Hysteroscopy for Abnormal Bleeding
Hubert Guedj
Jacques Barbot
Michael S. Baggish
Abnormal uterine bleeding is the oldest and the most frequent indication for the performance of hysteroscopy. Let us recall that the first successful hysteroscopy was performed by Pantaleoni in 1869 on a postmenopausal woman suffering from uterine bleeding. He discovered an endometrial polyp and cured his patient. Let us also keep in mind that for more than a century, blood has been the main hindrance to clear viewing of the uterine cavity, and this has delayed the development of hysteroscopy. Consequently, curettage and, later, hysterography have remained until recently the two main procedures for the investigation of metrorrhagia. Nowadays blood is no longer a visual problem, and hysteroscopy has become the most accurate method available to evaluate the endometrial cavity.
Not only has hysteroscopy greatly improved our understanding of abnormal bleeding by providing direct viewing of the bleeding disorders, but the most recent advances in operative hysteroscopy have allowed specific treatment of each disorder, completely changing our therapeutic approach. The old dilemma of choosing between repeated blind curettage or hysterectomy no longer exists. The introduction of electrosurgery or laser surgery within the uterine cavity now allows conservative treatment with long-lasting results in most cases.
In a recent study, de Wit et al. (2003) reviewed 1,045 diagnostic hysteroscopy procedures performed over 6 years. Most of these procedures were done because of abnormal bleeding. A normal cavity was seen in 54.2%, submucous myoma in 21%, and endometrial polyps in 14.4%. Endometrial hyperplasia and carcinoma (seven cases) made up the remainder of cases. The authors concluded that diagnostic hysteroscopy was a valuable tool. Ben-Yehuda et al. (1998) tried to determine whether hysteroscopy improved the accuracy of blind dilatation and curettage. The major deficiency of this report, however, was the obvious lack of expertise among the participating hysteroscopists who could barely differentiate hyperplasia in 50% of cases together with <20% pick-up rate for endometrial carcinoma. By way of contrast, Clark et al. in the United Kingdom (2002) performed a macroanalysis using 208 articles and 26,346 cases. Based on pooled ratios, the pretest probability of endometrial cancer was 3.9%. A positive hysteroscopic diagnosis increased the probability of cancer to 71.8%, and a negative hysteroscopy result reduced the probability of cancer to 0.6%.
Place of Abnormal Uterine Bleeding among the Indications for Hysteroscopy
Abnormal bleeding is one of the most common gynecologic disorders that prompt a patient to consult a physician. This should not be a surprise, since most intrauterine abnormalities sooner or later generate this alarming symptom. The emergence of new indications and the resulting diversification in the use of hysteroscopy have tended to reduce the indications related to metrorrhagia in young women. In postmenopausal women in whom disease related to reproduction is minimal, abnormal bleeding constitutes the major indication for intervention. Of course, the number of hysteroscopies performed for abnormal bleeding will vary, depending on each physician’s particular orientation in the field of gynecology.
Metrorrhagia was the primary indication for hysteroscopy in 48% of the 500 cases published by Porto in 1974. It accounted for 49.6% of 320 patients reported by Sciarra and Valle in 1977. This symptom was the indication for hysteroscopy in 37.5% of 680 examinations performed by Hamou et al. In a series of 810 contact hysteroscopies we performed in patients with problems not related to pregnancy, abnormal bleeding was the main complaint in 64.8% of the cases. In a recent series of 1,500 hysteroscopies, it accounted for 52.1% of the patients. Essentially one hysteroscopy out of two is performed because of abnormal bleeding.
Bain et al. (2002) randomized women to either outpatient hysteroscopy and endometrial biopsy or endometrial biopsy alone. The addition of hysteroscopy in this series did not increase the accuracy of the biopsy although zero endometrial cancers were diagnosed in the 370 women participating in the study. Gebauer et al (2001) studied whether hysteroscopy improved the detection and extraction of
endometrial polyps in women with postmenopausal bleeding. The authors concluded that curettage was not sufficient for either detection or extraction of polyps. Hysteroscopy picked up 51 polyps among 83 women with postmenopausal bleeding or ultrasonographically thickened endometrium whereas curettage diagnosed 22.
endometrial polyps in women with postmenopausal bleeding. The authors concluded that curettage was not sufficient for either detection or extraction of polyps. Hysteroscopy picked up 51 polyps among 83 women with postmenopausal bleeding or ultrasonographically thickened endometrium whereas curettage diagnosed 22.
