Fig. 5.1
A linear endoscopic probe (a, top; b) is typically used as the initial diagnostic tool to evaluate the upper gastrointestinal (GI) tract. A linear endoscopic ultrasound (EUS) scope (a, middle) and radial ultrasound scope (a, bottom) are used to visualize structures in the wall of the esophagus
This assessment serves to guide the biopsy of the lesion in question and esophageal brushings, which are performed through the linear echoendoscope. These instruments also have a role in management, as tumors of early cancer (T1a or below) are amenable to endoscopic ablative therapy, submucosal dissection, and endoscopic mucosal resection (EMR).
Tumors Amenable to Endoscopic Treatment
In the classification of esophageal tumors [1], T1a cancers, with a known 5–7 % chance of harboring lymphatic spread of tumor, are considered amenable to endoluminal therapy. On the other hand, T1b lesions, which have spread to the submucosa or beyond, have a 15–20 % chance of nodal involvement. These tumors are not amenable to endoluminal therapy [2].
Setting Up the Ultrasound Probe
The scope itself is larger than the linear probe. A balloon is placed on the tip using a plastic installing device (Fig. 5.2a). Before the probe is introduced into the patient, the balloon is insufflated with saline (Fig. 5.2b), and any air is expelled to allow a clear probe-tissue interface.
Fig. 5.2
The EUS scope is typically set up with a balloon, using a loading device (a) at the terminal end of the scope. All air is expelled from the balloon before it is inflated with water (b) to allow a scope-tissue interface to optimally assess the layers of the esophagus—the mucosa, submucosa, muscle layer
Technique
Assessment
Step 1. Visualize abnormalities
A regular endoscope is used to first visualize the tumor and any other associated esophageal and gastric wall abnormalities. Distance from the incisors, total tumor length, and length of any Barrett’s esophagus is noted by the endoscopist. The pylorus is investigated and intubated to visualize the duodenum.
Step 2. Assess the tumor
The radial probe is then advanced into the esophagus to the most proximal extent of the tumor as measured from the incisors previously. Tumor depth is then measured to define the T-stage
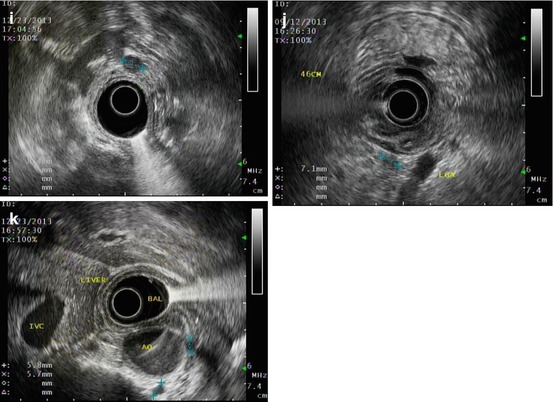
The ultrasound probe is positioned for universal interpretation (Fig. 5.3a, b):
Left atrium anteriorly
Aorta at 5 o’clock position
Azygos vein and left gastric artery posteriorly
Look for the thoracic duct between the aorta and azygos vein
Once the tumor is visualized on the monitor, the balloon is insufflated. All the layers of the esophageal wall are then seen (Fig. 5.3c, d). Any abnormal wall thickening should be documented. The T-stage of the tumor should be determined by adjusting the depth on the monitor (Fig. 5.3e). Invasion into neighboring structures also can be determined (Fig. 5.3f).