Fig. 32.1
Patients can also be prepped circumferentially from nipples to toes and draped by passing the lower half of the baby through an adult extremity drape
The use of an adult extremity drape for circumferential lower body draping is demonstrated. This technique is useful when access to the perineum is required for laparoscopically assisted endorectal pull-through operations for Hirschsprung’s disease or imperforate anus in small children and neonates (Fig. 32.1).
Trocar Selection and Insertion Technique
The technology void created by the growth of pediatric laparoscopy was quickly filled by manufacturers as the demand for customized pediatric trocars, instrumentation, and energy devices grew. Appropriate trocar selection, placement, and insertion technique will avoid frustration associated with poor ergonomics, visibility, and longer operative times. Abdominal access techniques and pneumoperitoneum are achieved in a somewhat similar manner as in adult patients, with several notable caveats.
Most children (and many adults) have at least a small fascial opening at the base of the umbilicus which allows a very safe method for accessing the abdomen. The umbilicus is often not nearly as deep as in larger patients, and the authors usually perform a direct vertical skin incision at the very base of the umbilicus. A hemostat can then usually be placed directly into the peritoneum and subsequently replaced by the first trocar. This often takes less than 20 s. The traditional open Hassan technique can be useful in larger patients as well. The abdominal wall is significantly thinner and more compliant in neonates, toddlers, and young children compared to adolescents and adults. Due to the increased pliability of the abdominal wall, and especially without pneumoperitoneum established, optical entry techniques like the Visiport™, Covidien, Mansfield, MA, should typically be avoided. The insertion technique for the remaining trocars often requires a gentle “pop” in the proper direction as opposed to steady pressure, as it takes surprisingly little effort to push the abdominal wall flush against the retroperitoneum in smaller children, even with appropriate pneumoperitoneum. In fact, trocar insertion proves to be responsible for most catastrophic complications in pediatric MIS with an incidence of great vessel injury of only 0.05 %, but with an associated mortality of 20 % [4].
The bladder can often be emptied by manual lower abdominal compression (the Credé maneuver) in younger children prior to short procedures. Intraoperative Foley catheter drainage can be used for long cases and discontinued at the end of the procedure or in the early postoperative period. The Foley is often continued for 1 week after dividing a rectourethral fistula during laparoscopic imperforate anus repair in male infants prior to obtaining a voiding cystourethrogram (VCUG).
The abdominal wall of many pediatric patients is quite thin. This has both advantages and disadvantages. Transillumination of the abdominal wall during trocar placement can be quite helpful in avoiding blood vessels. Many trocars, however, are designed to capture or hold the abdominal wall in several different manners; these trocars work better when the abdominal wall is thicker. One such trocar used by many pediatric surgeons in larger patients or in the umbilicus is the radially expanding Step™ trocar (Covidien, Mansfield, MA). The device comes in lengths of 75 and 100 mm and has an expandable sleeve that starts at a diameter of 1.7 mm and is inserted with a Veress needle. Other trocars have plastic ribbing to grip the abdominal wall or balloons which can be insufflated and pulled back against the abdominal wall. However, these trocars do not perform as well in infants and smaller pediatric patients. The balloons may take up too much of the short distance between the trocar and the operative target. Other trocars don’t grip the abdominal wall very well and have a tendency to slide out or become dislodged, especially when exchanging instruments. Therefore, the authors most often use reusable 2.7- and 3.5-mm trocars manufactured by Karl Storz (Tuttlingen, Germany), fitted with a short piece of 14-Fr catheter placed around the trocar at an appropriate (and adjustable) interval from the trocar exit as demonstrated in Fig. 32.2. This allows quite precise placement of the proper amount of intra-abdominal trocar length and allows the surgeon to suture the catheter to the skin to prevent unwanted movement. These trocars also have small heads which prevent them from colliding during instrument manipulation in an already crowded working environment.


Fig. 32.2
The Step™, radially expanding umbilical trocar, and the 3.5- and 2.7-mm reusable trocars are shown anchored to the skin with silk sutures tied to the clear, 14-Fr catheter used as a sleeve over the shaft of the trocar
Most surgeons do not close the fascial defect created by 5-mm trocars in adult patients. However, 5-mm port sites are at higher risk of trocar site herniation in children and are preferentially closed in pediatric patients [5, 6]. The use of stab incisions rather than traditional trocars for inserting laparoscopic instruments directly through the chest or abdominal wall is another maneuver used by some in pediatric MIS [7]. The authors use this technique for laparoscopic pyloromyotomy where instruments need to be changed out infrequently. We prefer small trocars for more complex operations that may require frequent exchanging of instrumentation, as it seems less traumatic to the abdominal wall.
Pearls and Pitfalls
The abdominal wall is very pliable in children, and extra care needs to be taken to avoid trocar injury to retroperitoneal structures.
To avoid frustration with trocar displacement, choose trocars that can be secured well to the thin abdominal wall in children.
Gas Insufflation
We know that pneumoperitoneum has the potential to cause pronounced physiologic changes in pediatric patients that can lead to complications. For instance, insufflation may cause an increase in end-tidal CO2, cephalad displacement of the diaphragm, reduced pulmonary compliance, and increased airway resistance, which can be remedied by increasing the minute ventilation. Also, lower intra-abdominal pressures (IAP) of <10 mmHg increase venous return, leading to increased cardiac output and a 20–25 % increase in arterial pressures. On the other hand, if IAP is increased to 20 mmHg, the inferior vena cava becomes compressed, resulting in decreased venous return, decreased cardiac output, and decreased renal blood flow. Most children can tolerate an IAP of 15 mmHg during laparoscopy, but neonates less than 5 kg should be limited to pressures of 10–12 mmHg [8]. The authors prefer to select insufflation pressures based on patient size depicted in Table 32.1. Some insufflators may be too insensitive to the rapid pressure changes within the abdomen and may inadvertently result in over insufflation. Although attempts have been made to design pediatric insufflators that administer less volume or use a lower flow rate, we have not yet found one to be equivalent to the standard insufflators available.
Table 32.1
Recommended pressure selection according to patient size in order to accomplish safe pneumoperitoneum in infants and young children during insufflation
Patient size (kg) | Pressure of pneumoperitoneum (mmHg) |
|---|---|
<5 | 10 |
5–10 | 12 |
>10 | 15 |
Pediatric Laparoscopic Instrumentation
Adult MIS instruments are frequently too long (32–36 cm) and too large in diameter (5–10 mm) for younger children, and especially neonates. Using adult-length instruments on small children may leave as much as 80 % of the instrument outside the patient which may lead to poor ergonomics, awkward manipulation, and imprecise movements. Ideally, two-thirds of an endoscopic instrument should be inside the body cavity with the other one-third outside the body to prevent motion parallax. In general, pediatric laparoscopic instrumentation has finer tips and the instruments come in varying lengths. The authors keep instruments in different sets based on patient size. Our infant tray generally has 2.7-mm instruments that are 20 cm in length. The adolescent tray has 5-mm instruments that are 30 cm. Our pediatric tray has a mixture of instruments ranging from 2.7 to 5 mm in diameter and from 25 to 30 cm in length. We similarly use a range of 0° and angled lens laparoscopes, ranging from a 20-cm, 2.7-mm-diameter scope to standard length 5-mm scopes. A small 70° scope is useful for performing contralateral inguinal exploration during inguinal hernia repair as well [9].
There are also multiple energy devices available for use in pediatric laparoscopy. Prior use and familiarity with any given energy device may be the best guide to follow when choosing instrumentation for a surgery, but it remains important to keep the active portion of the instrument visible on the screen and to use the lowest effective settings to avoid collateral damage and arcing potential.
Hand position is crucial when operating on smaller patients. Many pediatric surgeons operate when using trigger-handle instruments with their left hand inverted. The authors routinely do this, especially when operating on neonates as shown in Fig. 32.3. This allows a greater distance between the hand of the surgeon and that of the assistant in tight spaces. We prefer intracorporeal suturing and knot tying in order to use 2.7-mm instruments as opposed to automated devices such as the Endo Stitch™ by Covidien, which all require at least 5-mm ports. We manually bend or flatten small needles that are appropriate in size for the patient. We prefer an in-line, ring handle laparoscopic needle driver manufactured by Jarit (Integra, Plainfield, New Jersey).
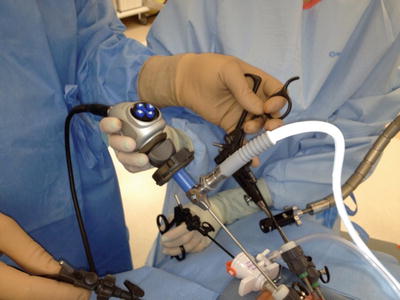
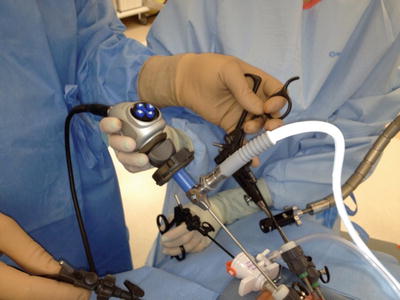
Fig. 32.3
The surgeon is demonstrating the inverted, left hand technique with a standard trigger-handle laparoscopic instrument to allow enough space for the assistant’s hands during instrument manipulation
The initial hesitancy to accept pediatric laparoscopy as a safe and effective surgical technique has quickly faded, and now, the question has changed from not whether minimally invasive surgery should be done for young children and infants, but for which conditions? As an example, thoracoscopic repair of infants with congenital diaphragm hernia has become a widespread technique, but recent data comparing it to standard open approaches show that the recurrence rate for thoracoscopic repair is unacceptably high.
The following sections will discuss a select number of pediatric colorectal diseases and our preferred therapeutic approach with minimally invasive techniques. Although certain diseases like Hirschsprung’s disease and imperforate anus are fairly specific to pediatric surgery, the techniques described certainly translate to a number of adult colorectal diseases and disorders.
Appendicitis
Clinical Presentation and Indications
Appendicitis remains the most common surgical illness in children that is treated by both pediatric and adult general surgeons. It has an incidence of 70,000 pediatric cases per year with the highest rates occurring at 25 cases per 10,000 children per year between 10 and 17 years of age. Diagnosing acute appendicitis in children is very similar and perhaps more straightforward than in adults. A history of migrating abdominal pain in association with physical findings and leukocytosis remain accurate diagnostic clues for children and adults. For instance, migrating abdominal pain for acute appendicitis has a positive predictive value (PPV) of 94.2 % in children and 89.6 % in adults [10]. In the absence of classic signs and symptoms, diagnostic imaging can be a helpful adjunct. Given the increased awareness and risk of radiation exposure in children, ultrasound is usually the preferred modality, although certain clinical situations require CT imaging as well.
Surgical Technique: Laparoscopic Appendectomy
Most commonly, pediatric laparoscopic appendectomy in the United States is performed through a three-port technique. We prefer to place a 12-mm port at the umbilicus and two additional working ports that range from 2.7 to 5 mm based on patient size. One is placed in the left lateral abdomen and another in the suprapubic region. In very small patients, the suprapubic port may be placed very low in the left lower abdomen to increase the distance between the trocar and the appendix. The surgeon stands to the left of the patient with the assistant initially on the patient’s right. After trocar placement, the assistant moves to the patient’s left as well in order to hold and manipulate the camera in-line with the working field. We prefer to use small graspers to sweep the bowel away from the operative field, taking care to avoid grasping and potentially injuring the bowel. We also avoid grasping the appendix where it is inflamed or visibly friable, grasping only the relatively healthy portion. Occasionally, a long Debakey grasper is needed for a very thick, inflamed appendix. We divide the mesoappendix with hook electrocautery regardless of patient size. Although residual bleeding is quite rare, a Maryland dissector can be used to grasp the area of concern to apply additional electrocautery. Other surgeons prefer various vessel-sealing devices for the mesoappendix such as the LigaSure™ (Covidien, Norwalk, CT) or Harmonic Scalpel (Ethicon, Cincinnati, OH), but we feel the added cost is unnecessary. Some surgeons also utilize an endostapler to control the mesoappendix, which often yields less than satisfactory results when there is significant inflammation. We prefer to use a 35-mm stapler with 2.5-mm staples to divide the appendix at its junction with the cecum. A cost-efficient, safe, and effective method has been validated using only electrocautery with a hook or Maryland dissector to divide the mesoappendix and three 0-PDS Endoloops (Ethicon Endo-Surgery, Cincinnati, OH) to ligate the base of the appendix with two proximal and one distal [11]. Although this gives the added advantage of a smaller 5-mm umbilical incision (the 12-mm incision is needed for the stapler), application of the Endoloops can be tedious and there can be a small amount of contamination when dividing an appendix with acute inflammation at the cecal junction. Furthermore, the appendix can usually be pulled out through the 12-mm trocar without needing a specimen retrieval bag.
Several early studies comparing open versus laparoscopic appendectomy were conflicted and resulted in little consensus among pediatric surgeons regarding the best operative approach. Other more recent studies suggest that laparoscopic appendectomy, in appropriately selected patients, can result in fewer postoperative complications. The rate of superficial wound infection is clearly reduced with laparoscopic appendectomy and patients may have slightly earlier discharge from the hospital [12–14]. Some earlier reports suggested that children with perforated appendicitis that underwent laparoscopic appendectomy had higher rates of abscess formation [15]. However, a recent study by Nadler and colleagues reported no difference in infectious complications and a lower overall rate of perioperative complications in their patients with perforated appendicitis treated with laparoscopy [16]. Pediatric subspecialty training also seems to have little impact on surgical outcomes with regard to readmission, wound infection, intra-abdominal infection, or mean hospital stay for appendicitis when compared against adult general surgeons and their outcomes [17]. These findings could be explained by the fact that laparoscopic appendectomy technique is similar across age groups, and most general surgeons are high-volume surgeons for adult appendectomy, even if they are low-volume for pediatric appendectomy.
Pearls and Pitfalls
Avoid grasping the appendix where it is very inflamed or gangrenous to avoid intraoperative rupture.
In difficult cases, carefully mobilizing the cecum medially and off of the retroperitoneum can help discern the anatomy.
Inflammatory Bowel Disease
Clinical Presentation and Indications
There is an increasing frequency of inflammatory bowel diseases (IBD) such as ulcerative colitis (UC), Crohn’s disease (CD), and indeterminate colitis (IC) in both pediatric and adult populations [18]. Ulcerative colitis and IC are most frequently diagnosed in children between the ages of 3 and 5, while CD increases during the adolescent years, peaking at 15 years of age. Pediatric surgeons become involved as the disease worsens and becomes refractory to medical management or when complications arise. The peak incidence of IBD occurs between the ages of 15 and 25 years, or a time when adolescents and young adults may traverse both pediatric and adult hospital settings when seeking surgical consultation [18]. Interestingly, a study by Jan et al. revealed that both hospital type and surgeon specialty within hospital type influenced the likelihood of surgical complications among adolescents and young adults with IBD requiring surgical intervention [19]. Despite higher complications among children’s hospitals, pediatric surgeons had the lowest predicated probabilities of surgical complication or 30-day readmission (24 %) compared with general surgeons (39 %) and colorectal surgeons (35 %). The lifetime risk of surgery for IBD complications, such as extraintestinal manifestations, bowel obstruction, enteric fistulas, abscess formation, toxic megacolon, or massive hemorrhage, ranges from 40 to 70 % with a surgical complication rate of 13–55 % [20–24]. Other surgical indications unique to the pediatric population include more chronic symptoms such as delayed puberty or growth retardation as demonstrated by a failure to follow normal growth curves.
Surgical Technique
Laparoscopic ileocecectomy for irreversible obstruction of the terminal ileum in patients with Crohn’s disease can be performed through a four-trocar approach. A stapled intracorporeal or extracorporeal anastomosis can be performed through an enlarged right lower quadrant port incision depending on preference. We prefer extracorporeal anastomosis. Ileocecal resection for Crohn’s disease is much less common in the pediatric population, but the adult experience has demonstrated this to be a safe technique with obvious cosmetic advantages, shorter length of stay, and fewer complications [25–27]. Therefore, additional instruction regarding operative technique will be deferred to the discussion found elsewhere in this text.
Surgery remains the definitive cure for patients with ulcerative colitis after failure of medical management or neoplastic degeneration. There are several notable differences in the surgical techniques that are usually applied to the pediatric patient. Patients usually undergo either a two-stage or a three-stage approach, depending on their clinical condition at the time of total abdominal colectomy. If patients are critically ill with toxic megacolon or on high-dose steroids, completion proctectomy and J-pouch creation are performed later in a staged approach with end ileostomy done at the time of the total abdominal colectomy. In patients who can tolerate it, we perform this laparoscopically in a manner quite similar to the adult operation (See Chap. 13). Although the specimen can be removed through the eventual ileostomy site, the specimen is often friable and dilated. The authors prefer to avoid making the ileostomy site incision any larger than required and alternatively use a relatively small transverse suprapubic incision for removal of the colectomy specimen.
The most notable disparity between typical adult and pediatric techniques involves the dissection and approach on the perineum. The ileal pouch-anal anastomosis (IPAA) is now commonly performed with a very low (end-to-end) EEA-stapled anastomosis in adults. This operation evolved after studies discovered that up to 50 % of patients undergoing endorectal mucosa resection and hand-sewn IPAA were left with early postoperative nighttime stool incontinence [28]. Despite preserving the richly innervated anal transition zone (ATZ), stapled IPAA has been shown to confer no early advantage with regard to decreased stool frequency or fewer episodes of fecal incontinence compared to hand-sewn IPAA [29]. Despite the results of a large meta-analysis that suggested stapled IPAA offered improved early nocturnal continence with coinciding higher anorectal resting and squeeze pressures, both procedures are acceptable with different benefits [30]. The stapled technique leaves several centimeters of anorectal mucosa at risk for the development of ulcerative colitis, polyposis, and in the long run, dysplastic conversion and malignant degeneration. Most practitioners recommend routine endoscopic surveillance for this cuff. Since most pediatric patients have significantly greater life expectancy, tedious surveillance of this at-risk mucosa can be avoided by performing a mucosectomy with a hand-sewn ileoanal anastomosis, with a reduced risk of eventual malignancy given that the life expectancy for these patients is longer.
A trans-abdominal low-anterior dissection of the rectum can be performed laparoscopically or via the small transverse suprapubic incision followed by the transanal mucosectomy on the perineum. For the mucosectomy, a circumferential incision is made just above the dentate line (Fig. 32.4), and multiple sutures are placed in this mucosal sleeve circumferentially to provide traction (Fig. 32.5). Pop-off sutures are preferred due to their ease of use and identical length. A Colorado needle-tip Bovie electrocautery is then used to dissect the muscularis layer proximally off of the mucosal sleeve (Fig. 32.6). At first, the plane can be somewhat difficult to create, but this often becomes easier and more apparent as the dissection is carried proximally. If the dissection becomes too facile at this stage, the surgeon may have inadvertently created a full-thickness dissection instead of remaining in the submucosal plane. If any defects are created in the mucosal tube, sutures are placed to repair them. Unfortunately, this may plicate the mucosa, making it more difficult to get back into the right plane as the proximal dissection continues. Fine, cotton-tipped swabs can be used as pushers to help create the plane as well, although small bleeding vessels will require electrocautery.
Fig. 32.4
Mucosal incisions 5–10 mm above the pectinate or dentate line (Courtesy of Keith Georgeson, MD, with permission)
Fig. 32.5
Rectum and colon pulled down in continuity, bringing transition zone through the anus (Courtesy of Keith Georgeson, with permission)