Technique of Hysteroscopy: Particular Points Related to Uterine Bleeding
Is the technique of hysteroscopy different when the investigation is performed because of abnormal bleeding? When the endoscopic examination is performed in the absence of blood, the technique is, of course, very straightforward and quite routine. To perform the examination during an episode of bleeding—either because of an emergency or because medical treatment cannot stop the bleeding—requires greater skill. The difficulties will be variable, depending on (a) the magnitude of the bleeding, (b) the available instrumentation, (c) the technique used, and (d) the experience of the hysteroscopist.
The case for emergency hysteroscopy is controversial. In the face of heavy uterine bleeding, the ability to see the entire cavity and to see accurately is questionable. The only medium that does not mix with blood and that permits a reasonably accurate hysteroscopic examination is Hyskon (dextran 32). Hysteroscopy does not in itself provide treatment for menorrhagia but may provide the vehicle through which treatment may be performed, e.g., endometrial ablation. Shalev et al. (2004) reported 41 cases in which emergency hysteroscopy was performed. In 40 cases, a benign, organic lesion was identified, and 1 case of endometrial cancer was diagnosed in the resection material. Quan et al. in China reported transcervical resection via hysteroscopy of placenta increta. This procedure is clearly dangerous and is not a recommended therapy for placenta accreta.
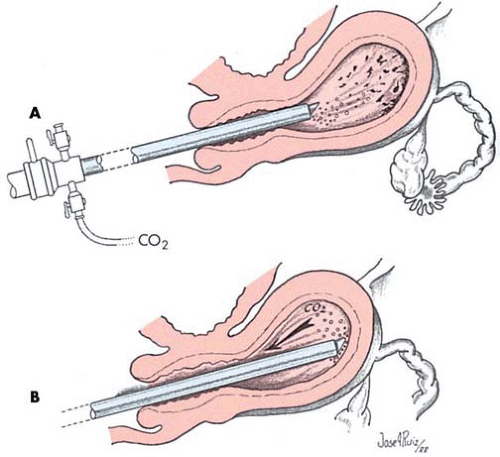
With CO2 as the distending medium, the presence of blood can cause the formation of gas bubbles, which make vision hazy or may even obtund the whole field of view. Some artifices are useful to know to cope with this particular situation. It is advisable to use a hysteroscope sheath provided with a gas channel opening at the tip of the telescope. The gas flow will clear the optic surface, blowing away bubbles and blood. This device was described by Semm as having a windshield wiper effect (Fig. 22.1A). When this action is incapable of providing clear viewing, one should touch the end of the telescope to the mucosa of the uterine fundus. This simple maneuver often restores satisfactory vision (Fig. 22.1B). In cases of failure, it will be necessary to remove the instrument and clean the tip of the telescope with gauze soaked in sterile saline or water.
Another problem associated with profuse bleeding that causes poor vision is obstruction of the gas channel by blood clots. This causes the uterine cavity to collapse, and a red curtain appears to cover the front of the telescope. The obstruction may be confirmed by removing the endoscope and submerging it in liquid: No bubbles are produced. The gas channel is unclogged by connecting a syringe to the inflow stopcock and injecting liquid under pressure through it. In other circumstances, the field will remain clear but the gas pressure will force a pool of blood to spread out over the posterior wall of the uterine cavity and submerge the cornua. Abnormalities located in those areas will remain undetected until the blood is removed. The easiest remedy is to introduce a catheter connected to a syringe through the operating channel and aspirate the blood under visual control. In case of bubble formation, the hysteroscopist must remain patient. Sometimes, after a short wait, the field will suddenly clear up and the bubbles will disappear. This event can be hastened by varying the gas pressure (either increasing or decreasing it). Since the clear view of the uterine cavity may last only a short time, the endoscopist must be ready to make a rapid diagnosis. When vision is severely restricted to the point of precluding a complete and reliable investigation, another distention technique should be used.
