Preparation of the Gynecologist to Perform Hysteroscopy
Michael S. Baggish
Rafael F. Valle
Visual examination of the uterine cavity to detect disease dates back to the first known demonstration of hysteroscopy by Pantaleoni in 1869. Gynecologists generally have preferred blind methods of examination: tactile appraisal, exploration with forceps or curettes, and radiographic studies with radiopaque material to demonstrate any filling defects in the uterine cavity. These blind methods have limitations, however, and since the early 1970s when hysteroscopy became a practical method for intrauterine visualization, precision-oriented gynecologists have preferred to evaluate the uterine cavity hysteroscopically, with the degree of success depending on the endoscopist’s skill.
Lack of familiarity with intrauterine visualization and difficulty in obtaining satisfactory uterine distention have frustrated gynecologists in attempting to use hysteroscopy in their practice. Skillful use of hysteroscopy requires thorough training, dedication, and experience. In the past, gynecologists learned the technique by self-teaching and solved their own problems without guidelines or tutors to help them. We believe that there is a more effective and more appropriate method for learning hysteroscopy. An up-to-date textbook devoted to hysteroscopy such as this book is exceedingly valuable since it provides a rational basis for understanding the techniques, instruments, and accessory tools required to perform the operation. Additionally, the numerous clear pictures of both normal and abnormal conditions provide a perpetual reference for purposes of interpretation. The book in essence is the practitioner’s road map.
Workshops, Seminars, and Lectures
Lectures and workshops on hysteroscopy have decreased since 1999. Perhaps half a dozen are given annually. Most of these seminars are didactic and theoretical, looking at methods, results, complications, practical applications, indications, and contraindications.
The selection of the best seminar to attend should be based on the expertise of the faculty and the course content. For example, basic physics, basic methodology, distending media, instrumentation, diagnostic hysteroscopy, operative hysteroscopy, and laser and electrosurgical hysteroscopy should be detailed, and the seminar should include video sessions showing actual procedures. Few courses nowadays have a hands-on component.
This hands-on or workshop experience should allow the physician to assemble various instruments and use uterine models to become familiar with the direct and fore-oblique views. Such exercises permit a wide variety of equipment to be used in a concentrated time period. Additionally, a substantial number of experienced hysteroscopists should be available to answer questions and demonstrate techniques.
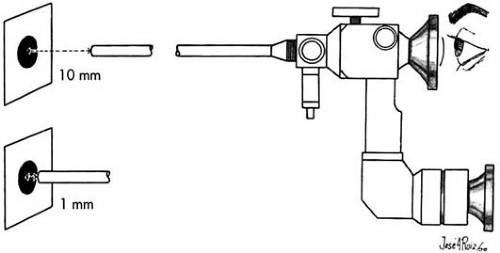 FIGURE 13.1 Objects of known sizes are examined at various distances from the terminus of the endoscope. |
The novice should not improvise, but rather, should learn one method until proficient, beginning with diagnostic procedures and advancing to therapeutic ones. From easy therapeutic procedures such as removal of endometrial polyps, removal of misplaced intrauterine foreign bodies, or targeted biopsies, the surgeon may progress to more difficult and complex operations.
Preceptorships
Ideally, this technique is best learned by performing endoscopy under the guidance of an expert who can correct mistakes and encourage success. Minimally, the new hysteroscopist should proceed in the same vein as a resident, i.e., performing the hysteroscopy with an experienced surgeon scrubbed in and assisting. Preceptor training is available in most major hospitals, where usually at least one physician has experience performing hysteroscopy. Under circumstances where no local hysteroscopy expertise is available, course directors may help by offering visiting hysteroscopy preceptorships. In the latter circumstance, one or more inexperienced surgeons are supervised in their own hospital by the visiting expert hysteroscopic surgeon.
Where to Begin
Familiarization with instruments is a key factor in learning any new technique. Examine objects of known sizes and shapes at distances from 2 cm to 1 to 2 mm from the terminus of the endoscope (Fig. 13.1). Do this examination with both 30-degree and 0-degree telescopes. Next, repeat the examination in a glass container-first using air, then water, then Hyskon. Drop a coin into the glass (Fig. 13.2) and examine the detailed etchings and inscriptions on the coin after attaching the fiberoptic light cable to the hysteroscope and connecting it in turn to the light generator. Settings should be made with different powers ranging from low- to high-intensity illuminations. Next, attempt these examinations first with a diagnostic sheath, then with various operating sheaths.
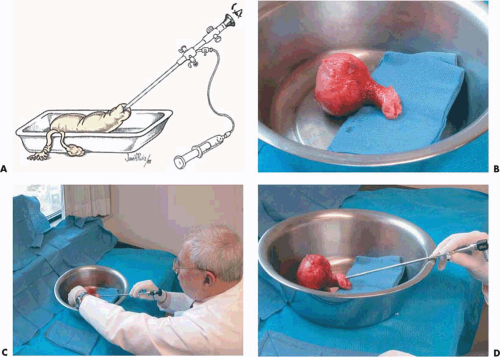
The most valuable and practical model on which to practice diagnostic and operative panoramic hysteroscopy is an extirpated human uterus (Fig. 13.3A). The best uterus to examine is a normal uterus; these are readily available following surgery (vaginal or abdominal hysterectomy) for the correction of pelvic relaxation and/or stress incontinence. The specimen should be placed in saline within a deep pan and secured in a timely fashion following the operative procedure (Fig. 13.3B). Obviously, removal of the specimen should be coordinated with the Department of Pathology beforehand. Additionally, in the present climate of sexually transmitted diseases, a negative serologic report for syphilis and human immunodeficiency virus is recommended. In fact, because of acquired immunodeficiency syndrome (AIDS) risk, the practice of using human specimens for exercises during hysteroscopy didactic courses should be abandoned (Fig. 13.4). Once a specimen has been obtained, examination should be performed with the hysteroscope fitted with a 5-mm diagnostic sheath. Water is used to distend the uterus and is delivered to the sheath via a 500-mL bag or bottle hung from an IV pole (Fig. 13.3C, D).
Recently a latex model has been devised that includes specimens with polyps, myomas, and other pathology (Fig. 13.4A–C). The device includes a flushing reservoir and drainage tube (Limbs and Things, Bristol, England) and is ideal for practicing diagnostic hysteroscopy using water (Fig. 13.5). The model is portable and may be used in almost any location (Fig. 13.6A, B). Most hands-on courses use cow uteri or pig bladders as models for practicing operative hysteroscopy with lasers or electrosurgical devices. Hyskon is a convenient source of medium for these animal uteri (Fig. 13.7).
Hysteroscopy Performed on a Living Patient
The best learning experience is obtained performing a diagnostic hysteroscopy with a patient under general anesthesia.
The important parameters, which can be learned only in these circumstances, are (a) the assembly of the hysteroscope and sheath, (b) purging air from the assembled telescope and sheath with the infusing medium, and (c) insertion through the cervix into the corpal cavity via video navigation.
The important parameters, which can be learned only in these circumstances, are (a) the assembly of the hysteroscope and sheath, (b) purging air from the assembled telescope and sheath with the infusing medium, and (c) insertion through the cervix into the corpal cavity via video navigation.
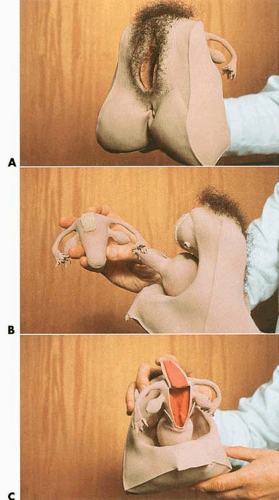 FIGURE 13.4 A: A latex rubber model of the human vagina and uterus. The vulva is also lifelike. B: The detachable uterus is anatomically accurate and is useful for practicing endoscopic observation and orientation. C: The uterus may be repeatedly hemisected for direct viewing.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|