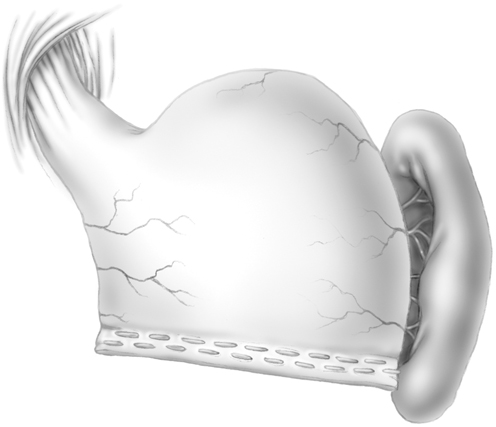
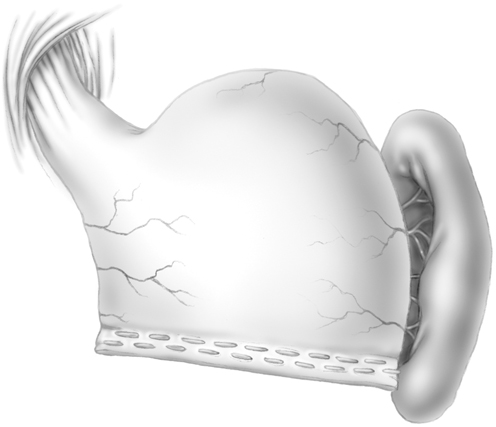
Fig. 14.4
Transection of the proximal stomach during a subtotal gastrectomy. (Image courtesy of Paul F. Mansfield, MD)
Remove the specimen staple line, deliver to pathology, and orient the specimen for the pathologist. Consider the gastric cancer histologic type (intestinal versus diffuse) when deciding whether to obtain circumferential or focused gastric margin specimens for intraoperative analysis.
While waiting for histologic confirmation of negative surgical margins along the proximal gastric staple line, which can be time-consuming if the entire gastric margin is examined, dissect the D2 lymph nodes (Fig. 14.5).
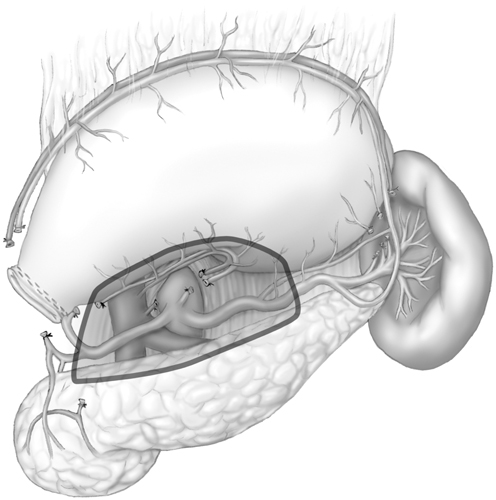
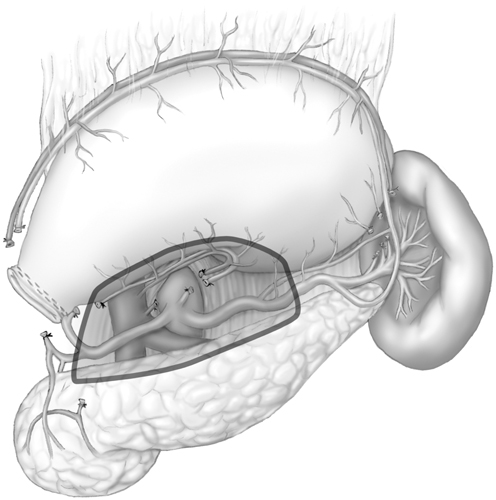
Fig. 14.5
D2 lymph node dissection during a subtotal gastrectomy. (Image courtesy of Paul F. Mansfield, MD)
Irrigate the abdomen, and confirm hemostasis.
Perform reconstruction with a Billroth II loop gastrojejunostomy or a Roux-en-Y gastrojejunostomy (both described below).
Billroth II Loop Gastrojejunostomy
In general, oversew a portion of the lesser curvature staple line with 3–0 silk Lembert sutures not only to reinforce an area that could be at high risk for leakage but also to limit the size of the upcoming anastomosis, as a full-length gastrojejunostomy is unnecessary.
Create a defect in the transverse mesocolon, and perform the anastomosis in a retrocolic fashion.
For a handsewn anastomosis, approximate the afferent limb of the small bowel to the greater curvature of the stomach and the efferent limb to the lesser curvature.
Alternatively, create a stapled anastomosis to the posterior stomach. Approximate the small bowel to the posterior stomach with 3–0 silk sutures at the corners of the anastomosis. Create a defect in the stomach and small bowel, perform a stapled side-to-side anastomosis with a GIA blue or green stapler, and close the gastroenterotomy defect.
Roux-en-Y Gastrojejunostomy
Use a blue GIA stapler to transect the first redundant limb that is suitable for limb creation distal (often approximately 20 cm) to the ligament of Treitz .
Using transillumination, take down the mesentery to identify feeding vessels and to determine the length necessary to prevent anastomotic tension.
Create a defect in the transverse mesocolon to the left of the middle colic vessels, and place the roux limb into position. Confirm that the roux limb is tension-free.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