Another problem associated with profuse bleeding that causes poor vision is obstruction of the gas channel by blood clots. This causes the uterine cavity to collapse, and a red curtain appears to cover the front of the telescope. The obstruction may be confirmed by removing the endoscope and submerging it in liquid: No bubbles are produced. The gas channel is unclogged by connecting a syringe to the inflow stopcock and injecting liquid under pressure through it. In other circumstances, the field will remain clear but the gas pressure will force a pool of blood to spread out over the posterior wall of the uterine cavity and submerge the cornua. Abnormalities located in those areas will remain undetected until the blood is removed. The easiest remedy is to introduce a catheter connected to a syringe through the operating channel and aspirate the blood under visual control. In case of bubble formation, the hysteroscopist must remain patient. Sometimes, after a short wait, the field will suddenly clear up and the bubbles will disappear. This event can be hastened by varying the gas pressure (either increasing or decreasing it). Since the clear view of the uterine cavity may last only a short time, the endoscopist must be ready to make a rapid diagnosis. When vision is severely restricted to the point of precluding a complete and reliable investigation, another distention technique should be used.
The use of dextran as the distending medium is not common in Europe. Hyskon is worth trying in cases of severe bleeding either as the first technique or following the failure of CO2. Hyskon flow is used first to clear the uterine cavity of blood; then, vision is maintained because of lack of miscibility of this solution with blood.
Another alternative is to use a contact hysteroscope. When the instrument maintains mucosal contact, bleeding is no longer a problem regardless of the quantity of blood within the uterine cavity. The only limitation to this instrument is the proficiency of the operator to interpret contact vision correctly. However, the increasing tendency when facing profuse uterine bleeding is to turn immediately to a technique of hysteroscopy using a low-viscosity liquid for continuous flushing of the uterus. This has been made possible by the development of multichannel sheaths with separate inflow and outflow channels that allow the liquid medium to cleanse blood and debris from the uterine cavity and, at the same time, to distend the uterus to obtain clear panoramic vision. These sheaths have been designed for operative hysteroscopy but can also be useful for diagnostic hysteroscopy. The only drawback is the large caliber of the sheath, which makes cervical dilatation necessary. A small-caliber dual-channel sheath designed only for diagnosis would be helpful in such cases. The type of low-viscosity liquid that is used for this procedure is not important, and many solutions are safe, among which saline, sorbitol, mannitol, glycine, and lactated Ringer solution are easily available. The short duration of a diagnostic examination rules out any risk of fluid overload.
Hysteroscopic Findings in Patients with Abnormal Bleeding
The findings in a series of 768 hysteroscopies performed for abnormal bleeding appear in Table 22.1. During the women’s reproductive years, submucous myomas, endometrial hyperplasia, and endometrial polyps were the most common lesions detected (Figs. 22.2, 22.3, 22.4, 22.5). These accounted for more than half of all the findings (54% in this series). Pregnancy-related bleeding was the next most common diagnosis. In postmenopausal women, hyperplasia, polyps, and myomas were frequently found, as were endometrial atrophy and carcinoma (Figs. 22.6 and 22.7). Abnormalities that produce uterine bleeding are numerous and provide a microcosm of the whole catalog of intrauterine disease conditions. All cases of abnormal bleeding should be evaluated for pharmacologic and hemostatic factor deficiencies regardless of other suspected diagnostic possibilities.
Philipp et al. evaluated 115 women with an objective diagnosis of menorrhagia. Sixty-five women were between the ages of 20 and 44 years, 25 were adolescent, and 25 perimenopausal. Forty-seven of 115 women were anemic at the time of testing. Fifty-four of 115 women (47%) were found to have one or more hemostatic abnormalities, which included platelet aggregation, von Willebrand factor, and single-factor deficiencies.
TABLE 22.1 Findings in a Series of 768 Hysteroscopies Performed for Abnormal Bleeding | |||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||
Serebruany et al. (2005) analyzed the risk of bleeding complications after different doses of aspirin in 192,036
patients enrolled in 31 randomized, controlled trials. Low daily doses of aspirin (<100 mg) were associated with the lowest risk. Doses of aspirin of 325 mg or more per day were associated with significantly higher risks of major bleeding events.
patients enrolled in 31 randomized, controlled trials. Low daily doses of aspirin (<100 mg) were associated with the lowest risk. Doses of aspirin of 325 mg or more per day were associated with significantly higher risks of major bleeding events.
Contribution of Hysteroscopy according to Disorders Involved in Abnormal Uterine Bleeding (Excluding Pregnancy-Related Bleeding)
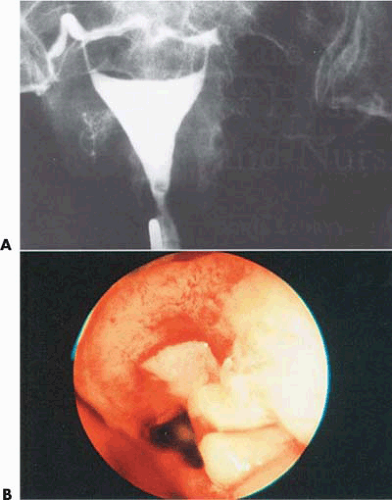
Endometrial polyps, submucous myomas, and endometrial hyperplasia account for most benign intrauterine disease conditions. They have several features in common. The primary presenting symptom is usually abnormal bleeding. The
gynecologic examination, including speculum examination and bimanual palpation of the uterus, does not usually lead to their diagnosis. It is now well documented that the standard diagnostic procedures designed to detect and differentiate these lesions are unreliable. The interpretation of abnormal shadows appearing on the hysterogram is uncertain or wrong in 30% to 50% of cases. Dilatation and curettage cannot remove the fibroids and often misses the polyps. An accurate diagnosis is absolutely necessary to direct the correct treatment, which is in fact different for the three lesions.
gynecologic examination, including speculum examination and bimanual palpation of the uterus, does not usually lead to their diagnosis. It is now well documented that the standard diagnostic procedures designed to detect and differentiate these lesions are unreliable. The interpretation of abnormal shadows appearing on the hysterogram is uncertain or wrong in 30% to 50% of cases. Dilatation and curettage cannot remove the fibroids and often misses the polyps. An accurate diagnosis is absolutely necessary to direct the correct treatment, which is in fact different for the three lesions.
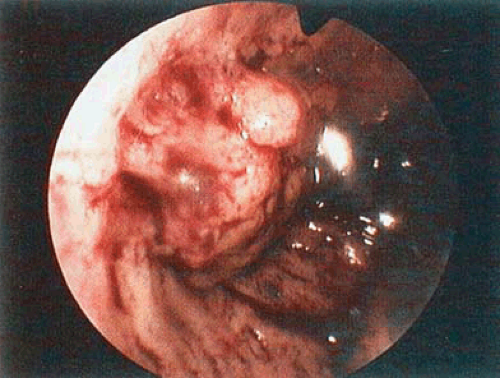 FIGURE 22.5 An endometrial polyp in a woman who had received tamoxifen treatment for breast cancer. The endometrium has been modified by the tamoxifen treatment. (Courtesy of H. Guedj, MD.) |
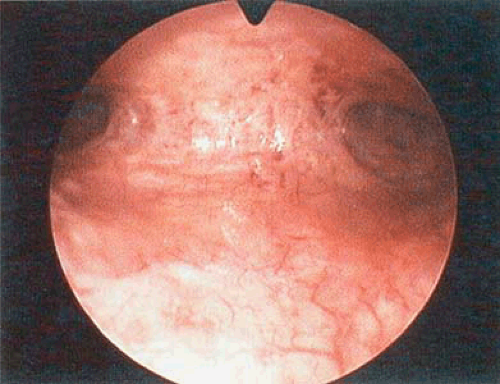 FIGURE 22.6 The endometrium shows extensive atrophy, which accounts for abnormal bleeding. (Courtesy of H. Guedj, MD.) |
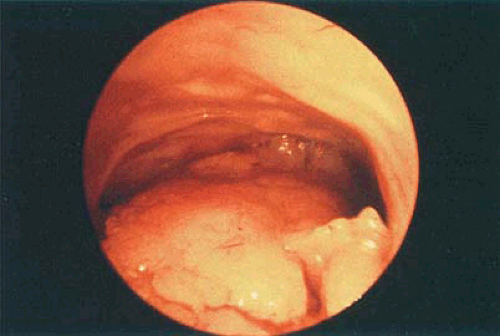 FIGURE 22.7 Abnormal vascular pattern and vegetations associated with adenocarcinoma endometrium arising from the posterior wall of the uterus. |
Endometrial hyperplasia requires curettage followed by hormonal therapy to prevent recurrence. A more recent management of this disorder is to substitute the resectoscope for the curette and use the electrical loop to resect the extra mucosa. A polyp requires precise division of its
pedicle at the base either with endoscopic scissors, an electric loop, or a laser fiber (Fig. 22.8). However, when the size of the polyp is important, its resection in fragments is advisable to facilitate its extraction through the cervix. A pedunculated myoma can be managed as a polyp, but the sessile variety requires either hysteroscopic resection when the submucous component is present or laparoscopic or conventional surgical removal when it is entirely intramural. In the absence of accurate diagnosis, frustration is the rule and the patient history is characterized by recurrent bleeding, abnormal filling defects persisting on the hysterogram, and repetitive curetting, culminating in an unnecessary hysterectomy.
pedicle at the base either with endoscopic scissors, an electric loop, or a laser fiber (Fig. 22.8). However, when the size of the polyp is important, its resection in fragments is advisable to facilitate its extraction through the cervix. A pedunculated myoma can be managed as a polyp, but the sessile variety requires either hysteroscopic resection when the submucous component is present or laparoscopic or conventional surgical removal when it is entirely intramural. In the absence of accurate diagnosis, frustration is the rule and the patient history is characterized by recurrent bleeding, abnormal filling defects persisting on the hysterogram, and repetitive curetting, culminating in an unnecessary hysterectomy.
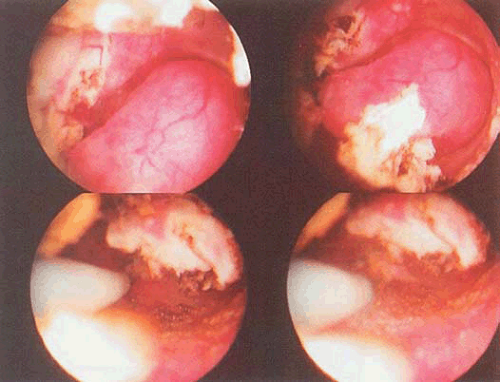 FIGURE 22.8 An endometrial polyp in the lower portion of the field. The polyp is resected using a loop electrode. |
Endometrial Polyp
Diagnosis
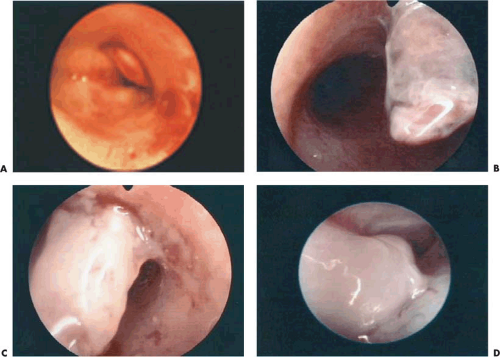
A functional polyp is lined with mucosa responsive to ovarian hormones and changing with the menstrual cycle. The structure is generally small, since it unevenly participates in menstrual shedding (Fig. 22.9A–D). Typically, the polyp is relatively broad based and soft. Its color and vasculature resemble that of the surrounding endometrium (Figs. 22.10A–C, 22.11A, B, 22.14A). It may be mistaken for an area of focal hyperplasia (Fig. 22.12A–C). Contact hysteroscopy is of great value in doubtful cases, since it demonstrates the presence of a central vascular axis and the tissue cohesion characteristic of a real polyp (Fig. 22.13A, B).
The nonfunctional polyp is insensitive to progesterone but still responds to estrogens, which support its growth. It can grow to a large size and, as its pedicle lengthens, becomes flattened between the opposing uterine walls. It may become triangular in shape. This variety of polyp is red-yellow, and its distal end is sometimes ecchymotic (Figs. 22.14B, C). CO2 gas pressure flattens it along the posterior uterine wall. Because it is very mobile, this polyp tends to slip away from the contact hysteroscope. Therefore it can be overlooked during a hasty examination with this instrument (Figs. 22.15 and 22.16A, B).
The polyp of the older woman is covered by a layer of white, atrophic endometrium (Fig. 22.17A, B). It is usually broad based, and its surface appears uneven because of small bluish translucent cysts.
Contribution of Hysteroscopy
The hysteroscopic examination permits accurate gross diagnosis. The proficient hysteroscopist can accurately anticipate the microscopic pattern, but the last word is always reserved for the pathologist. The ability to recover the entire polyp under visual control will also result in more reliable histologic examination. Blind curettage removes polyps in fragments together with strips of endometrium, making detection difficult for the pathologist. Hysteroscopy obviates the danger of overlooking adenocarcinoma developing within an initially benign polyp or spreading from a nearby endometrial area. Likewise, a thorough visual study of the uterine cavity can reveal other lesions coexisting with endometrial polyps, for example, endometrial hyperplasia or submucous myoma. Ultimately, after elective removal of a polyp, it is advisable in women older than 40 years of age to complete the procedure by a thorough sampling to make certain that no incipient lesion has been left behind. Reinsertion of the hysteroscope assures the operator that the uterus has been thoroughly emptied.
Submucous Myomas
Diagnosis
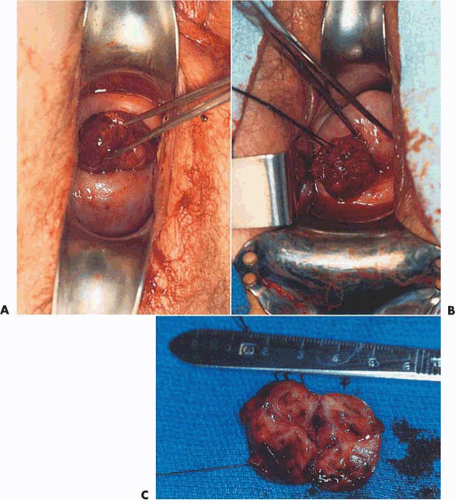
The diagnosis of a submucous myoma is usually easy. It most typically appears as a round protrusion bulging toward the uterine lumen (Fig. 22.18A, B). The overlying endometrium is often atrophic and lighter in color than the surrounding mucosa. A network of dilated vessels can be seen on its surface (Fig. 22.19A–C). Its hard consistency is demonstrated by the resistance it offers to the pressure of the hysteroscope tip. It constitutes an obstacle that cannot be pushed away but only passed around.
As the myoma becomes pedunculated its appearance is less characteristic, and its differentiation from an endometrial polyp may be difficult. When it extends toward the cervix, the myoma becomes flat and the tip appears more reddish. The intramural myoma produces a slight protrusion in the overlying endometrium, which otherwise does not differ from the surrounding mucosa. It can be easily overlooked. The asymmetric appearance of the uterine cavity when viewed from the internal os may be the only sign of this lesion.
Contribution of Hysteroscopy
Hysteroscopy is of great value for the diagnosis of submucous myoma, especially the small tumors that are consequently missed by the pelvic examination but that may cause heavy bleeding because of their intracavitary location (Fig. 22.20A–L). When hysterography is precluded because of persistent bleeding, hysteroscopy can provide an immediate diagnosis and save an unnecessary curettage. The presence of a submucous myoma can occasionally be suspected by the feel of the curette, but in most cases the diagnosis will be missed, and the abnormal bleeding will persist because the myoma has been eroded by the scraping. Sometimes a myoma is discovered by manual palpation of the uterus, but one must not be too hasty to implicate it as the cause of the
bleeding. Frequently hysteroscopy, if performed, will avoid an inaccurate diagnosis by demonstrating a coexisting abnormality within the uterine cavity, for example, endometrial hyperplasia, polyp, or carcinoma.
bleeding. Frequently hysteroscopy, if performed, will avoid an inaccurate diagnosis by demonstrating a coexisting abnormality within the uterine cavity, for example, endometrial hyperplasia, polyp, or carcinoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree