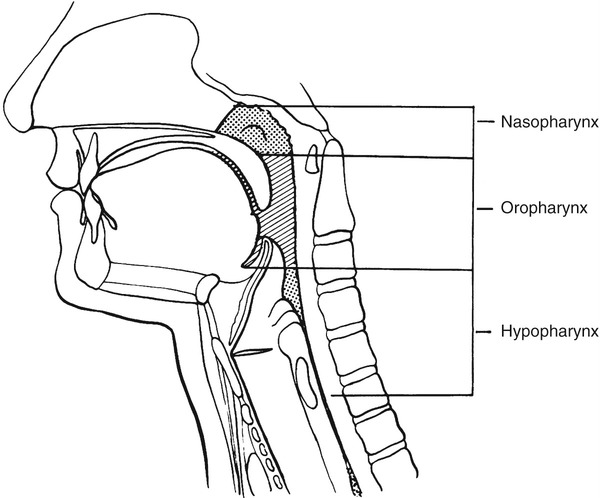
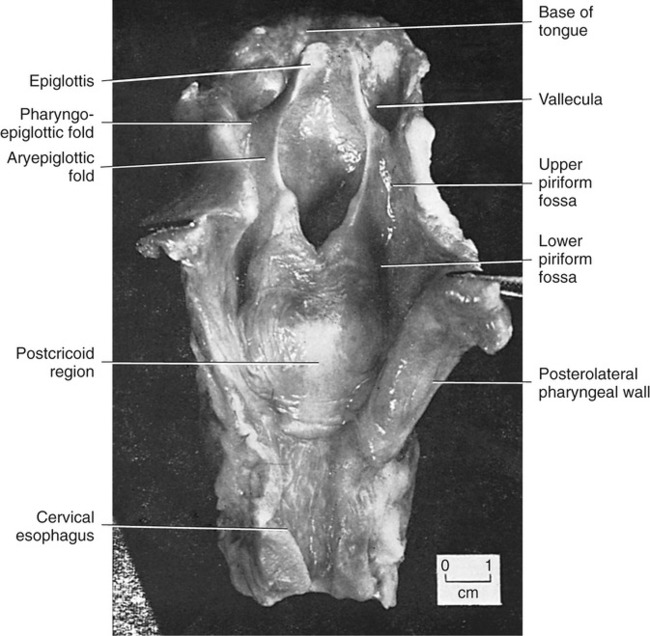
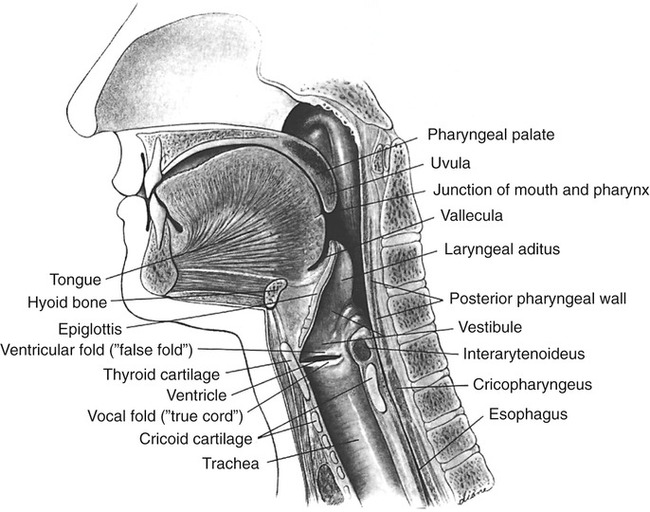
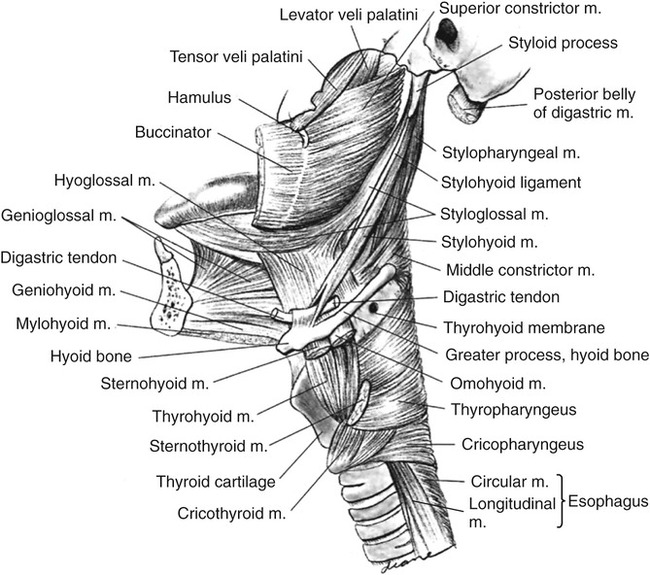
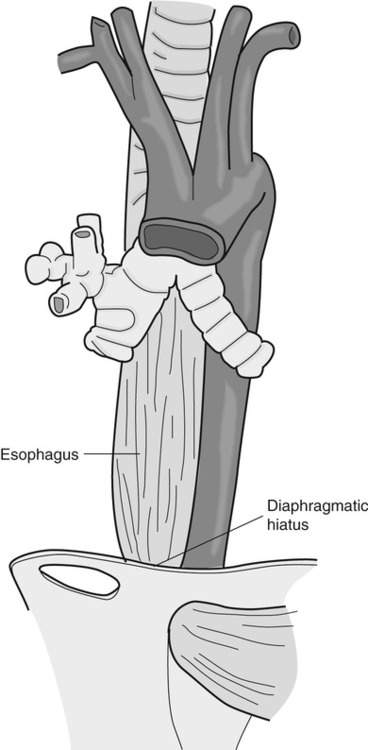
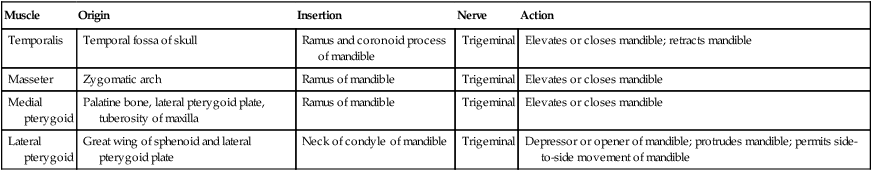
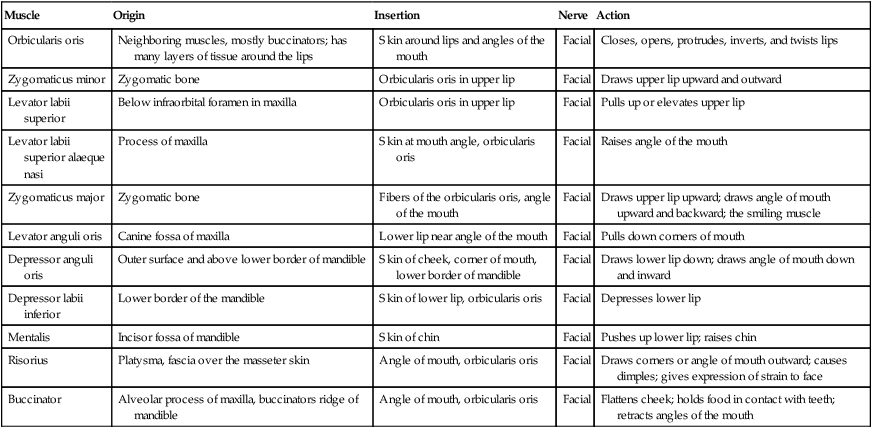
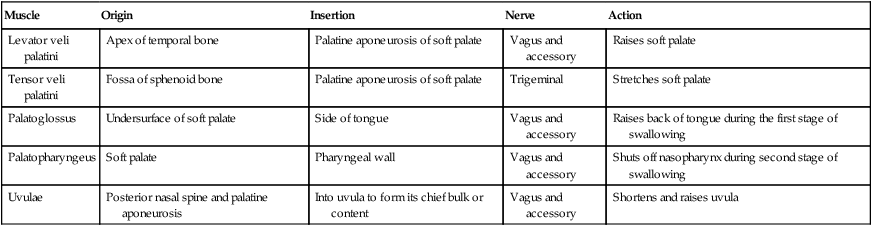
1. Define the key anatomic structures involved in swallowing. 2. Define the groups of muscles that participate in swallowing. 3. Define the peripheral and central neurologic controls for swallowing. 4. Discuss the key physiologic components that occur when moving a bolus from the mouth to the stomach. 5. Discuss how normal swallowing is affected by bolus type and delivery. Normal swallowing includes an integrated, interdependent group of complex feeding behaviors emerging from interacting cranial nerves of the brainstem and governed by neural regulatory mechanisms in the medulla, as well as in sensorimotor and limbic cortical systems. Healthy individuals simultaneously perform the sequential sensory and motor patterns of mastication and swallowing with little effort and conscious awareness. For purposes of simplification, such sensory-guided discriminatory feeding and sensory-cued, stereotyped swallowing behaviors usually are divided into four stages (Practice Note 2-1): (1) the oral preparatory stage, in which food is masticated in preparation for transfer; (2) the oral stage, which entails the transfer of material from the mouth to the oropharynx; (3) the pharyngeal stage, in which material is transported away from the oropharynx, around an occluded laryngeal vestibule, and through a relaxed cricopharyngeus muscle into the upper esophagus; and (4) the esophageal stage, in which material is transported through the esophagus into the gastric cardia. An additional stage of swallowing that precedes the oral stage has been proposed by Leopold and Kagel,1 who argue that visual appreciation of the bolus before its placement in the oral cavity may send a cognitive message that may help stimulate saliva during bolus preparation. The oral cavity extends from the lips anteriorly to the nasopharynx posteriorly and contains the tongue, gums, and teeth. The oral cavity is separated from the nasal cavity by the bony palate and velum (soft palate). It is composed of a highly mobile lower jaw, or mandible, consisting of a U-shaped body containing important ridges for muscle attachments. The upper jaw, or maxilla, meets the zygomatic or cheek bone and is adjoined by the L-shaped palatine bones, lying posterior to the nasal cavity. The perpendicular part of the palatines forms the back of the nasal cavity, whereas the horizontal part forms the back of the bony palate. The velum and posterior nasopharyngeal wall seal and open communication between the nasal and oral cavities during swallowing and respiratory behaviors, respectively. The nasopharynx lies above the velum, and the oropharynx lies posterior to the mouth. The pharynx extends below to the esophagus; its inferior portion is called the hypopharynx and is separated from the esophagus by the cricopharyngeal muscle (Figure 2-1). The cartilaginous larynx lies anterior to the hypopharynx at the upper end of the trachea, suspended by muscles attached to the hyoid bone. The cricoid cartilage lies above the trachea, with the thyroid cartilage above it. Both are suspended from muscles attached to the hyoid bone, which itself is suspended between the jaw, tongue, and sternum by suprahyoid and infrahyoid musculature. The valleculae are lateral recesses at the base of the tongue on each side of the epiglottis. The piriform sinuses are lateral recesses between the larynx and the anterior hypopharyngeal wall (Figure 2-2). These recesses serve as important anatomic landmarks in the videoradiographic assessment of pharyngeal swallow. Figure 2-3 shows a lateral view of the key anatomic structures in the region of the head and neck. The mandibular branch of the trigeminal nerve (cranial nerve [CN] V) innervates the principal muscles for chewing behaviors. The primary muscles of chewing are the masseter, temporalis, and pterygoid muscles, which attach to the sphenoid wing of the temporal bone. The masseter closes the jaw while the temporalis moves it up, forward, or backward (Table 2-1). The medial pterygoid muscles work bilaterally to elevate the mandible while they shift the jaw to the opposite side unilaterally. The lateral pterygoid muscles work together, pulling down or forward while moving the jaw or chin to the opposite side unilaterally. Both sets of pterygoid muscles cooperate to grind in mastication. TABLE 2-1 The facial nerve (CN VII) innervates lower facial muscles attached to the maxillae and mandible of the skull. These include the buccinator muscles, which compress the lips and flatten the cheeks in the movement of food across the teeth (Table 2-2). The buccinator fibers blend with those of the orbicularis oris, the sphincter of the lips. TABLE 2-2 In the nasopharynx, five muscles adjust the position of the velum with respect to the food bolus: the palatoglossal and levator veli palatini muscles (pharyngeal plexus and accessory nerve), which elevate the soft palate and seal the nasopharynx; the tensor veli palatini (mandibular branch of the trigeminal nerve), which tenses the palate and dilates the orifice of the eustachian tube; the palatopharyngeal muscle (pharyngeal plexus and spinal accessory nerve), which depresses the soft palate, approximates the palate or pharyngeal folds, and constricts the pharynx; and the muscularis uvula (spinal accessory nerve), which shortens the soft palate (Table 2-3). TABLE 2-3 The hypoglossal (CN XII), trigeminal (CN V), and facial (CN VII) nerves innervate the suprahyoid group of muscles. The hypoglossal nerve supplies the geniohyoid, which draws the hyoid bone up and forward, depressing the jaw, and the trigeminal nerve supplies the mylohyoid, which elevates the hyoid bone and tongue and depresses the jaw (Table 2-4). The digastric muscles contain anterior and posterior bellies. The anterior belly is innervated by the mandibular branch of the trigeminal nerve (CN V) and depresses the jaw or raises the hyoid bone, whereas the posterior portion is innervated by the facial nerve (CN VII) and elevates or retracts the hyoid. The facial nerve (CN VII) innervates the stylohyoid muscle, which elevates the hyoid bone during swallowing. In addition, the hyoglossus and the genioglossus serve as laryngeal elevators, as well as extrinsic tongue muscles, and are designed to depress the tongue or help elevate the hyoid bone when the tongue is fixed. The accessory nerve (CN XI), in association with the hypoglossal (CN XII) nerve, innervates the styloglossus, which draws the tongue up and back during swallowing. The glossopharyngeal (CN IX) and accessory (CN XI) nerves also cause the palatoglossus to raise the back of the tongue and lower the velum. The styloglossus and palatoglossus raise the back of the tongue and lower the sides of the soft palate. TABLE 2-4 The cricopharyngeal muscle is an important single muscle that lies at the transition level between the pharynx and the esophagus. Functionally, it is separate from both the pharynx and the esophagus and acts as a sphincter, relaxing during passage of the bolus from the pharynx into the esophagus. It is innervated by both pharyngeal branches of the vagus and sympathetic fibers from the middle and inferior cervical ganglia. The key muscles used in the oral and pharyngeal stages of swallowing are shown in Figure 2-4. The esophagus is a distensible tube, approximately 21 to 27 cm (10 inches) long, connecting the pharynx (at C6) and stomach (at T12). It is separated from the pharynx by the pharyngeal esophageal segment (PES) and from the stomach by the lower esophageal sphincter (LES). Under resting conditions, the esophageal lumen is collapsed, creating a potential space that can easily distend up to 3 cm to accommodate swallowed air, liquids, or solids. The esophagus is lined with a protective, stratified, squamous epithelium that covers an inner layer of circular fibers and an outer layer of longitudinal fibers. At its proximal end (upper fourth) the muscle is striated, whereas the distal two thirds are composed of smooth muscle. The middle third, in the region of the aorta, is a combination of smooth and striated muscle. As it courses through the thorax at the level of the carina, the esophagus runs lateral and posterior to the left ventricle of the heart, creating a natural bend as it courses anteriorly toward the diaphragmatic hiatus. After passing the diaphragmatic hiatus, it connects to the body of the stomach at the level of the LES. The smooth muscle of the LES is arranged in a specialized spiral configuration as it joins the inner oblique muscle zone of the stomach. The relation of the esophagus to the heart and tracheobronchial tree, as well as its path through the diaphragmatic hiatus, is shown in Figure 2-5. Many studies have examined the normal aspects of the oropharyngeal swallow sequence. The rationale usually given for such studies is that clinicians must be able to compare normative data with patient data to determine whether an abnormality exists. Although this approach to detection has heuristic appeal, studies of the normal swallow have revealed significant variability among normal (healthy) subjects, particularly in the oral preparatory and oral stages of swallowing.2–5 Part of this variability is attributable to subject selection, bolus type, and the tools used to measure swallow performance. Other variability seems inherent in the swallowing process. It appears that the mechanism for swallowing must be variable to accommodate the variations of bolus type and amount for successful ingestion in different circumstances of eating, such as eating while talking, in varied environments, and at various rates. The astute clinician will not ignore those aspects of normal swallow performance that have been empirically evaluated but should also be imminently cognizant of placing a person’s functional swallow in the context of his or her swallowing complaint, past medical history, and the results of physical and instrumental examinations. Normal swallowing performance depends on the rapid transfer of the bolus from the oral cavity to the stomach. A liquid bolus may pass through the pharynx within 2 seconds and enter the stomach in less than 5 seconds. Efficient movement is accomplished by the strength of the neuromuscular contraction exerted on the bolus and on the forces of gravity. Efficient bolus movement is accomplished when coordinated neuromuscular contractions and relaxations create zones of high pressure on the bolus and zones of negative pressure below the level of the bolus. Some parts of the swallowing chain, such as the esophagus, remain under negative pressure because of their location. Creating zones of high and low pressure is largely accomplished by the coordination and strength of the swallowing valves: lips, velum, airway closure, PES opening and closing, and upper esophageal sphincter (UES) opening and closing. A patent nasal airway also may be important (Practice Note 2-2). The tongue provides the initial positive driving force. The tongue’s posterior deflection provides the basis for laryngeal elevation by applying traction to the hyoid bone. Efficient (i.e., timely and strong) laryngeal elevation helps create a negative zone of pressure in the pharynx, particularly in the region of the PES. This allows the bolus to move rapidly, and therefore safely, from a zone of high pressure into a zone of negative pressure. Moving from a zone of high pressure into another zone of high pressure caused by a pathologic condition (e.g., muscle weakness or incoordination) inhibits bolus flow and results in stasis and residue that may be aspirated into the airway. Food or liquid in the mouth stimulates taste, temperature, and pressure (touch) receptors. The primary receptors of taste are located on the tongue, on the hard and soft palate, in the pharynx, and in the supralaryngeal region. The receptors are activated by saliva. Saliva is produced by the activation of the submandibular, submaxillary (autonomic aspects of CN VII), and parotid glands (autonomic aspects of CN IX). Activation of these glands is achieved by the actions of the jaw, tongue, and hyoid bone during bolus preparation and by the inherent taste of the bolus. The primary sensory receptors on the dorsum of the tongue responsible for the perception of salt, sweet, sour, and bitter are activated by saliva. In addition to facilitating taste and bolus formation, saliva is important in the maintenance of adequate oral hygiene by controlling microorganisms, in the regulation of the acidity levels in the stomach and esophagus because of it bicarbonate composition, and in the breakdown of carbohydrates. The number of times a person swallows saliva in 1 hour can vary between 18 and 400 and largely depends on the rate of salivary flow.6 Sensations of taste are carried by the chorda tympani branch of CN VII on the anterior two thirds of the tongue and through the greater petrosal branch on the hard and soft palate. Taste on the posterior third of the tongue is mediated by CN IX. Sensations of taste are sent to the nucleus tractus solitarii (NTS) in the medulla of the brainstem (see sections on neurologic controls), where they are transmitted to the sensorimotor cortex by the thalamus. Taste receptors in the region of the laryngeal aditus are carried to the NTS by the superior laryngeal branch of CN X. Appreciation of taste depends largely on smell. Smell sensations are carried by direct stimulation of the nasal cavity and by smell elicited by chewing, during which odors travel posteriorly into the nasopharynx. Interpretation of smell is ultimately accomplished through the thalamus to the frontal and temporal cortices by information carried by CN I. Information (memories) relating to smell may be stored in the hippocampus. The coordinated action of the tongue and jaw moves a bolus laterally onto the molar table for deformation. Further deformation is accomplished by variable contacts of the tongue to the hard palate. Although the tongue may play a large role in containing the bolus in the oral cavity before swallow, evidence indicates that during solid bolus mastication, material is allowed to collect in the vallecular recesses at the tongue base before swallow initiation.5 The ultimate role of the tongue is to manipulate, shape, hold, and then transfer the bolus into the oropharynx, signaling the onset of the oral stage of swallow as the swallowing sequence transitions into the pharyngeal stage with the passage of the bolus through the oropharyngeal port. The exact nature of the sensory cues that signal a bolus is ready for swallowing is not completely understood; however, studies have shown that the superior laryngeal nerve branch of the vagus is important in swallow initiation7 and in the sensory protective mechanisms of the upper airway.8 The mechanics of bolus preparation can be appreciated with videofluoroscopy. The first images are taken as the patient faces the camera and chews a piece of cracker (Video 2-1). The undulating and varied movements of the tongue and jaw are apparent. In the lateral view, the tongue can be seen touching the hard palate as material is pushed toward the tongue base, filling the valleculae before the swallow (Video 2-2). Once the bolus is prepared, the tongue tip is elevated to occlude the anterior oral cavity at the alveolar ridge, and the bolus is held against the hard palate. The edges of the tongue dorsum contain the bolus laterally. The tongue tip and dorsum appear to work longer in containment activity than the posterior tongue after the oral stage is initiated; however, the posterior tongue is more responsible for delivering the bolus into the pharynx.9 Before—but almost simultaneous with—the first posterior movement of the tongue, respiration ceases (see following section on respiration), followed by arytenoid cartilage approximation precipitating true vocal fold adduction. Retraction of the tongue is primarily accomplished by extrinsic tongue muscles: digastricus (CN V), mylohyoid (CN V), and the geniohyoid (CN XII). The tongue base applies positive pressure to the tail of the bolus by its contact with the velum and posterior pharyngeal wall, which allows the bolus to move rapidly through the pharynx into an open PES. As the tongue propels the bolus posteriorly, the palatopharyngeal folds are pulled medially to form a slit through which the bolus can pass. The levator veli palatinii muscles help elevate the velum to seal the nasopharyngeal opening. The combined action of the tongue’s contact to the velum and posterior pharyngeal wall and sealing the nasopharynx contribute to the maintenance of positive pressure on the bolus as it moves toward zones of negative pressure in the hypopharynx. By the tongue’s connections to the hyoid bone, and the hyoid bone’s connections to the thyroid and cricoid cartilages, the larynx is pulled up and forward, resting under the tongue base that now partially covers the opening to the airway. As the larynx rises, the cartilaginous epiglottis makes its descent over the top of the airway, completing an elaborate system of airway protection that allows the bolus to be directed toward the esophagus rather than into the trachea. The extent of epiglottic descent depends on anterior hyoid displacement, tongue base retraction force, and bolus size.10 Rapid and complete laryngeal elevation (2 to 3 cm on average) aids in creating negative pressure in the region of the hypopharynx. As the bolus enters the pharynx, it is divided by the vallecular spaces at the level of the tongue base, helping deflect it away from the airway as an additional component of airway protection.
Normal Swallowing in Adults
NORMAL ANATOMY
Oral Preparatory Stage
Muscle
Origin
Insertion
Nerve
Action
Temporalis
Temporal fossa of skull
Ramus and coronoid process of mandible
Trigeminal
Elevates or closes mandible; retracts mandible
Masseter
Zygomatic arch
Ramus of mandible
Trigeminal
Elevates or closes mandible
Medial pterygoid
Palatine bone, lateral pterygoid plate, tuberosity of maxilla
Ramus of mandible
Trigeminal
Elevates or closes mandible
Lateral pterygoid
Great wing of sphenoid and lateral pterygoid plate
Neck of condyle of mandible
Trigeminal
Depressor or opener of mandible; protrudes mandible; permits side-to-side movement of mandible
Muscle
Origin
Insertion
Nerve
Action
Orbicularis oris
Neighboring muscles, mostly buccinators; has many layers of tissue around the lips
Skin around lips and angles of the mouth
Facial
Closes, opens, protrudes, inverts, and twists lips
Zygomaticus minor
Zygomatic bone
Orbicularis oris in upper lip
Facial
Draws upper lip upward and outward
Levator labii superior
Below infraorbital foramen in maxilla
Orbicularis oris in upper lip
Facial
Pulls up or elevates upper lip
Levator labii superior alaeque nasi
Process of maxilla
Skin at mouth angle, orbicularis oris
Facial
Raises angle of the mouth
Zygomaticus major
Zygomatic bone
Fibers of the orbicularis oris, angle of the mouth
Facial
Draws upper lip upward; draws angle of mouth upward and backward; the smiling muscle
Levator anguli oris
Canine fossa of maxilla
Lower lip near angle of the mouth
Facial
Pulls down corners of mouth
Depressor anguli oris
Outer surface and above lower border of mandible
Skin of cheek, corner of mouth, lower border of mandible
Facial
Draws lower lip down; draws angle of mouth down and inward
Depressor labii inferior
Lower border of the mandible
Skin of lower lip, orbicularis oris
Facial
Depresses lower lip
Mentalis
Incisor fossa of mandible
Skin of chin
Facial
Pushes up lower lip; raises chin
Risorius
Platysma, fascia over the masseter skin
Angle of mouth, orbicularis oris
Facial
Draws corners or angle of mouth outward; causes dimples; gives expression of strain to face
Buccinator
Alveolar process of maxilla, buccinators ridge of mandible
Angle of mouth, orbicularis oris
Facial
Flattens cheek; holds food in contact with teeth; retracts angles of the mouth
Oral/Pharyngeal Stage
Muscle
Origin
Insertion
Nerve
Action
Levator veli palatini
Apex of temporal bone
Palatine aponeurosis of soft palate
Vagus and accessory
Raises soft palate
Tensor veli palatini
Fossa of sphenoid bone
Palatine aponeurosis of soft palate
Trigeminal
Stretches soft palate
Palatoglossus
Undersurface of soft palate
Side of tongue
Vagus and accessory
Raises back of tongue during the first stage of swallowing
Palatopharyngeus
Soft palate
Pharyngeal wall
Vagus and accessory
Shuts off nasopharynx during second stage of swallowing
Uvulae
Posterior nasal spine and palatine aponeurosis
Into uvula to form its chief bulk or content
Vagus and accessory
Shortens and raises uvula
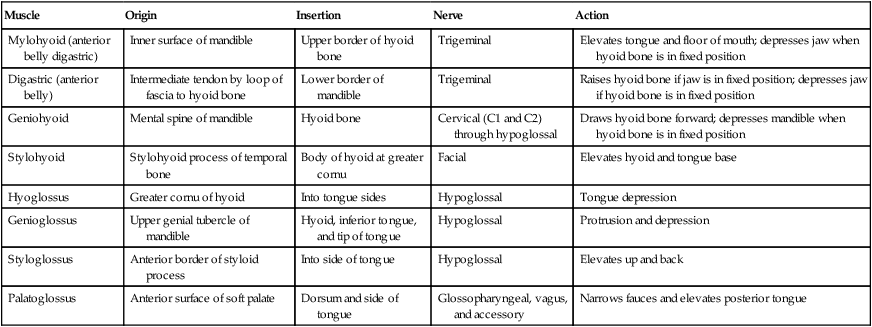
Muscle
Origin
Insertion
Nerve
Action
Mylohyoid (anterior belly digastric)
Inner surface of mandible
Upper border of hyoid bone
Trigeminal
Elevates tongue and floor of mouth; depresses jaw when hyoid bone is in fixed position
Digastric (anterior belly)
Intermediate tendon by loop of fascia to hyoid bone
Lower border of mandible
Trigeminal
Raises hyoid bone if jaw is in fixed position; depresses jaw if hyoid bone is in fixed position
Geniohyoid
Mental spine of mandible
Hyoid bone
Cervical (C1 and C2) through hypoglossal
Draws hyoid bone forward; depresses mandible when hyoid bone is in fixed position
Stylohyoid
Stylohyoid process of temporal bone
Body of hyoid at greater cornu
Facial
Elevates hyoid and tongue base
Hyoglossus
Greater cornu of hyoid
Into tongue sides
Hypoglossal
Tongue depression
Genioglossus
Upper genial tubercle of mandible
Hyoid, inferior tongue, and tip of tongue
Hypoglossal
Protrusion and depression
Styloglossus
Anterior border of styloid process
Into side of tongue
Hypoglossal
Elevates up and back
Palatoglossus
Anterior surface of soft palate
Dorsum and side of tongue
Glossopharyngeal, vagus, and accessory
Narrows fauces and elevates posterior tongue
Esophageal Stage
NORMAL PHYSIOLOGY
Oral Preparation
Oral Stage
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Abdominal Key
Fastest Abdominal Insight Engine