Fig. 15.1
Ischemic ostomy. Courtesy of Philip Y. Pearson, MD, with permission
Parastomal hernia remains an especially significant problem following stoma creation (Fig. 15.2). In fact, the creation of a defect in the abdominal wall for a stoma by definition places a weakness in the abdominal wall where there once was complete continuity. Associated complications may be relatively minor, such as skin breakdown near the stoma site or difficulty fitting an appliance around the stoma, or can be life-threatening such as incarcerated intestine within the hernia [4]. Although seemingly a logical approach to reduce parastomal hernia, Level I evidence in support of prophylactic mesh placement at the time of open stoma construction is limited and comprised various types of mesh, placed in different abdominal positions [13–18]. A meta-analysis evaluating three of these studies included 128 patients and demonstrated a statistically significant reduction of parastomal hernia incidence between the mesh group (12.5 %) compared with the control group (53 %) without a difference in mesh-related morbidity. Beck et al. presented a prospective, randomized, controlled third-party blinded study of 113 patients comparing mesh inlay for parastomal reinforcement in patients undergoing surgery for permanent abdominal wall ostomies to standard end stomal construction at the 2013 American Society of Colon and Rectum Surgeons meeting [19]. Although reinforcement was found to be safe, the incidence of parastomal hernia formation was not statistically lower after 24-month follow-up [16]. However, studies evaluating prophylactic mesh placement in laparoscopically created stomas are extremely limited, with initial experiences demonstrating safety and feasibility and potentially favorable outcomes [17, 18]. Solid evidence for prophylactic placement of mesh in laparoscopic stoma construction is not yet available.


Fig. 15.2
Parastomal hernia. Courtesy of Peter Cataldo, MD, with permission
Preoperative Planning
In the elective setting, preoperative stoma site selection and marking is essential. A stoma located incorrectly predisposes the patient to problems that cannot be managed conservatively (i.e., with changes in the stoma equipment). Since body habitus varies greatly between individuals, the ideal stoma site(s) must be modified, avoiding scars and skin creases [4].
To ensure skin folds do not interfere with appliance fitting, site selection should be done in supine, sitting, and bending positions, with attention also given to the individual’s beltline [4]. The usual site in an average individual is on the apex of the subumbilical fat roll, in either the right or left iliac fossa (Fig. 15.3) [20]. Finally, the patient needs to be able to visualize the stoma in order to care for it.


Fig. 15.3
Stoma position marked on the abdomen
Operating Room Setup and Patient Positioning
Two video monitors are placed angling toward the patient at the shoulder level if constructing an ileostomy and placed toward the foot of the bed or the patient’s knees if planning a sigmoid/descending colostomy. The procedure is performed with the patient in the supine position although a modified lithotomy position is also acceptable. If the latter position is utilized, the hips and knees are gently flexed to an angle no greater than 15° to avoid the patient’s thighs interfering with the laparoscopic instruments. If an ileostomy is planned, the left arm is tucked to the side, and the surgeon stands on the left side of the patient or between the patient’s legs (Fig. 15.4). If a sigmoid/descending colostomy is planned, the right arm is tucked, and the surgeon stands on the patient’s right or between the legs. The site of peritoneal access is dependent upon the type of stoma being created and the patient’s prior surgical history. For patients with prior abdominal surgery, accessing a “free” quadrant is usually the safest approach. After intra-abdominal access is obtained, the patient is placed in Trendelenburg position to augment visualization.


Fig. 15.4
Room setup demonstrating monitor sites
Technique: Laparoscopic Ileostomy [1, 2, 4, 20]
Variations in multi-port placement positioning and sequence have been described; however, most approaches use 2 or 3 ports, taking advantage of the principle of trocar triangulation to facilitate exposure and mobilization. The first trocar inserted is a 5-mm cannula placed just inferior to the umbilicus. Once 15-mmHg pneumoperitoneum is established, a (30°) laparoscope is inserted to inspect the abdomen and direct the remaining port positions (Fig. 15.5). The patient is placed right side up in Trendelenburg position. The surgeon can visually ensure that the planned ostomy site is suitable and free of adhesions.
Fig. 15.5
Ileostomy and port sites
If the previously selected right iliac fossa stoma site is acceptable, a 12-mm port is then placed after making a 2.5-cm incision at the predetermined stoma site, excising the skin and subcutaneous fat as a cone of tissue down to the anterior rectus sheath and then dividing the sheath in a cruciate fashion. The fibers of the rectus muscle are then split longitudinally by opening an instrument perpendicular to the line of the fibers. This procedure results in little or no bleeding unless the deep inferior epigastric vessels are encountered and divided deep to the rectus muscle. After the rectus muscle is split, the posterior rectus sheath is incised to accommodate the 12-mm trocar. The 12-mm trocar provides the ability to accommodate a laparoscopic stapler for intracorporeal division if creating an end ileostomy, rather than exteriorizing the intestines for extracorporeal division. If the ileum requires further mobilization not possible with a single working port, additional 5-mm trocar(s) may be placed either in the left lower quadrant, lateral to the rectus muscle and above the pelvic brim, or suprapubically.
The terminal ileum is located, and a point on the small bowel about 15–20 cm proximal to the ileocecal valve is identified laparoscopically. Visualization of the ligament of Treves, located on the antimesenteric border of the terminal ileum just proximal to the ileocecal valve, is also helpful in identifying the anatomy (Fig. 15.6). The terminal ileum is inspected for any pathology as well as length of mesentery available for loop stoma creation. The terminal ileum is usually supplied by two arcades of vessels, which join the ileocolic vessels adjacent to the cecum. These arcades must be divided as close to the ileocolic vessels as possible to preserve blood supply to the terminal ileum.
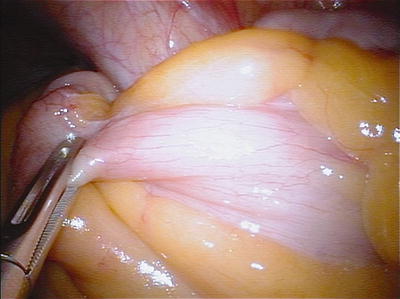
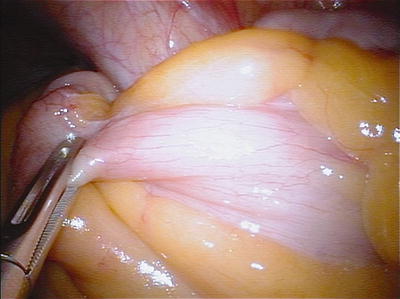
Fig. 15.6
Terminal ileum with fold of Treves visible
The proximal side (1 serosal thermal burn) and distal side (3 serosal thermal burns) of the selected point on the small bowel are marked by using laparoscopic electrocautery. Alternatively, the future ileostomy site may be marked with different colored sutures for orientation. Once mobilized, the ileum can be grasped and divided with a laparoscopic stapler through the 12-mm port and brought through the abdominal wall or exteriorized through the fascial defect and divided extracorporeally (for an end stoma). If constructing a loop ileostomy, the ileum is grasped and brought through the fascia with attention to maintaining proper orientation. To exteriorize the ileum in both cases, the fascial defect within the posterior rectus sheath must be opened and enlarged over the trocar. Because the ascending colon usually tethers the ileocolic vessels to the right lower quadrant, optimal positioning of the stoma requires the placement of the proximal end along the inferior aspect of the stoma site in a loop ileostomy.
The ileostomy is then matured in the usual fashion (Fig. 15.7). The surgeon places an index finger both along the side of the stoma down to the fascia as well as into the stoma itself and beneath the peritoneum to ensure the fascial opening is not excessively tight and the stoma is not angulated.


Fig. 15.7
Completed stoma
For single-port laparoscopic ileostomy construction, a 2.5-cm incision is made in the right iliac fossa at the predetermined stoma site (Video 15.1). The incision is carried down to the anterior rectus sheath, which is then divided in a cruciate fashion. The skin and subcutaneous fat are excised as a cone of tissue down to the anterior rectus sheath (Fig. 15.8). The rectus abdominis muscle is spread in the direction of its fibers exposing the posterior rectus sheath and peritoneum, which are then divided in a cruciate fashion over a distance of 2.5 cm, wide enough to accommodate 2 fingers (Fig. 15.9).
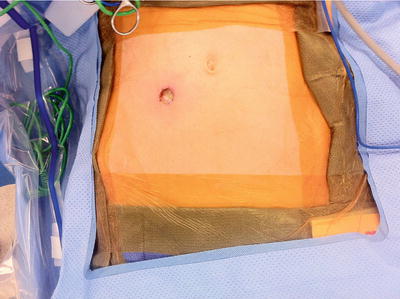

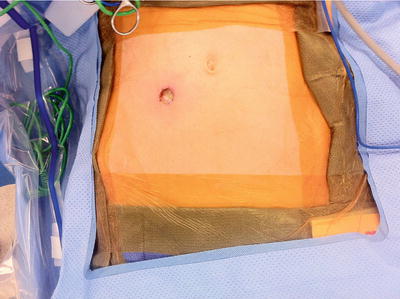
Fig. 15.8
Anterior sheath

Fig. 15.9
Posterior sheath: dissection down through the subcutaneous tissue, anterior rectus sheath, and rectus muscle, exposing the posterior rectus sheath
The single-port access system is then inserted through this incision (Figs. 15.10 and 15.11). The abdomen is insufflated with CO2 to 15 mmHg. A 5-mm laparoscope with a flexible steerable tip is used to visualize the abdomen. Single-incision laparoscopic instruments may be used, but standard laparoscopic instruments are suitable in most cases.










