Office Hysteroscopy
Rafael F. Valle
Although modern hysteroscopy has evolved over the last 35 years, its use in the office setting was not made practical until an innovation in the early 1980s. The introduction of small-caliber hysteroscopes, <5-mm outer diameter, simplified ambulatory uterine exploration and, jointly with the already well-established methods of office sampling of the endometrium, significantly improved the office evaluation of patients complaining of abnormal uterine bleeding.
Other methods of uterine evaluation have been introduced such as vaginal sonography, fluid-enhanced sonography, and magnetic resonance imaging (MRI), all of them offering specific features that complement each other and are valuable in the appropriate evaluation of selected patients.
It is important, nonetheless, to understand the reasons for looking into the uterine cavity, the principles of panoramic hysteroscopy, and the appropriate technique in its performance. Furthermore, it is important to clearly define the selection of patients and exclusion criteria needed to perform hysteroscopy in a safe, simple, and efficient manner that will pave the way to a procedure performed free of complications and that will help derive specific standards of an appropriate patient evaluation.
Principles of Panoramic Hysteroscopy
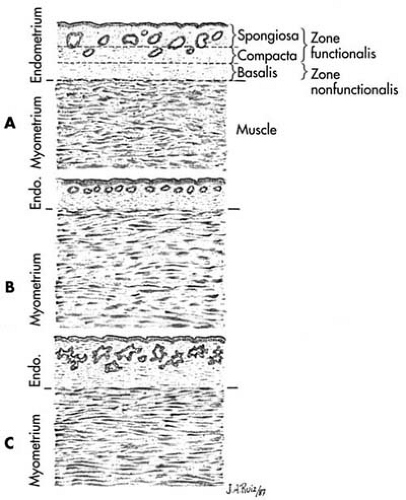
The uterus is an organ with thick muscular walls in apposition, with a central virtual cavity lined with an epithelium that bleeds cyclically. Its surface changes constantly in thickness and structure during the menstrual cycle. To convert this virtual cavity to an actual volumetric space for panoramic visualization, positive pressures of the distending medium inside the uterine cavity are required. Because the endometrial lining varies in thickness and friability, distention of the uterine cavity is easier at some periods than at others during these cyclic changes (Fig. 17.1).
These anatomic and physiologic features help explain why the use of hysteroscopy did not keep pace with cystoscopy, despite their common origin. The urinary bladder requires gravity pressure only for its distention rather than positive pressure, since a thin muscle of the bladder wall can achieve distention easily. Furthermore, its transitional epithelium neither bleeds cyclically nor changes periodically in thickness and structure and seldom bleeds on contact. These features explain why cystoscopy was a practical technique on introduction of the original cystoscope by Desormeaux in 1865 (Table 17.1). Rubin noted these differences in the 1920s
when he began distending the uterine cavity with CO2 gas to perform hysteroscopy and therefore adapted the positive pressures to the uterus to maintain uterine wall separation while visualization was taking place.
when he began distending the uterine cavity with CO2 gas to perform hysteroscopy and therefore adapted the positive pressures to the uterus to maintain uterine wall separation while visualization was taking place.
Methods of Uterine Distention for Hysteroscopy
Since the early 1970s when hysteroscopy became a practical method for intrauterine visualization, the media most commonly used for uterine distention to perform panoramic hysteroscopy have been dextran 70, 32% weight/volume (w/v) in dextrose 10% (w/v) or Hyskon; carbon dioxide (CO2) gas insufflation; and low-viscosity fluids
with or without electrolytes.
with or without electrolytes.
Dextran in Dextrose (Hyskon)
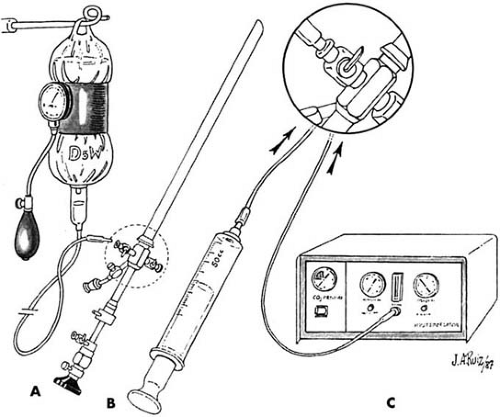
Dextran 70, 32% w/v (Hyskon), is an optically clear, viscous solution with a high refractory index and high viscosity of 25 centipoise (cp) at 37°C. It has a molecular weight of 70,000 and does not mix easily with blood. It offers excellent clear vision in panoramic hysteroscopy, requiring only about 50 mL of solution for each examination. Spillage during the examination is minimal. Previously, during the hysteroscopic examination, an assistant delivered the Hyskon by means of a syringe through a connective tubing attached to the inflow channel of the hysteroscope (Fig. 17.2). This method, however, seldom is used at present.
Carbon Dioxide Gas Insufflation
CO2 gas insufflation permits excellent visualization of the uterine cavity; it provides good uterine distention and keeps the instruments and the operative field relatively clean. Delivery of the gas to the uterine cavity requires a special hysteroscopy insufflator that monitors electronically the intrauterine pressure and flow rate to the uterine cavity (Table 17.2). The use of CO2 gas has been confined to the office and at present, owing to advances in continuous-flow systems for hysteroscopy that permit the easy use of low-viscosity fluids, is not frequently used.
TABLE 17.1 Factors Related to Panoramic Endoscopy of Uterus and Urinary Bladder | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Low-Viscosity Fluids
Low-viscosity fluids can be devoid of electrolytes when electrosurgery is to be used; those with electrolytes can be used when no conduction of electrosurgery is expected. The most commonly used low-viscosity fluids containing electrolytes are normal saline, dextrose 5% in ½ normal saline, and Ringer lactate. When electrosurgery is necessary, the commonly used fluids are glycine 1.5%, sorbitol 3%, mannitol 5%, and 5% dextrose in water (D5W). Low-viscosity fluids offer an advantage of washing the uterine cavity prior to uterine distention or when debris, mucus, or blood clots are encountered with manipulation, particularly after cervical dilatation and operative procedures. When the hysteroscope lacks continuous flow, this washing effect is obtained through a polyethylene catheter introduced through the operating channel of the hysteroscope to obtain a practical inflow and targeted outflow system under a low gravity pressure. When the returning fluid becomes clear, the polyethylene catheter is occluded and adequate distention begins. These media clear the endometrial cavity of debris, mucus, or blood clots and aid in the assessment of tubal patency by hysteroscopy with concomitant laparoscopy.
In general, no one of these three methods is better than the others for diagnostic hysteroscopy; with each, examination and hysteroscopic interventions can be performed adequately when the specific technique is well known and the operator is familiar with the properties, peculiarities, and possible side effects of each specific method. When the operator has experience with all of them, they can be interchanged and combined during an examination. Nonetheless, CO2 gas insufflation remains the method of choice for therapeutic office hysteroscopy, along with low-viscosity fluids.
TABLE 17.2 Flow Rates and Intrauterine Pressure for CO2 Hysteroscopy | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Diagnostic Hysteroscopes
Diagnostic hysteroscopes of small caliber (<5-mm outer diameter) can be of two types: rigid and flexible. The rigid endoscopes have wide-angle optics and excellent resolution. The telescope has a 3- to 4-mm outer diameter, and the encasing sheaths a 4- to 6-mm outer diameter. Although all endoscopes of <3-mm outer diameter encased in a 4-mm outer diameter sheath seldom require cervical dilatation, when this diameter increases, some type of dilatation may be required. Because of their size, hysteroscopes with a 4-mm or less outer diameter are better used with CO2 gas distention to avoid the following: clouding of the field when liquids are used, difficulty in washing the uterine cavity, and
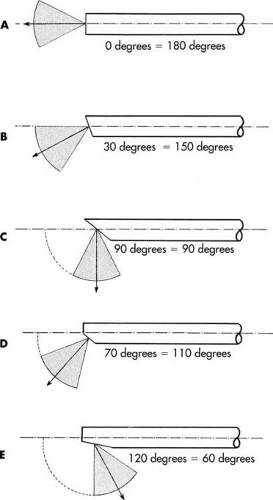
retrieving the fluid through an outer port. For these reasons, most of these hysteroscopes have only one port, the inflow. New diagnostic/operative hysteroscopes, 4- to 6-mm outer diameter, with continuous-flow system capabilities have been introduced, permitting continuous washings of the uterine cavity. However, because of their size, they may occasionally require cervical dilatation before introduction. These hysteroscopes are fitted with a 5-F operative channel for minor surgical procedures. Most of these endoscopes are manufactured to accommodate different adapters for various light cables, and additionally they should have a good locking mechanism that avoids dislodging the telescope by tripping. The distal end of the hysteroscope can be beveled to accommodate the fore-oblique (30-degree angle) view telescope. Some physicians prefer a direct 180-degree view, but the visualization of the uterotubal cones may be somewhat more difficult (Fig. 17.3). However, because of their size, they may occasionally require cervical dilatation before introduction. A 5-F operative channel is useful for minor surgical procedures.
retrieving the fluid through an outer port. For these reasons, most of these hysteroscopes have only one port, the inflow. New diagnostic/operative hysteroscopes, 4- to 6-mm outer diameter, with continuous-flow system capabilities have been introduced, permitting continuous washings of the uterine cavity. However, because of their size, they may occasionally require cervical dilatation before introduction. These hysteroscopes are fitted with a 5-F operative channel for minor surgical procedures. Most of these endoscopes are manufactured to accommodate different adapters for various light cables, and additionally they should have a good locking mechanism that avoids dislodging the telescope by tripping. The distal end of the hysteroscope can be beveled to accommodate the fore-oblique (30-degree angle) view telescope. Some physicians prefer a direct 180-degree view, but the visualization of the uterotubal cones may be somewhat more difficult (Fig. 17.3). However, because of their size, they may occasionally require cervical dilatation before introduction. A 5-F operative channel is useful for minor surgical procedures.
Flexible Hysteroscopes
Flexible hysteroscopes are also adapted to permit distal steerability with some rigidity in the main shaft, so they can be introduced as if they were rigid at initial insertion. The proximal steering knob is fixed to make the distal tip somewhat rigid while beginning the insertion; the 3.3-mm outer diameter flexible hysteroscope permits cervical introduction without previous cervical dilatation. The granular aspect of the image has been refined lately and approaches the image obtained by rigid endoscopes. These flexible hysteroscopes are totally assembled and come in a single unit.
Microhysteroscopes
Small-caliber hysteroscopes, <3 mm in outer diameter, may further simplify the use of hysteroscopy in the office setting. This is particularly true for those designed to permit either CO2 gas for uterine distention or low-viscosity fluids under a continuous-flow system, as well as instrumentation throughout an expandable outer sheath, not requiring cervical dilatation before insertion. Most small-diameter hysteroscopes are now adapted with a 5-F operative channel so flexible or semirigid instruments can be used.
Panoramic Hysteroscopy in the Office
Selection of patients is based on appropriate indications, complete medical history, and physical examination—including a pelvic examination, recent Papanicolaou smear, cervical and vaginal smears and cultures, and a pregnancy test when appropriate. Although specific indications for performing panoramic hysteroscopy may vary according to the patient’s needs and the skill of the endoscopist, contraindications to this technique should be ruled out.
Contraindications of Hysteroscopy
There are a few absolute contraindications to hysteroscopy. They are the following: desired pregnancy, cervical infection, profuse uterine bleeding, and known cervical malignancy.
Pregnancy
Because hysteroscopy invades the uterine cavity, pregnancy is a contraindication owing to the dangers of introducing infection to the early conceptus or interrupting a desired pregnancy. Hysteroscopy may be modified as an amnioscopic examination in selected patients but under strict criteria and a specific technique.
Recent or Existing Uterine or Cervical Infection
The danger of spreading infections from the lower genital tract into the peritoneal cavity by way of the fallopian tubes or the systemic circulation dictates avoidance of hysteroscopy when infection is suspected.
Profuse Uterine Bleeding
In the presence of excessive uterine bleeding or menstruation, hysteroscopy cannot be performed satisfactorily, regardless of the distending medium, and should therefore be avoided.
Known Cervical Malignancy
The presence of invasive cervical malignancy is another absolute contraindication, not only because hysteroscopy is of doubtful value in these situations, but also because cervical manipulation may spread malignant cells.
Relative Contraindications
Relative contraindications to hysteroscopy are the following: known adenocarcinoma of the endometrium when the clinician is not familiar with this disease, marked cervical stenosis not resolved by usual dilation, and the operator’s unfamiliarity with the instrumentation and technique used, particularly unfamiliarity with the distending medium used and its delivery.
Clinical Indications for Hysteroscopy
Clinical studies have demonstrated the value of hysteroscopy in the diagnosis and treatment of patients afflicted with various gynecologic problems. The present indications for hysteroscopy are the following:
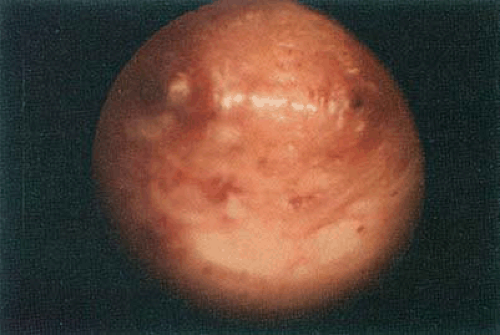
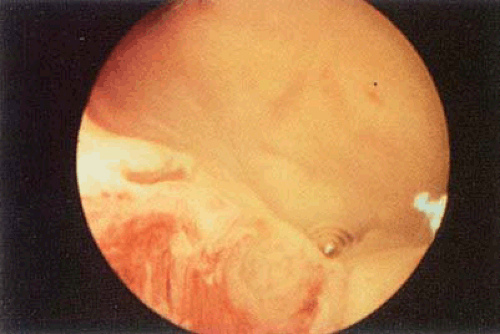
Abnormal premenopausal and postmenopausal uterine bleeding (Figs. 17.4 and 17.5).
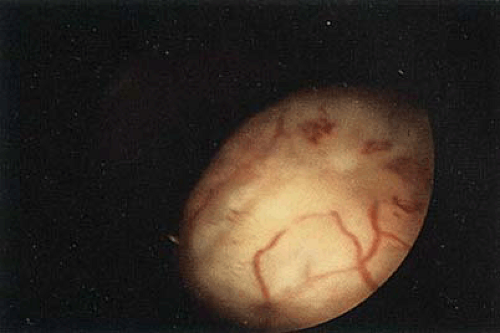
Diagnosis and possible transcervical removal of submucous leiomyomas or endometrial polyps (Figs. 17.6, 17.7, 17.8).
Location and retrieval of “lost” intrauterine devices or other foreign bodies.
Evaluation of infertile patients with abnormal hysterograms (Fig. 17.9).
Diagnosis and surgical treatment of intrauterine adhesions.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree