Fig. 31.1
Trocar placement for a conventional laparoscopic-assisted procedure
When a HALS procedure is planned, only two 5-mm trocars are placed in the right and left lower quadrants. After feasibility of the laparoscopic approach is confirmed, a Pfannenstiel incision is performed two fingerbreadths above the pubis. The pneumoperitoneum is evacuated, and the hand-assisted device is inserted and secured in placed (Fig. 31.2). When feasible, the future ileostomy site is used as one of the port sites.
Fig. 31.2
Trocar placement for a HALS procedure
Step 2: Mobilization of the Intra-Abdominal Colon
Pneumoperitoneum is reestablished and the patient is placed in reverse Trendelenburg and right lateral decubitus position. The surgeon stands between the patient’s legs, with the camera operator being typically on the left side of the patient holding a 30° 5 mm scope. The ligament of Treitz is identified, and the small intestine is evaluated in its entirety, to rule out unexpected small bowel disorders or abnormalities that may preclude pouch construction. The small intestine is placed in the left upper quadrant away from the operating field, thus facilitating the initial mobilization of the ileocolic vascular pedicle. The surgeon moves to the patient’s left side next to the camera operator, the assistant stands on the patient’s left side, and the patient is placed in steep Trendelenburg and left lateral decubitus position to keep the small bowel out of the operating field. The ileocolic vascular pedicle is then identified, placed under tension, dissected, and divided with a vessel-sealing device. While we try to preserve the terminal ileal branches, we do not divide the ileocolic pedicle close to the bowel. Next, medial to lateral mobilization of the ascending colon is completed all the way up to the hepatic flexure in the submesenteric avascular plane. Attention is then directed to the lateral peritoneal attachments, which are taken down from the hepatic flexure to the cecum (Fig. 31.3). With the surgeon now on the patient’s right side, the operating table is placed in reverse Trendelenburg and the transverse colon is mobilized from the hepatic to the splenic flexure by sequentially dividing the greater omentum just distal to the gastroepiploic arcade and the transverse mesocolon (Figs. 31.4, 31.5a, b and 31.6). The omentum is taken with the specimen, thus facilitating the dissection. The splenic flexure is taken down bluntly and sharply usually in an antegrade fashion, but in difficult cases, a combination of antegrade (from the transverse colon) and retrograde (from the descending colon) mobilization is sometimes needed. At this point, the surgeon is operating between the patient’s legs. The descending colon is mobilized all the way to the level of the sigmoid colon by sequentially dividing and ligating the lateral attachments and the mesentery (Fig. 31.7). At this point, pneumoperitoneum is evacuated and the specimen is exteriorized through the Pfannenstiel incision with a wound protector in place. The terminal ileum is dissected off of the mesentery and divided with a GIA stapler. An end ileostomy is matured.
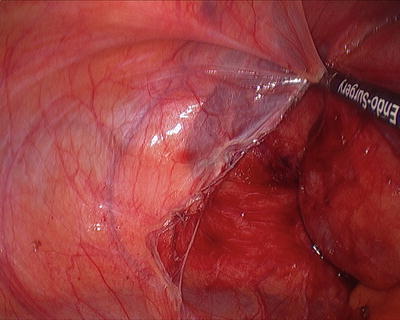
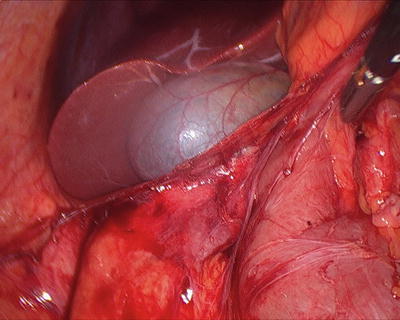
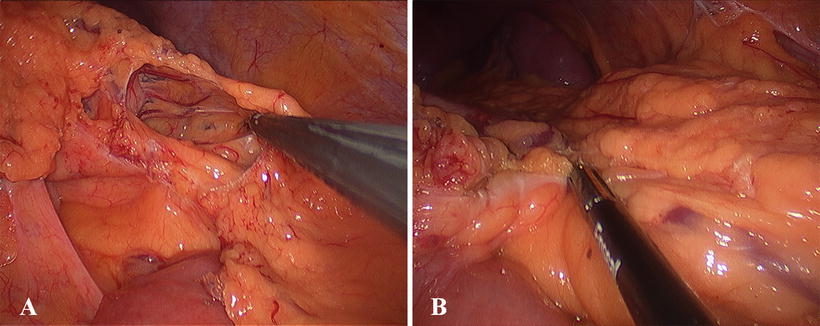
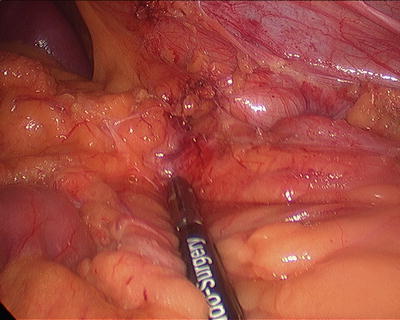
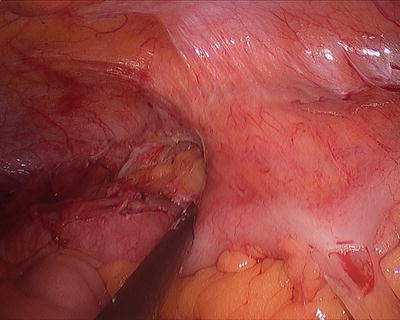
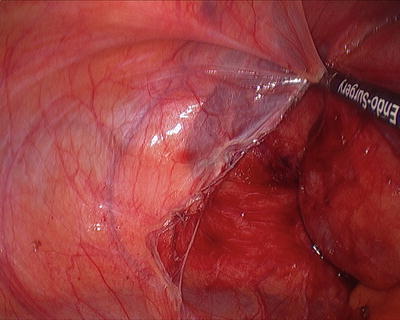
Fig. 31.3
Mobilization of the ascending colon
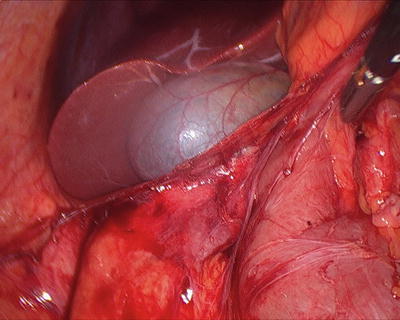
Fig. 31.4
Mobilization of the hepatic flexure
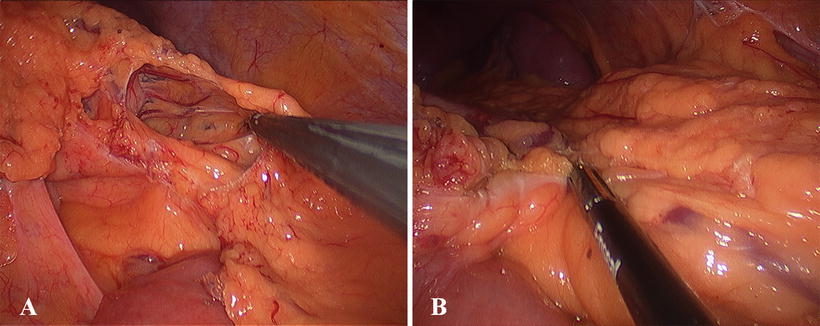
Fig. 31.5
Mobilization of the transverse colon: (a) opening of the gastrocolic ligament; (b) division of the gastrocolic ligament
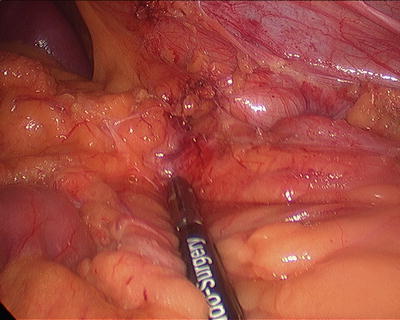
Fig. 31.6
Takedown of the splenic flexure
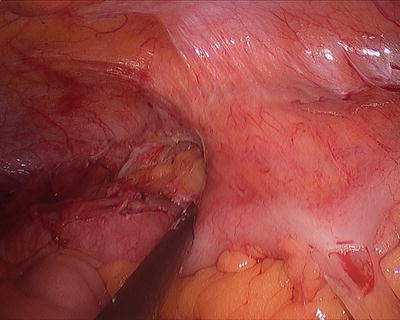
Fig. 31.7
Mobilization of the descending colon
Completion Proctectomy with IPAA
A completion proctectomy with IPAA and loop ileostomy is the second step of our staged approach.
Step 1: Positioning of the Patient, Placement of Trocars, and Exploration
The positioning of the patient is the same as for a total abdominal colectomy.
A circular incision is made around the ileostomy. The ileum is separated from its attachments to the subcutaneous tissue and fascia. The most distal ileum is then transected with a GIA stapling device. Through the ileostomy site, a 12-mm port is placed.
After exploration of the abdominal cavity, additional four 5-mm trocars are placed in each of the four abdominal quadrants as for a laparoscopic-assisted total colectomy.
Step 2: Mobilization of the Small Bowel Mesentery
With the surgeon typically between the patient’s leg and with the table in reverse Trendelenburg, the root of the mesentery of the small intestine is lifted off the retroperitoneum all the way to the third portion of the duodenum to allow a tension-free ileoanal anastomosis (Video 31.1). The avascular plane is easily identified and developed.
Step 3: Pelvic Dissection
The monitors are positioned at the foot of the table. The surgeon is on the patient’s right side with the assistant on the opposite side retracting the rectum up and out of the pelvis.
The Hartmann’s pouch is identified. The left and right ureters are identified and preserved. The superior rectal vessels are identified and divided with a vessel-sealing device. The hypogastric plexus is also identified and preserved. Only after these structures have been identified, a total mesorectal excision plane is then entered. Even for benign disease, we prefer to follow this plane of dissection because it allows for a precise and bloodless rectal mobilization. Care is taken to identify the neurovascular bundles bilaterally (Fig. 31.8). The dissection proceeds initially posteriorly, then laterally, finally anteriorly. Effort is made to dissect the rectum posteriorly all the way to the levators at the pelvic floor. Then, the lateral rectal stalks, often including the middle rectal artery, are divided all the way to the levators, and finally the anterior dissection is completed, in a male patient posterior to Denonvilliers’ fascia. At this point, when the rectum is adequately mobilized distally, the pneumoperitoneum is evacuated. The rectum will be divided at the pelvic floor either with a stapler, in the case of a stapled IPAA, or sharply in case of mucosectomy and handsewn IPAA.
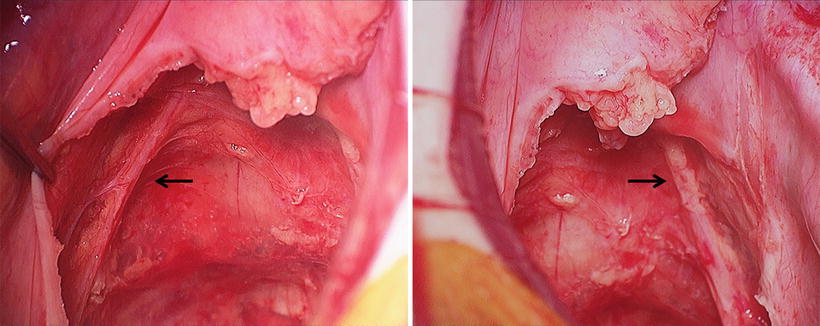
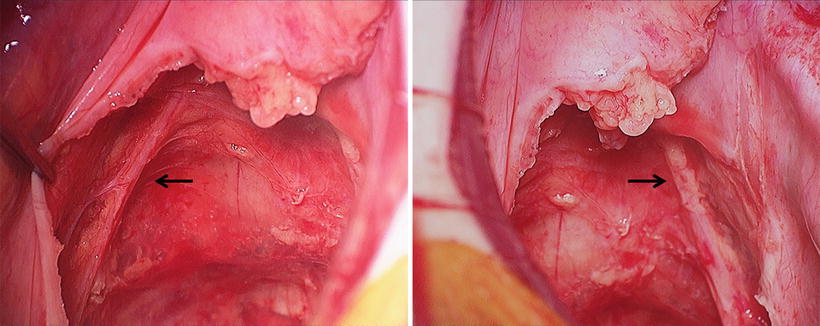
Fig. 31.8
Hypogastric nerves
Step 4: Construction of the Ileoanal Pouch
Several pouch designs have been described, but it is our practice to perform a J-pouch. Handsewn IPAA with a transanal mucosectomy starting at the dentate line is reserved in our practice in case dysplasia is demonstrated by endoscopic biopsy irrespective of location and severity [9], while stapled IPAA is performed for the majority of patients without dysplasia.
The terminal ileal mesentery is then properly oriented and the most dependent loop of small bowel identified. A 3-0 silk 30-in. long suture is placed at the apex (Fig. 31.9), and the two loops are approximated with 4-0 nonabsorbable sutures (Fig. 31.10). The abdominal cavity is protected with moist laparotomy pads. and a bowel clamp is placed on the proximal small bowel. Enterotomies on the two loops are performed. The pouch is constructed as previously described [10]. Sequential fires of an 80-mm GIA stapler are applied through the enterotomies (Figs. 31.11 and 31.12), and the pouch is progressively everted as stapling progresses toward the apex of the pouch for accurate placement of the rows of staples as well as to achieve hemostasis (Fig. 31.13). When the pouch is completely constructed, it is inverted back (Fig. 31.14) and the two enterotomies are closed in layers. By using this technique, the apex of the pouch, the future site of the anastomosis, is not manipulated or traumatized. When performing a stapled ileoanal anastomosis, the anvil is placed at the apex of the pouch, and a standard double-stapled end-to-end anastomosis is constructed with an EEA stapler. For a hand sewn IPAA, a completion mucosectomy is performed transanally. The submucosa of the residual distal rectum and anal transition zone is infiltrated with epinephrine containing local anesthetic solution to facilitate hemostasis. The circumferential mucosectomy is facilitated by placing a Lone Star™ (Lone star Co, Stafford, TX) retractor (Fig. 31.15). The internal sphincter is visualized and preserved circumferentially, and given the typically short remnant, there is no need for anal dilation or aggressive manipulation of the sphincter complex. The electrocautery is our preferred tool for a precise and hemostatic complete mucosectomy starting at the dentate line. The pouch is then carefully advanced to the pelvis (Fig. 31.16), and after adequate hemostasis, a two-layer interrupted pouch anal anastomosis is constructed (Fig. 31.17). The anastomosis is checked with a flexible sigmoidoscope for hemostasis and patency and a leak test of the anastomosis is performed. A pelvic drain is seldom necessary.
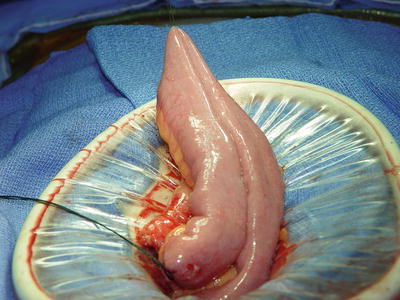
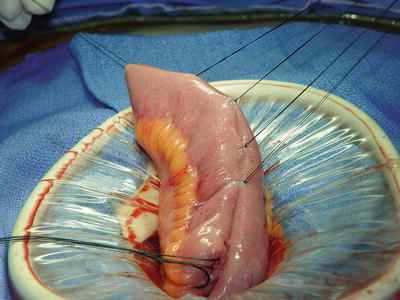
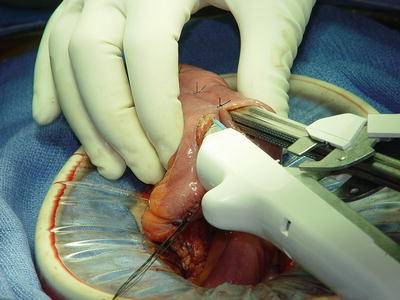
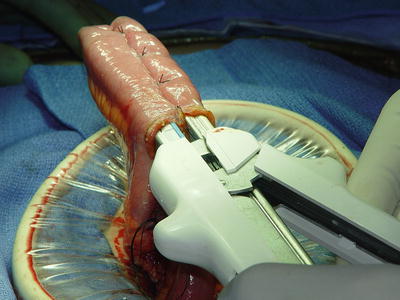
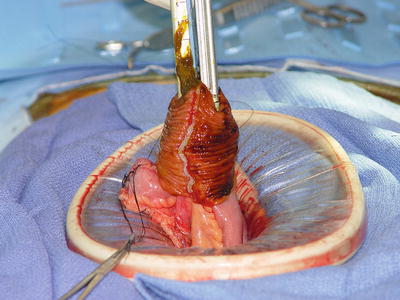
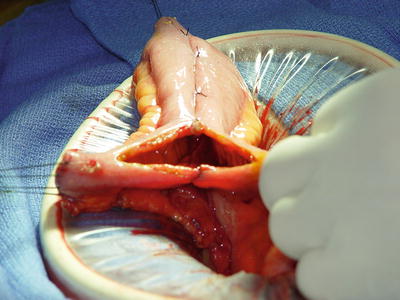
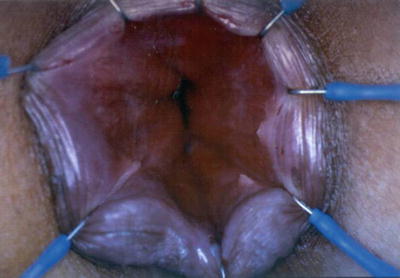

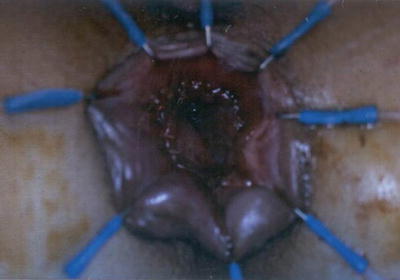
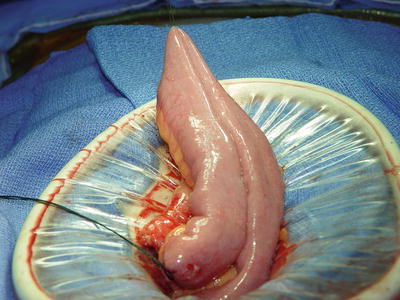
Fig. 31.9
Marking of the apex of the pouch with silk suture
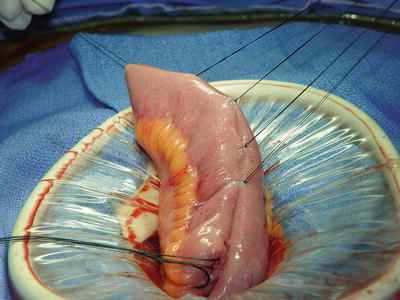
Fig. 31.10
The two loops are approximated with Lambert sutures
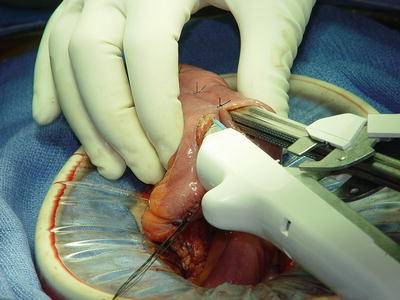
Fig. 31.11
Pouch creation: application of sequential fires of an 80-mm GIA stapler through the enterotomies
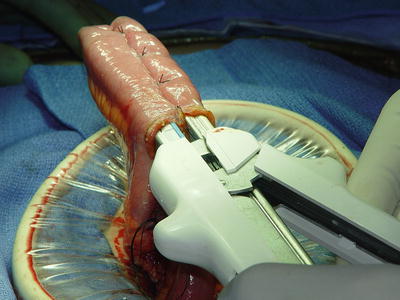
Fig. 31.12
Pouch creation: application of sequential fires of an 80-mm GIA stapler through the enterotomies
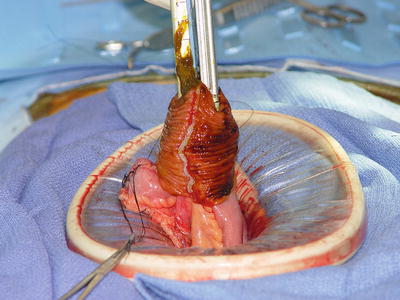
Fig. 31.13
Pouch creation: progressive eversion of the pouch as the stapler progresses toward the apex of the pouch
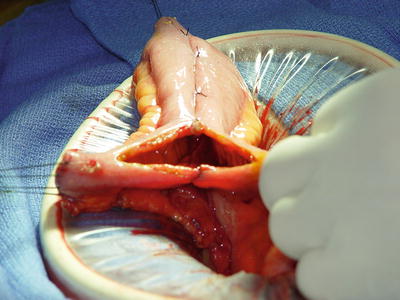
Fig. 31.14
Pouch creation: inversion of the pouch and closure of the two enterotomies
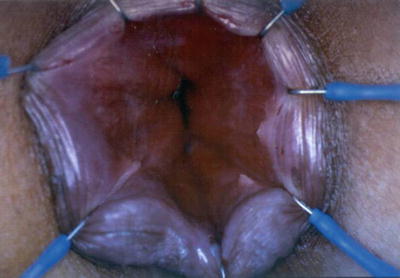
Fig. 31.15
Exposure of the anal canal for mucosectomy

Fig. 31.16
The pouch is delivered and visible at the level of the dentate line
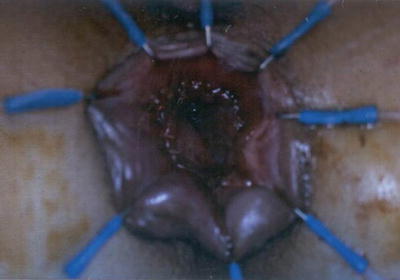
Fig. 31.17
Two-layer handsewn ileoanal pouch anastomosis
After irrigation and hemostasis in the abdomen and pelvis, a suitable loop of small bowel is identified, and a 14-French red rubber catheter is placed through the mesentery. The loop is delivered through the previously developed ileostomy site and secured in place by suturing the red rubber catheter to the skin with nonabsorbable sutures. An anti-adhesive barrier is typically used to facilitate the subsequent takedown. The Pfannenstiel incision is closed in layers and the skin is closed with subcutaneous sutures. The incision is protected and the ileostomy matured in the standard Brooke fashion with 3-0 chromic interrupted sutures (Fig. 31.18).


Fig. 31.18
Patient after completion proctectomy and IPAA
An anastomosis between the ileal pouch and anal canal performed under tension is associated with increased risk of dehiscence with severe short-term and long-term sequelae [11].
Few studies have evaluated and compared several techniques for lengthening the small bowel mesentery, including complete small bowel mobilization to the origin of its mesentery, ileocolic vessel ligation close to their origin from the superior mesenteric pedicle, and transverse mesenteric relaxing incisions [12]. These strategies facilitate a tension-free IPAA in most cases.
We have had a very limited experience with these techniques, due to the frequent staged approach to these patients. By optimizing body weight, tissue characteristics, and general medical conditions, we have almost eliminated the need for mesenteric lengthening from our practice.
For patients with extremely short mesentery, an alternative strategy has been described by Goes et al. [13]. Multiple vascular ligations are performed between the right colon wall and the marginal vascular arcade, from the right branch of the middle colic artery that is preserved and provides the only blood supply to the ileal branch of the ileocolic artery. Right colic and ileocolic arteries at their origin and the superior mesenteric trunk at its distal third are divided.
This technique presents several drawbacks: (1) it is time consuming, (2) it is technically challenging, and (3) it can lead to pouch ischemia, but it offers additional length in the extreme situations.
Total Proctocolectomy with IPAA
Step 1: Positioning of the Patient, Placement of Trocars, and Abdomen Exploration
This step is the same as for a total abdominal colectomy.
Step 2: Mobilization of the Intra-Abdominal Colon
The mobilization of the intra-abdominal colon follows the previously described steps of a total abdominal colectomy all the way to the pelvis.
Step 3: Pelvic Dissection
The monitors that were placed at the head of the table are moved to the foot of the table. The surgeon is on the patient’s right side with the assistant on the opposite side retracting the rectum up and out of the pelvis. Typically a medial to lateral approach to the mobilization of the inferior mesenteric artery is undertaken. The peritoneum overlying the sacral promontory is incised on the patient’s right side, and the left ureter is clearly identified and mobilized off the operating field. The hypogastric plexus is also identified and preserved. Only after these structures have been identified, the inferior mesenteric artery is divided and ligated with a vessel-sealing device. The level of transection of the inferior mesenteric artery and vein follows the oncologic principles in presence of colorectal cancer. The total mesorectal excision plane is then entered, and this step of the procedure follows that already described for a proctectomy.
Step 4: Construction of the Ileoanal Pouch
The IPAA construction follows the previously described steps for a proctectomy.
Single-Incision Laparoscopic Surgery (SILS)
First Stage: Total Abdominal Colectomy with End Ileostomy
Step 1: Positioning of the Patient, Placement of Trocars, and Abdomen Exploration
The positioning of the patient is the same as previously described for the other procedures.
The access to the peritoneal cavity is obtained by inserting a GelPOINT® Advanced Access Platform (Applied Medical, Rancho Santa Margarita, CA) through a circular incision at the future ileostomy site in the right lower quadrant. The GelSeal® cap provides additional working space and the ability to achieve triangulation with the instruments. One 12-mm and three 5-mm trocars are introduced through the gel platform (Fig. 31.19). The procedure is performed with conventional laparoscopic instruments, including a 12-mm 30° laparoscope and a 5-mm bipolar vessel-sealing device for tissue dissection and vascular resection. The Trendelenburg and side-to-side tilt positions dynamically vary during the procedure for optimal surgical field exposure [14].